Decoding Viral Evolution: A Comprehensive Guide to NGS for Mutation Rate Analysis in Drug Discovery and Clinical Research
Next-generation sequencing (NGS) has revolutionized the tracking and analysis of viral mutation rates, becoming an indispensable tool for researchers and drug development professionals. This article provides a comprehensive exploration of how NGS technologies are applied to understand viral evolution, from fundamental principles to advanced clinical applications. We cover the critical methodological approaches for detecting mutations, including strategies for optimizing accuracy and sensitivity to identify low-frequency variants. The content further delves into troubleshooting common challenges, comparing sequencing platforms, and establishing robust validation frameworks. By synthesizing current methodologies and their practical implementations in monitoring antiviral resistance and guiding therapeutic development, this guide serves as an essential resource for advancing viral genomics research and precision medicine.
Decoding Viral Evolution: A Comprehensive Guide to NGS for Mutation Rate Analysis in Drug Discovery and Clinical Research
Abstract
Next-generation sequencing (NGS) has revolutionized the tracking and analysis of viral mutation rates, becoming an indispensable tool for researchers and drug development professionals. This article provides a comprehensive exploration of how NGS technologies are applied to understand viral evolution, from fundamental principles to advanced clinical applications. We cover the critical methodological approaches for detecting mutations, including strategies for optimizing accuracy and sensitivity to identify low-frequency variants. The content further delves into troubleshooting common challenges, comparing sequencing platforms, and establishing robust validation frameworks. By synthesizing current methodologies and their practical implementations in monitoring antiviral resistance and guiding therapeutic development, this guide serves as an essential resource for advancing viral genomics research and precision medicine.
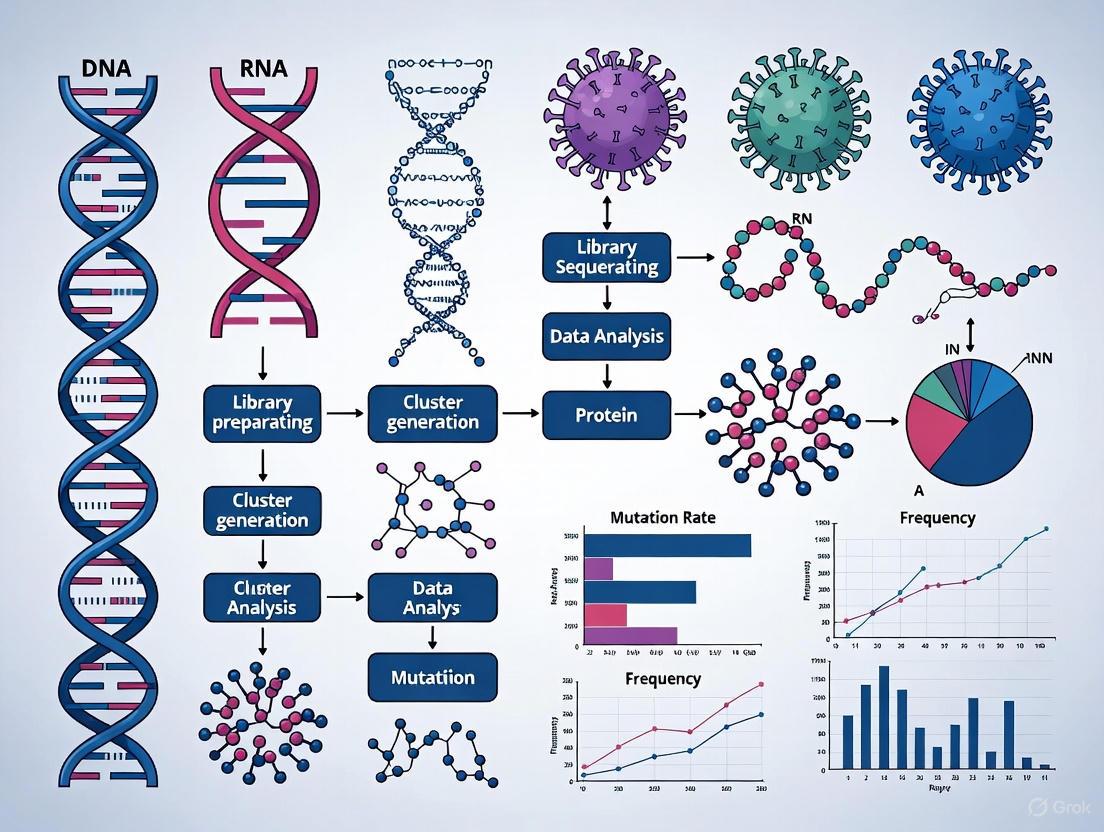
Viral Mutation Fundamentals: From Molecular Mechanisms to NGS Detection Principles
The study of viral mutation rates is a cornerstone of virology, with profound implications for understanding viral evolution, pathogenesis, and the development of effective countermeasures. Next-generation sequencing (NGS) has revolutionized this field by providing unprecedented resolution to detect and quantify genetic variations within viral populations. The mutational landscape of viruses is not merely an academic curiosity; it directly impacts pandemic preparedness, vaccine design, and therapeutic development. This application note examines the distinct mutational profiles of DNA and RNA viruses, with a specific focus on insights gained through advanced NGS methodologies. We present standardized protocols for mutation rate quantification, detailed experimental designs for comparative studies, and key reagent solutions to support research in this critical area.
Quantitative Comparison of Viral Mutation Rates
Data compiled from recent studies utilizing NGS methodologies reveal significant differences in mutation rates between RNA viruses and between RNA and DNA viruses. These quantitative measurements provide a foundation for understanding viral evolution and adaptive potential.
Table 1: Comparative Mutation Rates of Viruses Measured by NGS Approaches
| Virus | Genome Type | Mutation Rate (substitutions/site/passage) | Mutation Spectrum Bias | Primary NGS Method | Reference |
|---|---|---|---|---|---|
| SARS-CoV-2 | +ssRNA | ~1.5 × 10â»â¶ [1] | Dominated by C→U transitions [1] | CirSeq [1] | |
| SARS-CoV-2 | +ssRNA | 3.76 × 10â»â¶ [2] | Mostly transitions [2] | RT-PCR Cloning & Sanger Sequencing [2] | |
| Influenza A Virus (IAV) | -ssRNA | 9.01 × 10â»âµ [2] | Similar transitions/transversions [2] | RT-PCR Cloning & Sanger Sequencing [2] | |
| Poliovirus | +ssRNA | ~1 × 10â»âµ [1] | Not Specified | CirSeq [1] |
The data in Table 1 highlight a critical finding: the presence of a proofreading mechanism can profoundly alter the mutational landscape of an RNA virus. SARS-CoV-2, which possesses a proofreading 3′-to-5′ exoribonuclease activity in its nsp14 protein [2] [3], exhibits a mutation rate approximately 23.9-fold lower than that of Influenza A Virus, which lacks such a repair system [2]. This difference underscores why mutation rates can vary significantly even within the same broad category of RNA viruses.
Experimental Protocols for Mutation Rate Determination
Accurate determination of mutation rates relies on robust experimental designs and precise sequencing protocols. Below, we detail two key methodologies applied in recent viral studies.
Protocol 1: Circular RNA Consensus Sequencing (CirSeq) for High-Fidelity Mutation Detection
Application: This protocol is designed for the ultra-sensitive detection of spontaneous mutations in viral RNA genomes, minimizing sequencing errors to reveal the true mutational landscape [1] [4].
Workflow Overview: The following diagram illustrates the key steps in the CirSeq protocol, from RNA sample preparation to final mutation calling:
Procedure:
- Viral RNA Fragmentation: Purify viral RNA and fragment it into short pieces (~200-400 nucleotides) using controlled hydrolysis or enzymatic methods [1].
- RNA Circularization: Circulate the fragmented RNA molecules using RNA ligase. This step creates a template for generating tandem repeats during the subsequent reverse transcription [1] [4].
- cDNA Synthesis and Amplification: Perform reverse transcription on the circularized RNA. The polymerase circles the template, generating a complementary DNA (cDNA) molecule containing long tandem repeats of the original sequence. Amplify this cDNA for sequencing [1].
- NGS Library Prep and Sequencing: Prepare a sequencing library from the amplified cDNA and sequence it using a high-throughput NGS platform (e.g., Illumina) [1] [5].
- Consensus Building and Mutation Calling: Bioinformatically process the sequencing reads. Align the tandem repeats from each original RNA molecule to generate a high-accuracy consensus sequence, effectively eliminating errors introduced during reverse transcription and sequencing. Compare these consensus sequences to the reference genome to identify true mutations [1] [4].
Protocol 2: Serial Passaging and Targeted Gene Analysis
Application: This method is used for direct comparative measurement of mutation rates between different viruses under controlled cell culture conditions, often focusing on specific genes of interest like surface glycoproteins [2].
Workflow Overview: The logical flow of the serial passaging experiment is shown below:
Procedure:
- Cell Culture and Infection: Use cell lines susceptible to the viruses under study (e.g., Calu-3 human lung epithelial cells for respiratory viruses). Infect cells at a low multiplicity of infection (MOI=0.1-1) to minimize co-infection and complementation effects [1] [2].
- Serial Virus Passaging: Harvest the virus-containing culture supernatant after a fixed period (e.g., 48 hours). Use this supernatant to infect fresh cells. Repeat this process for multiple passages (e.g., 15 passages) to allow for the accumulation of mutations [2].
- Viral RNA Extraction and Gene Targeting: After the final passage, extract viral RNA from the supernatant. Use Reverse Transcription-Polymerase Chain Reaction (RT-PCR) with gene-specific primers to amplify target regions (e.g., the Spike (S) gene for SARS-CoV-2 or the Hemagglutinin (HA) and Neuraminidase (NA) genes for Influenza) [2].
- Cloning and Sequencing: Clone the RT-PCR products into plasmids. Sequence a sufficient number of clones (e.g., 20 per passage line) to detect mutations and determine their frequency [2].
- Mutation Rate Calculation: Calculate the mutation rate using the formula: Mutation Rate = (Total number of mutations / Total number of nucleotides sequenced) / Number of passages [2].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of the aforementioned protocols requires a suite of reliable reagents and tools. The following table details key solutions for viral mutation rate studies.
Table 2: Key Research Reagent Solutions for Viral Mutation Rate Studies
| Reagent / Tool | Function / Application | Specific Examples / Notes |
|---|---|---|
| Susceptible Cell Lines | Provides a permissive system for viral replication and serial passaging. | VeroE6 cells (for high viral diversity) [1]; Calu-3 (human lung adenocarcinoma, physiologically relevant) [1] [2]. |
| Ultra-Sensitive NGS Kits | Library preparation for high-fidelity sequencing. | CirSeq library prep kits [1]; Illumina sequencing-by-synthesis kits [5]. |
| Viral RNA Extraction Kits | Isolation of high-quality, intact viral RNA from culture supernatants or clinical samples. | Kits based on silica-membrane column technology or magnetic beads. |
| Reverse Transcriptase & PCR Kits | Amplification of specific viral genomic regions for cloning and sequencing. | High-fidelity RT-PCR kits to minimize polymerase-introduced errors during amplification [2]. |
| Bioinformatic Pipelines | Consensus sequence generation, variant calling, and mutation spectrum analysis. | Custom CirSeq data analysis pipelines [1]; BWA/GATK for short-read data; specialized tools for quasispecies reconstruction [4]. |
| A2 | A2, CAS:131816-87-0, MF:C21H15N5O10S2, MW:561.5 g/mol | Chemical Reagent |
| 4-Bromomethyl-1,2-dinitrobenzene | 4-Bromomethyl-1,2-dinitrobenzene, CAS:114872-53-6, MF:C7H5BrN2O4, MW:261.03 g/mol | Chemical Reagent |
Discussion and Evolutionary Implications
The empirical data generated through NGS-based protocols reveal fundamental evolutionary strategies. The high mutation rate of Influenza A virus facilitates rapid antigenic drift, allowing it to escape host immunity and necessitating annual vaccine reformulation [2] [3]. Conversely, the lower mutation rate of SARS-CoV-2, enabled by its proofreading mechanism, may be a necessary adaptation to maintain the integrity of its large (~30 kb) genome [1] [3]. However, its global spread and high replication volume provide ample opportunity for fitter variants to emerge, as observed with the Omicron lineage and its sub-lineages [6].
The biased mutation spectrum, particularly the C→U transitions dominant in SARS-CoV-2, points to specific underlying mutational processes, such as cytidine deamination, which may represent a therapeutic target [1]. Furthermore, the finding that mutation rates are reduced in regions of RNA secondary structure highlights an additional layer of genomic constraint where synonymous mutations can have significant fitness costs [1].
Next-generation sequencing has provided a refined, quantitative understanding of viral mutation rates, moving beyond broad generalizations to reveal the precise mechanisms and constraints that shape viral evolution. The protocols and reagent solutions outlined in this application note provide a framework for researchers to accurately measure and compare these critical parameters. As NGS technologies continue to advance, becoming more sensitive and accessible, their application in tracking viral evolution in near real-time will be invaluable for public health responses, drug discovery, and the design of next-generation, resilient vaccines.
The field of viral genomics has undergone a profound transformation, moving from targeted, sequence-dependent methods to an era of untargeted, high-throughput genomic surveillance. Next-generation sequencing (NGS) has emerged as a powerful tool that provides unparalleled capabilities for analyzing viral DNA and RNA molecules in a high-throughput and cost-effective manner [5]. This revolutionary technology allows researchers to sequence millions of nucleic acid fragments simultaneously, providing comprehensive insights into viral genome structure, genetic variations, and evolutionary dynamics [5].
The evolution of sequencing technologies is vividly illustrated by comparing the discovery of three major zoonotic coronaviruses. In 2002/2003, SARS-CoV-1 was identified using a combination of virus isolation, electron microscopy, serology, and partial genome sequencing via Sanger technology. A decade later, the identification of MERS-CoV in 2012 leveraged similar methods but incorporated whole genome sequencing using the Roche 454 short-read NGS platform. In 2019, SARS-CoV-2 was directly identified from patient samples using short-read mNGS with the Illumina platform, producing a complete viral genome sequence within days [7]. This progression highlights how NGS has dramatically accelerated and broadened our ability to characterize viral pathogens.
The NGS Technology Landscape
The versatility of NGS platforms has expanded the scope of viral genomics research, facilitating studies on viral evolution, outbreak investigation, and vaccine development. Various sequencing platforms offer distinct advantages depending on the specific application requirements.
Table 1: Comparison of Key Sequencing Technologies for Viral Genomics
| Technology | Read Length | Error Rate | Key Strengths | Best Applications in Virology |
|---|---|---|---|---|
| Illumina | 50-300 bp | 0.1-1.0% | High accuracy, high throughput, high sensitivity | Variant calling, genomic surveillance, low-frequency mutation detection |
| Oxford Nanopore (ONT) | Up to 1+ Mb | 1-15% | Long read length, portability, real-time sequencing | Rapid outbreak investigation, genome finishing, structural variation |
| PacBio HiFi | 10,000-25,000 bp | <1% (with circular consensus) | Long reads with high accuracy | De novo genome assembly, complex strain discrimination |
| Ion Torrent | 200-400 bp | ~1% | Fast run times, semiconductor detection | Rapid diagnostics, targeted sequencing |
NGS technologies are broadly categorized into second-generation (short-read) and third-generation (long-read) platforms. Short-read technologies like Illumina provide high accuracy and are ideal for detecting single nucleotide variants and performing quantitative analyses [7]. Long-read technologies such as Oxford Nanopore and PacBio excel at resolving complex genomic regions, detecting structural variations, and achieving complete de novo genome assemblies without the need for reference-based mapping [5] [7].
The choice between these technologies depends on the specific research goals. For comprehensive viral discovery where no prior sequence information exists, long-read sequencing provides advantages in assembling complete genomes. For sensitive detection of minor variants in a viral population, short-read sequencing offers the depth and accuracy required to identify mutations present at low frequencies [8].
Key Applications in Viral Genomics
Viral Discovery and Metagenomics
Viral metagenomic next-generation sequencing (vmNGS) has transformed our capacity for the untargeted detection and characterization of emerging zoonotic viruses, surpassing the limitations of traditional targeted diagnostics [7]. This sequence-independent approach enables detection without prior genetic information, making it invaluable for outbreak investigations of unknown etiology.
vmNGS supports comprehensive viral genome surveillance, enabling real-time monitoring of viral evolution, identification of origins, and tracking of dissemination routes. Its application is particularly crucial within the One Health paradigm, which recognizes the interdependence of animal, environmental, and human health [7]. Approximately 60-80% of emerging human viruses have zoonotic origins, and vmNGS provides a central tool for early warning at the human-animal-environment interface [7].
Tracking Viral Mutations and Evolution
NGS enables high-resolution characterization of individual mutations in viral genomes, providing insights into evolutionary dynamics and treatment responses. Targeted NGS approaches using enrichment strategies allow researchers to focus sequencing on specific genomic regions, enabling deeper coverage and detection of rare variants [9].
For example, in studying evolving bacterial populations, researchers used xGen Lockdown Probes to perform target enrichment of commonly mutated genes [9]. This approach enabled them to track the frequency of mutations in evolving populations with sufficient sensitivity to detect competing mutations when they were still "new" and very rare within the population. Similar approaches can be applied to monitor the evolution of viruses, including key oncogenes in cancer-associated viruses [9].
In HIV research, NGS has revolutionized the tracking of drug resistance mutations (DRMs). Unlike Sanger sequencing, NGS can detect minority variants present in 1% to 20% of the viral population, which may increase the risk of treatment failure [10]. This additional information regarding relative abundance of susceptible/resistant strains strengthens our ability to assess the clinical impact of a given DRM and guide treatment strategies.
Experimental Protocols and Workflows
Viral Metagenomic Sequencing Workflow
The following diagram illustrates the core workflow for viral metagenomic sequencing:
Viral Genome Enrichment Protocol for Avian Orthoreoviruses
Sample Preparation and Viral Culture Conditions:
- Inoculate LMH cell monolayers at 95% confluency with viral inoculum
- Incubate at 38°C with 5% CO₂ for 5 days
- Harvest infected cells and supernatant by centrifugation at 3,000 × g for 10 minutes
- Resuspend pellet in virus dilution buffer and sonicate on ice (3 pulses at 30% amplitude, 10s on/30s off) [8]
ARV Genome Enrichment Protocol:
- Virion Purification: Use Capto Core 700 resin for initial purification
- Host rRNA Depletion: Treat with custom ssDNA probes targeting chicken rRNA, RNase H, and DNase I
- cDNA Synthesis: Convert viral RNA to cDNA using ARV-specific primers
- Single Primer Amplification PCR (R-SPA): Amplify cDNA using ARV-specific primers [8]
Library Preparation and Sequencing:
- For Illumina short-read sequencing: Use Nextera XT DNA Library Preparation Kit with IDT for Illumina DNA/RNA UD Indexes
- For Oxford Nanopore long-read sequencing: Follow ONT Rapid sequencing gDNA barcoding protocol
- Sequence Illumina libraries on MiSeq using Nano Kit v2 (500 cycles)
- Sequence ONT libraries on GridION platform [8]
Target Enrichment for Tracking Rare Mutations
Population Sequencing with Target Enrichment:
- Grow successive generations of microbial populations in liquid culture with daily transfers
- Monitor population dynamics using phenotypic markers (e.g., araA+/araA– clones on indicator agar)
- Isolate genomic DNA after desired generations (~500 generations)
- Prepare Illumina libraries with custom adapters containing barcoding sequences
- Perform target enrichment using ~120 xGen Lockdown Probes targeting genes of interest
- Follow Nimblegen SeqCap protocol with 72-hour hybridization
- Perform stringent washes with hard vortexing using reagents heated to 90°C
- Sequence enriched DNA on Illumina HiSeq platform [9]
Bioinformatic Analysis for Mutation Tracking:
- For improved confidence in rare variant calls, consider duplex sequencing using adapters with 12 random bases at the 3' end
- Use random barcodes to identify reads arising from the same gDNA molecule
- Generate consensus sequences to eliminate errors from single reads
- Track mutation frequencies across time points to calculate fitness effects [9]
Essential Research Reagents and Tools
Table 2: Key Research Reagent Solutions for Viral NGS
| Reagent/Kit | Function | Application Example |
|---|---|---|
| xGen Lockdown Probes | Target enrichment for specific genomic regions | Capturing viral genes of interest for deep sequencing [9] |
| Nextera XT DNA Library Prep Kit | Library preparation for Illumina platforms | Preparing metagenomic libraries from viral cDNA [8] |
| Capto Core 700 Resin | Virion purification | Initial purification of viral particles from cell culture [8] |
| Custom ssDNA Probes | Host rRNA depletion | Removing chicken rRNA from avian virus samples [8] |
| Universal Probe Library (UPL) | Quantitative digital PCR | Absolute quantification of NGS libraries [11] |
| ONT Rapid Barcoding Kit | Library preparation for Nanopore | Rapid barcoding of viral genomes for long-read sequencing [8] |
Data Analysis and Bioinformatics Pipeline
Quality Control and Preprocessing:
- For Illumina reads: Use Trimmomatic with Phred score threshold >30 [8]
- For Nanopore reads: Apply NanoFilt with Q value threshold of 7, then trim with Porechop [8]
Assembly Methods Comparison:
- De novo assembly: Use SPAdes for short reads or Canu/Flye for long reads
- Reference-guided assembly: Map quality-trimmed reads to custom reference genome using BWA or minimap2
- Hybrid assembly: Combine short and long reads for improved assembly quality [8]
Studies comparing assembly methods for avian orthoreoviruses found that regardless of sequencing technology, the best quality assemblies were generated by mapping quality-trimmed reads to a custom reference genome constructed from publicly available ARV genomic segments with highest sequence similarity to de novo contigs [8].
Quantitative Comparison Methods: For quantitative comparison of sequencing datasets, statistical methods like ChIPComp account for background signals, signal-to-noise ratios, biological variations, and multiple-factor experimental designs [12]. These methods model read counts following Poisson distribution, with underlying rates accounting for both technical artifacts and biological signals, enabling robust differential analysis [12].
Future Perspectives and Challenges
Despite its transformative potential, implementing NGS in viral genomics faces several challenges. Workflow complexity involves multiple steps with potential variables that need careful control [10]. Rigorous validation of equipment, methods, and processes is essential to ensure accurate, reproducible, and reliable results [10].
Cost and infrastructure requirements remain significant barriers, particularly for clinical settings and resource-limited environments [7]. The need for confirmation by secondary validated methods further complicates clinical implementation [10].
Data management and analysis present substantial hurdles, as NGS generates enormous datasets requiring sophisticated computational infrastructure and bioinformatics expertise [5] [10]. Interpretation of results often requires specialized knowledge, as seen with HIV drug resistance mutation profiling [10].
Looking forward, the field is moving toward more integrated surveillance systems based on the One Health approach [7]. As sequencing technologies continue to evolve, becoming more efficient, scalable, and cost-effective, NGS is poised to become a central tool for global pandemic preparedness and zoonotic disease control [5] [7]. The development of novel algorithms for data analysis and improved quantification methods will further enhance our ability to extract meaningful biological insights from the vast datasets generated by these powerful technologies [5] [11].
Next-generation sequencing (NGS) has become a cornerstone for tracking viral evolution and detecting mutations that confer drug resistance. This Application Note provides detailed protocols and resources for researchers focusing on the key genetic targets and methodologies essential for robust viral mutation rate studies.
The error-prone replication of viruses, combined with selective pressure from antiviral therapies, drives the emergence of drug-resistant viral variants. The traditional view that DNA viruses, such as herpesviruses, evolve slowly has been overturned; growing evidence shows they exist as dynamic populations with significant standing variation [13]. For instance, herpes simplex virus (HSV) populations can exhibit mutation frequencies as high as 3.6 x 10^-4 substitutions per base per plaque transfer, and nucleotide variations can be found in up to 3-4% of the HSV-1 genome between strains [13]. Detecting these minority variants, which can rise to dominance and cause treatment failure, requires sensitive and high-throughput sequencing approaches [13] [14]. Targeted next-generation sequencing (tNGS) offers a powerful, culture-independent solution, enabling comprehensive resistance profiling directly from clinical samples with high sensitivity and a relatively low cost [15] [16].
Key Viral Genetic Targets for Drug Resistance
Resistance mutations are not uniformly distributed across viral genomes; they are often concentrated in specific genes that are the targets of antiviral drugs. The table below summarizes critical genetic targets for major human viruses.
Table 1: Key Genetic Targets for Drug Resistance in Clinically Significant Viruses
| Virus | Genome Type | Key Target Genes/Proteins | Associated Antiviral Drugs | Clinical Impact of Resistance |
|---|---|---|---|---|
| Human Immunodeficiency Virus (HIV-1) | RNA | Protease (PR), Reverse Transcriptase (RT), Integrase (IN) [14] | Protease inhibitors, NRTIs, NNRTIs, Integrase inhibitors [14] | Treatment failure across multiple drug classes [14] |
| Hepatitis B Virus (HBV) | DNA | Reverse Transcriptase/Polymersase (RT) [14] | Nucleos(t)ide analogues (e.g., Lamivudine, Entecavir) [14] | Reduced efficacy of first-line treatments [14] |
| Hepatitis C Virus (HCV) | RNA | NS3, NS5A, NS5B [14] | Protease inhibitors, NS5A inhibitors, NS5B polymerase inhibitors [14] | Compromised efficacy of direct-acting antiviral (DAA) regimens [14] |
| Herpes Simplex Virus (HSV-1/2) | DNA | Thymidine Kinase (UL23), DNA Polymerase (UL30) [13] | Acyclovir, Famiciclovir [13] | Reduced susceptibility to first-line therapies [13] |
| Influenza A Virus (IAV) | RNA | Neuraminidase (NA), Matrix 2 (M2), Polymerase complex (PB2, PB1, PA) [17] | Oseltamivir, Zanamivir, Adamantanes [17] | Limited treatment options, especially during outbreaks [17] |
| Mycobacterium tuberculosis | DNA | katG, inhA, rpoB, pncA, gyrA, gyrB, rpsL, rrs [16] | Isoniazid, Rifampicin, Pyrazinamide, Fluoroquinolones [16] | Emergence of multi-drug (MDR) and extensively drug-resistant (XDR) TB [16] |
| SARS-CoV-2 | RNA | RNA-dependent RNA polymerase (RdRp), Spike (S) protein [14] | Remdesivir, Nirmatrelvir, monoclonal antibodies [14] | Escape from neutralizing antibodies and antiviral agents [14] |
Quantitative Performance of NGS in Resistance Detection
The analytical performance of NGS methods is critical for reliable variant detection. The following table compiles key performance metrics from recent studies.
Table 2: Analytical Performance of NGS Methodologies for Resistance Detection
| Methodology / Platform | Virus / Pathogen | Key Performance Metrics | Reference |
|---|---|---|---|
| Targeted NGS (tNGS) | Mycobacterium tuberculosis | 95.1% concordance with phenotypic AST; 87.95% positive rate in confirmed TB cases (vs 80.72% for Xpert MTB/RIF) [16] | [16] |
| Short-Read Sequencing (Illumina iSeq100/MiSeq) | HIV-1, HBV, HCV, TB, SARS-CoV-2 | High concordance for majority and minority variants; Q30 scores ≥80%; low error rates (<1%) [14] | [14] |
| Long-Read Sequencing (Oxford Nanopore MinION) | HIV-1, HBV, HCV, TB, SARS-CoV-2 | High concordance for majority subtypes; detected a higher number of minority mutations (<20%) compared to short-read platforms [14] | [14] |
| Optimized Whole-Genome Sequencing (Nanopore) | Influenza A Virus (IAV) | Robust whole-genome amplification from avian, swine, and human samples with low viral loads; enabled high-throughput multiplexing [17] | [17] |
Detailed Experimental Protocol for Targeted NGS of Viral Genes
This protocol outlines a generalized workflow for tNGS of viral genomes, adaptable for viruses like HIV, HBV, and HCV, based on established methods [14].
Sample Preparation and Nucleic Acid Extraction
- Sample Type: 200 µL of plasma, serum, or other clinical samples (e.g., bronchoalveolar lavage fluid) [16] [14].
- Extraction Method: Automated nucleic acid extraction is recommended for consistency. Use platform-specific kits, such as the MagNA Pure system (Roche) or the KingFisher Apex (Thermo Fisher Scientific) [14] [17].
- Quality Control: Quantify extracted nucleic acids using a fluorometer (e.g., Qubit Flex). For RNA samples, assess integrity if possible. Include positive and negative extraction controls to monitor for contamination [16] [14].
Target Amplification
This step uses multiplex PCR to amplify genomic regions associated with drug resistance.
- Principle: Pathogen-specific primer sets are used to generate amplicons covering known and potential drug resistance mutations under standardized conditions [14].
- Reaction Setup:
- Primers: Use commercially available, validated primer sets (e.g., DeepChek Assays) or published primers targeting critical regions (e.g., HIV pol gene, HBV RT gene) [14].
- Cycling Conditions (Example):
- Amplicon QC: Verify amplification success and specificity by running 5 µL of the PCR product on an agarose gel (e.g., E-Gel System) [14].
Library Preparation and Sequencing
This protocol is based on the Illumina platform [14].
- Purification and Quantification: Pool PCR amplicons if multiple regions were amplified separately. Purify the pool using magnetic beads (e.g., AMPure XP). Quantify the purified DNA with a fluorometer [14].
- Library Preparation: Use a commercial NGS library prep kit (e.g., DeepChek NGS Library preparation kit).
- Fragmentation and End-Repair: Enzymatically fragment 3 ng/µL of the amplicon pool at 37°C for 30 min, followed by end-repair and A-tailing [14].
- Adapter Ligation: Ligate indexed adapters to the fragments at 20°C for 15 min [14].
- Library Amplification: Perform 8 cycles of PCR to enrich the adapter-ligated fragments [14].
- Library QC and Normalization:
- Size Selection: Clean up the library with magnetic beads (0.8x ratio) to remove fragments outside the 200-800 bp range [14].
- Quality Assessment: Analyze 1 µL of the library on a fragment analyzer (e.g., TapeStation 4150) to confirm a peak at ~400 bp and the absence of primer-dimers [14].
- Quantification: Quantify the final library by qPCR to ensure a minimum concentration of 2 ng/µL [14].
- Sequencing:
Bioinformatic Analysis
A standardized pipeline is required to translate raw sequencing data into actionable mutation reports.
- Base Calling and Demultiplexing: Generate FASTQ files and assign reads to samples based on their unique indices [18].
- Read Processing: Trim low-quality bases and adapter sequences from the reads.
- Alignment: Map processed reads to a reference genome (e.g., HXB2 for HIV-1) using aligners like BWA or Bowtie2 [18].
- Variant Calling: Identify nucleotide variants relative to the reference, including single nucleotide polymorphisms (SNPs) and insertions/deletions (indels). Use specialized variant callers (e.g., DeepVariant) for high accuracy [19].
- Variant Annotation and Reporting: Annotate called variants with functional consequences (e.g., amino acid change) and known associations with drug resistance using databases like the WHO mutation catalog for TB [16]. Report mutations as consensus or minority variants based on a predefined frequency threshold (e.g., ≥5% or ≥20%) [14].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key reagents and tools required for successful implementation of viral resistance sequencing.
Table 3: Essential Research Reagents and Materials for Viral tNGS
| Item | Function / Application | Example Products / Kits |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolation of high-quality viral DNA/RNA from clinical samples. | MagNA Pure Kits (Roche), QIAamp Viral RNA Mini Kit (Qiagen), KingFisher Automated Systems [14] [17] |
| Target-Specific Primer Panels | Amplification of drug resistance-associated genomic regions. | DeepChek Assays (ABL Diagnostics) [14], custom-designed primer pools [17] |
| High-Fidelity PCR Master Mix | Accurate amplification of target sequences with low error rates. | Q5 Hot Start High-Fidelity DNA Polymerase (NEB), LunaScript RT Master Mix (NEB) [17] |
| NGS Library Prep Kit | Preparation of amplified DNA for sequencing on NGS platforms. | DeepChek NGS Library Prep Kit (ABL Diagnostics) [14] |
| NGS Sequencing Platform | High-throughput sequencing of prepared libraries. | Illumina (iSeq100, MiSeq), Oxford Nanopore (MinION) [14] [19] |
| Bioinformatics Software | Data analysis, variant calling, and interpretation of resistance mutations. | DeepChek Software (ABL Diagnostics), DeepVariant (Google) [14] [19] |
| Reference Materials & Controls | Ensuring assay accuracy, precision, and detecting contamination. | QCMD Panels, positive/negative extraction controls, non-template controls (NTC) [16] [14] |
| Alfalone | Alfalone, CAS:970-48-9, MF:C17H14O5, MW:298.29 g/mol | Chemical Reagent |
| Brassicasterol | Brassicasterol, CAS:474-67-9, MF:C28H46O, MW:398.7 g/mol | Chemical Reagent |
The precise identification of genetic targets for antiviral drug resistance is fundamental to effective therapy and public health surveillance. tNGS provides a powerful and flexible framework for detecting both majority and minority resistant variants across a broad spectrum of viruses. The protocols and resources detailed in this application note provide a roadmap for researchers to implement robust sequencing assays, enabling deeper insights into viral evolution and the preemptive management of treatment failure.
Next-generation sequencing (NGS) has revolutionized the study of viral pathogens by enabling researchers to analyze viral populations with unprecedented depth and resolution. Unlike traditional Sanger sequencing, which produces a consensus sequence, NGS can sequence millions of DNA fragments simultaneously, providing critical insights into genetically heterogeneous viral populations known as quasispecies [20] [5]. This technological advancement is particularly valuable for understanding viral evolution, as RNA viruses like Human Immunodeficiency Virus (HIV) mutate at remarkably high rates, with HIV-1 exhibiting mutation rates as high as 10â»Â³ nucleotide substitutions per site per year [20]. The error-prone activity of viral reverse transcriptase (RT) is largely responsible for this observed variability, creating complex distributions of closely related variant genomes that facilitate rapid adaptation to environmental pressures, including antiretroviral therapy [20].
The application of NGS in virology has opened new avenues for connecting specific genetic mutations to treatment outcomes, particularly through the identification of resistance-associated mutations (RAMs) that reduce drug efficacy. Numerous HIV-related outcomes can be determined from the viral genome, including resistance profiles, population transmission dynamics, viral heritability traits, and time since infection [21]. The shift from Sanger sequencing to NGS in HIV research over the past decade has been crucial because NGS achieves near full-length genome sequence coverage while simultaneously characterizing within-host diversity by encapsulating HIV subpopulations [21]. This detailed genetic information is essential for developing effective treatment strategies and understanding treatment failure mechanisms, making NGS an indispensable tool in both clinical virology and drug development pipelines.
Key NGS Technologies and Platforms
The selection of appropriate NGS platforms is fundamental to successful viral genomics research. Second-generation sequencing methods, often called short-read technologies, form the backbone of most current viral sequencing applications due to their high accuracy and throughput [5]. The Illumina platform utilizes a sequencing-by-synthesis method based on reversible dye terminators, making it particularly suitable for detecting single nucleotide variants and achieving high coverage depths necessary for identifying minority variants in viral populations [5]. However, researchers must be aware that sample overloading on Illumina platforms can result in overcrowding or overlapping signals, potentially increasing error rates to approximately 1% [5].
Third-generation sequencing technologies, exemplified by Pacific Biosciences (PacBio) Single-Molecule Real-Time (SMRT) sequencing and Oxford Nanopore sequencing, offer distinct advantages for specific viral genomics applications [5]. These platforms generate long reads that are invaluable for resolving complex genomic regions, haplotyping, and detecting structural variations. PacBio SMRT sequencing employs specialized cells housing numerous zero-mode waveguides (ZMWs) where individual DNA molecules are immobilized, with light emissions measured in real-time as polymerase incorporates nucleotides [5]. While PacBio systems traditionally focused on long-read sequencing, the recent introduction of the PacBio Onso system utilizes sequencing by binding (SBB) chemistry for short-read applications, providing an alternative to traditional Illumina workflows [5].
Table 1: Comparison of NGS Platforms for Viral Genomics
| Platform | Technology | Read Length | Key Strengths | Limitations | Ideal Viral Applications |
|---|---|---|---|---|---|
| Illumina | Sequencing-by-synthesis | 36-300 bp | High accuracy, low cost per base, high throughput | Short reads limit haplotype resolution | Variant calling, resistance mutation profiling, population diversity |
| PacBio SMRT | Single-molecule real-time | Average 10,000-25,000 bp | Long reads, direct epigenetics | Higher cost, lower throughput | Full-length viral genome assembly, complex variant detection |
| Oxford Nanopore | Nanopore sensing | Average 10,000-30,000 bp | Ultra-long reads, real-time analysis, portability | Higher error rate (~15%) | Rapid outbreak investigation, large structural variants |
| Ion Torrent | Semiconductor | 200-400 bp | Fast run times, simple workflow | Homopolymer errors | Targeted viral sequencing, resistance testing |
The computational requirements for NGS data analysis represent a critical consideration for research design. NGS data analysis is computationally intensive, requiring storage, transfer, and processing of very large data files that typically range from 1–3 GB in size [22]. Access to advanced computing resources, either on-site via private networks or cloud-based solutions, is highly recommended for efficient data processing [22]. Furthermore, while many user-friendly bioinformatic tools are available, researchers often require scripting and coding skills in languages such as Python, Perl, R, and Bash, typically performed within Linux or Unix-like operating environments [22].
NGS Data Analysis Framework
The analysis of NGS data follows a structured framework comprising three core stages: primary, secondary, and tertiary analysis [22]. Each stage transforms the data progressively from raw sequencing outputs to biologically meaningful conclusions about viral mutations and their potential clinical significance. Understanding this workflow is essential for properly interpreting NGS data in the context of viral resistance research.
Primary Analysis
Primary analysis begins with the assessment of raw sequencing data for quality control and initial processing [22]. For Illumina sequencing, the input is typically a binary base call (BCL) file containing raw intensity measurements and nucleotide base identifications [22]. Specialized software, such as bcl2fastq Conversion Software, processes these files to generate text-based FASTQ files, which contain the nucleotide sequences along with quality scores for each base [22]. During this stage, several critical quality metrics are assessed, including total sequencing yield, error rates based on internal controls, Phred quality scores (with Q>30 indicating <0.1% base call error rate), percentage of sequences aligned to control genomes, cluster density, and phasing/prephasing percentages [22].
A crucial step in primary analysis is demultiplexing, which separates sequencing data from multiple library samples that were processed concurrently [22]. Each sample is identified by unique index sequences, and demultiplexing generates individual FASTQ files corresponding to each sample in the experiment [22]. These files contain read names, flow cell locations, and other identifying information necessary for downstream analysis. Proper quality control at this stage is vital, as issues with sequencing efficiency or sample misidentification can compromise all subsequent analyses.
Secondary Analysis
Secondary analysis converts the raw sequence data into biologically interpretable results through a series of computational steps [22]. The process begins with read cleanup, where low-quality sequence reads and portions of reads are removed or trimmed—a process known as "soft-clipping" [22]. Tools like FastQC provide comprehensive quality assessment, including per-base quality scores, sequence quality distribution, GC content, and identification of duplicate or overrepresented sequences [22]. For viral RNA sequencing, additional specialized cleanup steps may include correction of sequence bias introduced during library preparation, quantitation of RNA types (such as ribosomal RNA contaminants), and determination of strandedness when directional sequencing kits are used [22].
Following quality control, sequencing reads are aligned to reference genomes using tools such as BWA or Bowtie 2 [22]. The choice of reference genome is critical, as inconsistencies can introduce artifacts in variant calling. For HIV research, standard references like HXB2 are commonly used, but researchers must document and consistently apply their chosen reference to ensure reproducibility [22]. The output from alignment is typically stored in Binary Alignment Map (BAM) files, which provide a compressed, efficient format for storing sequence alignment data [23]. These files can be visualized using genome browsers like the Integrative Genomic Viewer (IGV), allowing researchers to inspect read alignments, identify pileups in specific regions, and visually confirm potential mutations [22].
The final stage of secondary analysis involves mutation calling, where genetic variations that differ from the reference genome are identified [22]. For viral research, this includes identifying single nucleotide polymorphisms (SNPs), insertions, deletions, and other anomalies. The output is typically stored in Variant Call Format (VCF) files, which provide a standardized, text-based format for storing gene sequence variations [22]. For gene expression analysis in viral studies, tab-delimited formats (TSV files) are often used, with columns representing samples, genes, raw counts, and normalized counts [22].
Tertiary Analysis
Tertiary analysis represents the final stage where biological meaning is extracted from the processed data [22]. In the context of viral resistance research, this involves connecting identified mutations to known resistance profiles, interpreting their potential impact on treatment outcomes, and generating actionable reports. This stage often integrates additional data sources, including clinical patient information, drug treatment histories, and existing knowledge bases of resistance-associated mutations.
Experimental Protocol: NGS for HIV Drug Resistance Profiling
This section provides a detailed protocol for using NGS to profile HIV drug resistance mutations, based on established methodologies from the Swiss HIV Cohort Study and other research initiatives [21].
Sample Preparation and Library Construction
Begin with plasma samples from HIV-positive patients, ensuring proper ethical approvals and informed consent are obtained. Viral RNA should be extracted from 500-1000 μL of patient plasma using commercial viral RNA extraction kits. Include appropriate controls: negative extraction controls (nuclease-free water) and positive controls with known viral titers. Convert extracted RNA to cDNA using reverse transcriptase with gene-specific primers targeting the HIV pol gene, which encodes viral enzymes including reverse transcriptase and protease—primary targets of antiretroviral drugs.
Amplify the cDNA using a nested PCR approach with primers designed to target the entire protease gene and the first 1,000 nucleotides of the reverse transcriptase gene. This amplification strategy ensures adequate coverage of genomic regions where most known resistance-associated mutations occur. Purify PCR products using magnetic bead-based clean-up systems and quantify using fluorometric methods. For library preparation, utilize commercial library preparation kits compatible with your sequencing platform. During library preparation, incorporate unique dual indexes (UDIs) to enable multiplexing of multiple samples while preventing index hopping issues. Validate the final libraries using capillary electrophoresis systems to confirm appropriate fragment sizes and the absence of primer dimers.
Sequencing and Data Processing
Dilute libraries to appropriate concentrations and pool based on the desired sequencing depth. For viral resistance profiling, a minimum coverage of 10,000x per base is recommended to reliably detect low-frequency variants present at 1% or higher. Sequence the pooled libraries on an Illumina platform using a 2x150 bp paired-end sequencing strategy to ensure adequate overlap for read merging and high-quality consensus calling.
Process the raw sequencing data through the primary and secondary analysis workflow as described in Section 3. Begin by converting BCL files to demultiplexed FASTQ files using bcl2fastq software. Perform quality assessment of the FASTQ files using FastQC, then trim adapter sequences and low-quality bases using tools like Trimmomatic or Cutadapt. Align the processed reads to the HXB2 reference HIV genome using optimized aligners such as BWA or Bowtie2. Process the resulting SAM files into sorted BAM files, then mark and remove PCR duplicates using tools like Picard Tools. Call variants using a specialized viral variant caller such as LoFreq or VarScan2, which are optimized for detecting low-frequency variants in viral populations.
Table 2: Key Research Reagents for Viral NGS
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| RNA Extraction Kits | Commercial viral RNA kits | Isolate viral RNA from plasma | Evaluate yield and purity; avoid degradation |
| Reverse Transcriptase | MLV RT, AMV RT, thermostable RTs | cDNA synthesis from RNA template | Fidelity impacts mutation detection accuracy [20] |
| PCR Enzymes | High-fidelity DNA polymerases | Amplify target viral sequences | Minimize introduction of amplification errors |
| Library Prep Kits | Illumina Nextera, Swift Accel | Fragment DNA and add adapters | Compatibility with sequencing platform is critical |
| Quantification Kits | Qubit dsDNA HS Assay | Accurate DNA quantification | Fluorometric methods preferred over spectrophotometric |
| Unique Dual Indexes | Illumina IDT UDIs | Sample multiplexing | Reduce index hopping and cross-contamination |
Resistance Mutation Analysis
Annotate identified variants using specialized databases such as the Stanford HIV Drug Resistance Database. Categorize mutations based on their known association with resistance to specific drug classes: nucleoside reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), protease inhibitors (PIs), and integrase strand transfer inhibitors (INSTIs). Generate a comprehensive resistance report that includes the frequency of each resistance-associated mutation, the associated drug resistance levels, and potential cross-resistance patterns. For clinical interpretation, follow established guidelines from organizations such as the International Antiviral Society-USA.
Advanced Methods for Studying Viral Mutation Rates
Understanding the intrinsic mutation rates of viruses provides crucial insights into their evolutionary dynamics and capacity for developing drug resistance. Several advanced NGS-based methods have been developed specifically for characterizing the fidelity of viral reverse transcriptases and RNA-dependent RNA polymerases, addressing the limitations of traditional enzymatic and reporter-based assays [20].
The PRIMER ID method incorporates unique molecular identifiers (UMIs) during the reverse transcription step, allowing researchers to distinguish true biological mutations from errors introduced during PCR amplification and sequencing [20]. Each cDNA molecule is tagged with a random oligonucleotide "primer ID," enabling bioinformatic tracking of amplification products derived from the original viral RNA molecule. This approach significantly reduces artifacts and provides more accurate measurements of viral mutation frequencies.
Other specialized methods include Circular Sequencing (CIR-SEQ), which uses circularization of RNA templates to achieve multiple passes of sequencing, thereby enhancing accuracy, and Single-Molecule Real-Time Sequencing (SMRT-SEQ) that allows direct observation of polymerase activity without amplification bias [20]. Rolling Circle Sequencing (ROLL-SEQ) applies similar principles to circular templates for high-fidelity variant detection. These techniques are particularly valuable for studying the mutation profiles of different reverse transcriptases, including those from HIV-1, HIV-2, and non-retroviral RTs like the thermostable group II intron RT (TGIRT) from Geobacillus stearothermophilus [20].
Data Management and Implementation Considerations
The implementation of NGS for viral resistance studies requires robust data management strategies to handle the substantial computational and storage challenges associated with genomic data. The Swiss HIV Cohort Study Viral NGS Database (SHCND) exemplifies an effective solution, addressing key issues in handling NGS data including high volumes of raw and processed data, storage solutions, application of sophisticated bioinformatic tools, high-performance computing resources, and reproducibility [21].
A dedicated NGS database should incorporate several key design elements: centralized storage of all NGS data with standardized metadata annotation, direct integration of bioinformatic pipelines for automated processing, version control for analysis protocols, and secure access mechanisms for researchers [21]. The SHCND, which includes NGS sequences from 5,178 unique people with HIV (PWH) as of 2025, has demonstrated its utility across multiple research projects on HIV pathogenesis, treatment, drug resistance, and molecular epidemiology [21]. This approach ensures data integrity, facilitates collaboration, and enables the integration of genomic data with clinical metadata for comprehensive analysis.
For laboratories establishing viral NGS capabilities, several practical considerations are essential. Data storage requirements can be substantial, with raw FASTQ files for a single sample typically ranging from 1-50 GB depending on the sequencing depth [23]. Compressed alignment files (BAM format) typically reduce storage needs by 30-50% compared to uncompressed files, while CRAM format can offer an additional 30-60% size reduction through reference-based compression [23]. Computational infrastructure must support the processing demands of alignment and variant calling, which often requires high-performance computing clusters or cloud-based solutions. Additionally, standardized operating procedures for data analysis, including specific versions of bioinformatic tools and reference genomes, are critical for ensuring reproducible results across different experiments and research groups.
Table 3: NGS Data Management and File Formats
| Data Type | Standard Format | Size Range | Primary Use | Tools for Handling |
|---|---|---|---|---|
| Raw Reads | FASTQ | 1-50 GB | Store sequences with quality scores | FastQC, Trimmomatic, Cutadapt |
| Alignments | BAM | 30-50% smaller than FASTQ | Store mapped reads; enable visualization | SAMtools, BWA, Bowtie2, IGV |
| Alignment Index | BAI | Small | Enable random access to BAM files | SAMtools, Picard |
| Variants | VCF | Variable | Store mutation calls | BCFtools, GATK, SnpEff |
| Compressed Alignments | CRAM | 30-60% smaller than BAM | Long-term storage; data transfer | SAMtools |
Next-generation sequencing has fundamentally transformed our approach to understanding viral mutations and their relationship to treatment outcomes. The methodologies outlined in this application note provide researchers with a comprehensive framework for implementing NGS-based approaches to study viral resistance mechanisms. By integrating advanced sequencing technologies with robust bioinformatic analyses and proper data management practices, researchers can accurately identify resistance-associated mutations, characterize viral diversity, and elucidate the genetic basis of treatment failure.
The continued evolution of NGS technologies, including the emergence of long-read sequencing and improved single-molecule methods, promises to further enhance our ability to study viral populations with increasing resolution and accuracy. As these technologies become more accessible and standardized, their implementation in clinical and research settings will be crucial for advancing our understanding of viral evolution, optimizing treatment strategies, and ultimately improving patient outcomes in the face of rapidly evolving viral pathogens.
NGS in Action: Methodologies and Clinical Applications for Viral Mutation Detection
Within viral genomics research, targeted sequencing has become an indispensable methodology for focusing resources on specific genomic regions of interest, enabling deeper characterization of viral diversity and evolution. This approach is particularly critical for studying viral mutation rates, where capturing complete haplotypes and resolving complex variations is essential. Targeted sequencing allows researchers to bypass the unnecessary sequencing of entire viral or host genomes, concentrating instead on key genes or regions known to influence pathogenicity, immune evasion, or drug resistance [24]. Two powerful strategies for target enrichment—long-range PCR and amplicon-based sequencing—provide robust frameworks for generating high-quality viral genomic data, even from challenging sample types like clinical isolates and environmental wastewater [25] [26].
The application of these methods in virology addresses several inherent challenges of short-read sequencing, including limited ability to phase distantly separated variants and difficulties in analyzing regions with high sequence homology or complex repeats [27] [24]. Long-read sequencing technologies, such as those offered by Oxford Nanopore Technologies (ONT) and PacBio, when coupled with targeted enrichment, now enable researchers to obtain complete viral genomes with unambiguous haplotype resolution, providing deeper insights into viral quasispecies evolution and transmission dynamics [24] [28].
Long-Range PCR for Targeted Viral Sequencing
Principles and Workflow Optimization
Long-range PCR (LR-PCR) refers to the amplification of DNA targets over 5 kilobases (kb) in length, which typically cannot be amplified using routine PCR methods or reagents [29]. This technique is particularly valuable in viral genomics for generating large amplicons that span significant portions of viral genomes or entire smaller viral genomes in a single fragment. Successful LR-PCR traditionally employs a blend of DNA polymerases—typically a primary polymerase for fast elongation combined with a proofreading enzyme for accuracy [29]. The proofreading component repairs DNA mismatches incorporated at the 3' end of the growing strand, allowing the primary polymerase to continue elongation much further, resulting in successful amplification of long DNA fragments.
Recent methodological advances have optimized LR-PCR for integration with long-read sequencing platforms. A 2025 study established a robust, end-to-end workflow for phasing and localizing variants using LR-PCR and targeted Nanopore sequencing, demonstrating successful amplification of targets up to 22 kb with a 90% success rate using the UltraRun LongRange PCR Kit [27]. Critical optimization steps included careful primer design in unique sequence regions, adherence to manufacturer-recommended PCR programs with single annealing temperatures and extension times to enable processing of multiple samples simultaneously, and limitation of PCR cycles to 26 to minimize the generation of chimeric reads—a known PCR artifact where two different biological sequences combine, potentially affecting sequencing accuracy and phasing [27].
Application in Viral Research
LR-PCR has been successfully implemented in sequencing complex viral genomes, including Human Papillomavirus 16 (HPV16). A 2025 study developed a scalable HPV16 whole-genome sequencing approach using ONT's MinION and PromethION2 platforms that employed multiple primer set designs, including a near full-length primer set generating amplicons up to 7.7 kb to capture intact or nearly full-length HPV16 DNA [28]. This strategy enabled researchers to comprehensively analyze HPV16 genetic diversity among women in sub-Saharan African countries, generating complete HPV16 genomes at high coverage (median read coverage: 5,899–15,279×) and identifying all four previously defined HPV16 lineages (A–D) and their high-risk sublineages [28].
The method demonstrated sufficient sensitivity to amplify and sequence as few as five copies of HPV16 per reaction, making it particularly valuable for working with low-biomass clinical samples often encountered in viral research [28]. The successful application of this LR-PCR approach in resource-limited settings highlights its potential for decentralizing genomic surveillance and enabling in-country sequencing capabilities in regions most affected by viral pathogens.
Table 1: Performance Metrics of Optimized Long-Range PCR in Viral Sequencing Applications
| Parameter | Performance Metric | Experimental Context |
|---|---|---|
| Success Rate | 90% for amplification up to 22 kb | Human genomic DNA amplification [27] |
| Chimeric Read Rate | Median 2.80% (range 1.79–16.12%) | Under optimized conditions [27] |
| Variant Phasing Concordance | 100% for SNV pairs and small InDels | Inter-variant distances 5.8–21.4 kb [27] |
| Sensitivity | As few as 5 HPV16 copies per reaction | CaSki cell line DNA [28] |
| Coverage Depth | Median 5,899–15,279× | HPV16 clinical samples [28] |
Experimental Protocol: Long-Range PCR for Viral Genome Amplification
Sample Preparation and DNA Extraction
- Begin with viral propagation in appropriate cell lines (e.g., Vero E6 cells for TOSV) or clinical samples (cervical exfoliated cells for HPV16) [30] [28].
- Extract nucleic acids using commercial kits (e.g., QIAsymphony with "Virus Pathogens DSP Midi Kit" for RNA viruses), eluting in 60 μL volume [25].
- For DNA viruses, use proteinase K digestion followed by column-based purification.
- Quantify extracted nucleic acids using fluorometric methods and assess quality via spectrophotometric ratios (A260/280 ≈ 1.8-2.0).
Primer Design
- Design primers targeting conserved regions of viral genomes using alignment software (MAFFT v7.525) and specialized primer design tools (FastPCR software) [25] [30].
- For comprehensive genome coverage, design multiple overlapping amplicons (e.g., three amplicons of 4961 bp, 6378 bp, and 4860 bp for RSV-A) [25].
- Incorporate degenerate bases at variable positions to enhance binding efficacy across diverse viral strains [30].
- Verify primer specificity using BLAST analysis against relevant databases.
Long-Range PCR Amplification
- Select appropriate LR-PCR kit (e.g., UltraRun LongRange PCR Kit, Platinum SuperFi II PCR Master Mix) based on target length [27] [25].
- Prepare 20-50 μL reactions containing 1X PCR master mix, 0.5 μM each forward and reverse primer, and 150 ng DNA or 10 μL RNA (for reverse transcription PCR) [27] [25].
- Use the following thermocycling conditions for DNA amplification:
- Initial denaturation: 94°C for 2 minutes
- 26 cycles of:
- Denaturation: 94°C for 15 seconds
- Annealing: 60-68°C (primer-specific) for 30 seconds
- Extension: 68°C for 1 minute per kb (adjust based on target length)
- Final extension: 68°C for 5-10 minutes
- For RNA viruses, include initial reverse transcription step (50°C for 10-30 minutes) using systems like SuperScript IV One-Step RT-PCR [25].
PCR Product Cleanup and Quantification
- Analyze amplicons using capillary electrophoresis (e.g., Agilent 4200 TapeStation System) [27].
- Define successful amplification as presence of clear band with concentration >2 ng/μL without significant non-specific products.
- Purify amplicons using bead-based cleanups (e.g., AMPure XP beads) if necessary.
- Quantify using fluorometric methods and normalize concentrations for library preparation.
Amplicon-Based Sequencing Strategies
Tiled Amplicon Approaches for Viral Genome Sequencing
Amplicon-based sequencing utilizes polymerase chain reaction (PCR) to selectively amplify genetic regions of interest, with primers designed to bookend target regions so the resulting amplicons can be specifically sequenced [24]. While simple and cost-effective, this approach has been significantly enhanced through tiling strategies that amplify overlapping fragments spanning entire viral genomes. This method has become particularly valuable for viral surveillance, enabling comprehensive genomic characterization even from low-concentration samples.
A novel targeted tiled amplicon-based sequencing protocol developed for sequencing the Hemagglutinin (HA) gene segment of seasonal influenza A and B viruses from wastewater demonstrates the power of this approach for public health surveillance [26]. The method uses short tiled amplicons (<250 bp in length) to successfully capture the HA gene segment, achieving consistent coverage across the gene in samples with influenza viral target digital PCR detections of at least 10³ copies/L [26]. This sensitivity threshold makes it possible to monitor viral evolution and detect low-frequency single nucleotide variants (SNVs) at high depth of coverage, providing insights into the diversity of circulating influenza viruses at the community level.
Similarly, an improved high-throughput amplicon-based whole-genome sequencing assay for Respiratory Syncytial Virus (RSV) was designed with three distinct amplicons covering the entire ~15.2 kb RSV genome [25]. This protocol achieved success in approximately 95% of samples with relatively low viral load (typically corresponding to cycle of quantification values of 27-32) and produced exceptionally high median depth of coverage (over 12,000×) with more than 1×10ⶠmapped reads [25]. Sequences passing quality filters showed coverage of at least 98% across the entire genome, enabling robust phylogenetic analysis and detection of emerging variants.
Implementation for Viral Surveillance
The development of a novel amplicon-based whole-genome sequencing framework for Toscana virus (TOSV) showcases the adaptability of this approach for emerging viral threats [30]. Researchers designed 45 oligonucleotide primer pairs based on TOSV lineage A reference sequences, generating 26 primer pairs for segment L, 13 for segment M, and 6 for segment S capable of amplifying overlapping sequences spanning the entire TOSV genome [30]. Strategic incorporation of degenerate bases in the primers enhanced sensitivity by maximizing binding efficacy to multiple strains, mitigating the risk of amplification failure across diverse viral isolates.
Sensitivity testing of this TOSV amplicon sequencing method demonstrated robust performance at viral RNA concentrations above 10² copies/μL, with coverage exceeding 96% across all genomic segments [30]. At higher concentrations (10³-10ⴠcopies/μL), the method achieved nearly complete genome recovery with consensus lengths consistently full-length for all segments, suggesting excellent assembly and comprehensive genomic characterization [30]. This performance highlights the utility of amplicon-based approaches for building genomic databases for understudied pathogens, enabling large-scale studies of genetic diversity and evolutionary dynamics critical for improving diagnostics and public health strategies.
Table 2: Performance Characteristics of Amplicon-Based Sequencing for Viral Surveillance
| Virus | Amplicon Strategy | Sensitivity | Coverage | Application Context |
|---|---|---|---|---|
| Influenza A/B | Short tiled amplicons (<250 bp) | 10³ copies/L | Consistent coverage across HA gene | Wastewater surveillance [26] |
| RSV | Three amplicons (4.9-6.4 kb) | Cq ≤32 (≥10³.ⵠRNA copies/mL) | ≥98% full genome | Clinical samples [25] |
| TOSV | 45 primer pairs (tiled) | >10² copies/μL | >96% (all segments) | Viral propagates, clinical samples [30] |
| HPV16 | Full-length + tiling primers | 5 copies/reaction | 5,899-15,279× median depth | Clinical isolates, cell lines [28] |
Experimental Protocol: Tiled Amplicon Sequencing for Viral Genomes
Primer Design and Validation
- Retrieve complete genome sequences of target virus from public databases (e.g., Nextstrain) representing recent circulating strains [25].
- Align sequences using MAFFT v7.525 or similar alignment software to identify conserved regions [25] [30].
- Design primer pairs to generate overlapping amplicons of 400-500 bp for short-read platforms or 2-7 kb for long-read platforms [30] [28].
- Incorporate degenerate bases at polymorphic positions to enhance coverage across diverse strains [30].
- Validate primer specificity in silico using BLAST and evaluate efficiency with FastPCR software [25].
- Conduct phylo-primer-mismatch analysis by mapping primer sequences against strain alignment to visualize mismatches across phylogenetic tree [25].
Library Preparation and Sequencing
- For RNA viruses: perform reverse transcription using SuperScript IV One-Step RT-PCR System or equivalent [25].
- Amplify viral genome in multiple separate RT-PCR/PCR reactions (e.g., 3 reactions for RSV covering different genome segments) [25].
- Use 50 μL reactions containing 10 μL total RNA, appropriate primer concentrations (typically 0.5 μM final concentration), and master mix [25].
- Pool PCR products in equimolar ratios after quantification and quality assessment.
- Proceed with library preparation using platform-specific kits:
- Sequence on appropriate platform (Illumina for short-read, GridION/PromethION for long-read).
Bioinformatic Analysis
- Perform basecalling and demultiplexing using platform-specific tools (e.g., MinKNOW/dorado for Nanopore) [27].
- Align reads to reference genome using Minimap2 (long-read) or BWA (short-read) [27] [28].
- For amplicon-based data: implement primer trimming and consider amplicon-aware alignment.
- Conduct variant calling using appropriate tools:
- Generate consensus sequences and perform phylogenetic analysis for lineage assignment.
Successful implementation of long-range PCR and amplicon-based sequencing strategies requires careful selection of molecular biology reagents, sequencing kits, and bioinformatic tools. The following table summarizes key solutions utilized in the protocols cited in this application note.
Table 3: Essential Research Reagents and Resources for Viral Targeted Sequencing
| Category | Specific Product/Kits | Application Purpose | Key Features |
|---|---|---|---|
| LR-PCR Kits | UltraRun LongRange PCR Kit (Qiagen) | Amplification of long targets (up to 22 kb) | 90% success rate for long targets [27] |
| Platinum SuperFi II PCR Master Mix (Invitrogen) | High-fidelity amplification of complex templates | Proofreading activity, high processivity [27] | |
| LongAmp Taq 2X Master Mix (NEB) | Robust amplification of GC-rich targets | Blended polymerase system [27] | |
| Reverse Transcription Kits | SuperScript IV One-Step RT-PCR System | Whole-genome amplification of RNA viruses | High sensitivity, high fidelity [25] |
| Sequencing Kits | Ligation Sequencing Kit V14 (SQK-LSK114, ONT) | Library preparation for Nanopore sequencing | Compatible with native barcoding [27] |
| Native Barcoding Kit 24 V14 (SQK-NBD114.24, ONT) | Multiplexing samples on Flongle/GridION | Enables up to 8-plex per flow cell [27] | |
| Illumina Microbial Amplicon Prep (iMAP) | Amplicon sequencing on Illumina platforms | Optimized for tiled amplicon workflows [30] | |
| Bioinformatic Tools | Clair3 | Variant calling from long-read data | Combines pileup and full-alignment approaches [27] [28] |
| PEPPER-Margin-DeepVariant | Variant calling pipeline | Full-alignment method for high precision [28] | |
| WhatsHap, HapCUT2 | Phasing of genetic variants | Resolves haplotypes from long-read data [27] | |
| Minimap2 | Alignment of long reads to reference | Fast and accurate for noisy long reads [27] |
Long-range PCR and amplicon-based sequencing strategies represent powerful approaches for targeted viral sequencing, each with distinct advantages for different research contexts. LR-PCR excels in generating long amplicons that span complex genomic regions or entire viral genomes, enabling comprehensive haplotype resolution and characterization of structural variations [27] [28]. Tiled amplicon approaches provide exceptional depth of coverage across target regions, making them ideal for detecting low-frequency variants and working with challenging sample types like wastewater and low-viral-load clinical specimens [25] [26].
The integration of these targeted enrichment methods with third-generation sequencing platforms has dramatically improved our ability to study viral mutation rates and evolution. By providing complete viral haplotypes and resolving complex genomic regions that were previously intractable to short-read sequencing, these approaches enable researchers to track viral transmission pathways, identify emerging variants of concern, and understand the molecular mechanisms driving viral evolution. As these methodologies continue to mature and become more accessible, they promise to further democratize viral genomic surveillance, enabling researchers worldwide to contribute to our collective understanding of viral dynamics and evolution.
Next-generation sequencing (NGS) has revolutionized the management of viral infections in immunocompromised patients, enabling high-resolution detection of antiviral resistance mutations. For Human Cytomegalovirus (HCMV) and Human Immunodeficiency Virus (HIV), the emergence of drug-resistant strains poses a significant challenge to successful long-term therapy [31] [32]. NGS surpasses traditional Sanger sequencing by detecting minority variants present at frequencies as low as 1-5%, providing an early warning system for emerging resistance and allowing for more informed clinical decision-making [31] [32] [10]. This document outlines detailed application notes and protocols for implementing NGS-based antiviral resistance monitoring for HCMV and HIV within a clinical research context.
Recent surveillance data highlights the prevalence and trends of antiviral resistance in HCMV and HIV, underscoring the need for continuous monitoring.
Table 1: Documented Resistance Mutations and Their Frequencies
| Virus | Gene/Region | Key Resistance Mutations | Associated Antiviral(s) | Reported Frequency |
|---|---|---|---|---|
| HCMV | UL97 | Various (e.g., G579C) [33] | (Val)ganciclovir, Maribavir [31] | Found in 25% of patients with novel mutations [33] |
| UL54 | Various (e.g., A835T, P522S) [33] | Ganciclovir, Cidofovir, Foscarnet [31] | Found in 25% of patients with novel mutations [33] | |
| UL56 / UL89 | Various [31] | Letermovir [31] | Not specified | |
| HIV | Reverse Transcriptase | K65R, M184I/V [34] | Tenofovir, Emtricitabine/Lamivudine [34] | 22% in seroconversions on PrEP [34] |
| Integrase | R263K [35] | Dolutegravir, Bictegravir [35] | Increasing prevalence [35] | |
| Protease | Multiple major mutations [35] | Protease Inhibitors | 2.1% (in HIV DNA, 2024) [35] |
Table 2: HIV Drug Resistance Trends Over Time (2018-2024) [35]
| Resistance Category | Prevalence in HIV RNA (2018) | Prevalence in HIV RNA (2024) | Trend |
|---|---|---|---|
| Any Drug Resistance | ~30% | ~25% | â–¼ Declining |
| NRTI + NNRTI Resistance | 6.1% | 3.5% | â–¼ Declining |
| Dual NRTI + INSTI Resistance | 8.7% | 4.7% | â–¼ Declining |
| Protease Inhibitor Resistance | <3% | <3% | â–º Stable |
Experimental Protocols for NGS-Based Resistance Detection
NGS Protocol for HCMV Antiviral Resistance
This protocol is adapted from a validated procedure for sequencing HCMV genes associated with antiviral resistance [31].
1. Primer Design and Multiplex PCR Setup:
- Design: Design primers to generate 400-800 bp amplicons covering full coding sequences of target genes (UL27, UL54, UL55, UL56, UL89, UL97) using the HCMV Merlin strain (NC_006273.2) as a reference. Utilize tools like Primal Scheme and refine with multiple sequence alignment to ensure coverage of genetic diversity [31].
- Multiplexing: Group primer sets into three multiplex pools to avoid dimerization [31].
- PCR Master Mix:
- Primer Pool (final concentration 0.08-0.1 µM)
- 1x Q5 Reaction Buffer
- 0.2 mM dNTPs
- <10 ng viral DNA template
- 0.02 U/µL Q5 High-Fidelity DNA Polymerase
- 1x Q5 High GC Enhancer
- Nuclease-free water to 25 µL [31].
- Thermocycling Conditions:
- Initial Denaturation: 98°C for 15 min.
- 35 Cycles: 95°C for 15 s, 62°C for 5 min.
- Final Extension: 62°C for 5 min.
- Hold at 4°C [31].
2. Library Preparation and Sequencing:
- Purify the multiplex PCR products.
- Prepare sequencing libraries using the Illumina Nextera XT kit.
- Sequence on an Illumina MiSeq platform with a minimum of 100,000 reads per sample to ensure adequate depth for variant calling [31].
3. Bioinformatic Analysis:
- Quality Control: Use FastQC to assess raw read quality.
- Alignment: Map reads to the HCMV reference genome (NC_006273.2) using BWA or similar aligner.
- Variant Calling: Identify single nucleotide variants (SNVs) and indels using tools like GATK. The limit of detection for minority variants is ~5% [31].
- Interpretation: Compare identified amino acid substitutions to published databases (e.g., CHARMD, HerpesDRG) to classify mutations as confirmed resistance-associated, polymorphic, or novel [33].
Hybrid NGS Protocol for HIV-2 Drug Resistance
This protocol details a hybrid NGS approach for HIV-2, which is inherently resistant to some antiretrovirals [36].
1. Sample Preparation and Amplification:
- Extract viral RNA from plasma samples.
- Perform reverse transcription to generate cDNA.
- Amplify the protease, reverse transcriptase, and integrase regions of the HIV-2 pol gene using a one-touch PCR approach.
2. Library Preparation and Sequencing:
- Prepare sequencing libraries from the amplified cDNA.
- Sequence the libraries using an Ion Torrent platform (e.g., GeneStudio S5) [36].
3. Data Analysis and Validation:
- Analysis: Use the Torrent Suite and Ion Reporter software for base calling, alignment, and variant identification.
- Validation: The protocol demonstrated 92% amplification success for protease, 91% for reverse transcriptase, and 49% for integrase in a cohort of 100 samples. It showed strong agreement with Sanger sequencing while additionally detecting minority variants like K70E and M184V that Sanger missed [36].
Workflow Visualization
The following diagram illustrates the generalized NGS workflow for antiviral resistance profiling, applicable to both HCMV and HIV with target-specific modifications.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of NGS for antiviral resistance monitoring requires a suite of specialized reagents and computational tools.
Table 3: Key Research Reagent Solutions and Materials
| Category | Item | Specific Example / Function | Application |
|---|---|---|---|
| Wet-Lab Reagents | High-Fidelity DNA Polymerase | Q5 High-Fidelity DNA Polymerase (NEB) | Accurate amplification of target viral genes for sequencing [31]. |
| NGS Library Prep Kit | Illumina Nextera XT; Ion Chef System | Prepares amplified DNA for sequencing on the respective platform [31] [37]. | |
| Targeted Amplicon Panel | Custom-designed multiplex primer pools | Enriches specific viral genes (e.g., UL54, UL97 for HCMV; pol for HIV) [31] [37]. | |
| Platform & Sequencing | NGS Sequencer | Illumina MiSeq; Ion Torrent S5 | Generates high-throughput sequence data [31] [36]. |
| Bioinformatics | Primary Analysis Software | Torrent Suite (Ion Torrent); Illumina DRAGEN | Performs base calling, quality control, and initial alignment [37]. |
| Secondary Analysis & Interpretation | Stanford HIVdb; In-house HCMV pipelines | Annotates variants and interprets drug resistance from sequence data [32] [38]. | |
| Data Visualization | MultiQC; Custom scripts | Provides QC overview and visualization of results [38]. | |
| Corilagin (Standard) | Corilagin (Standard), CAS:23094-69-1, MF:C27H22O18, MW:634.5 g/mol | Chemical Reagent | Bench Chemicals |
| Demethylsuberosin | Demethylsuberosin, CAS:21422-04-8, MF:C14H14O3, MW:230.26 g/mol | Chemical Reagent | Bench Chemicals |
Next-generation sequencing (NGS) has revolutionized virology, transforming applications far beyond routine surveillance into powerful tools for viral discovery and outbreak investigation. This transformative technology provides unparalleled capabilities for analyzing viral DNA and RNA molecules in a high-throughput and cost-effective manner, enabling researchers to decode complex viral dynamics with unprecedented resolution [5]. The versatility of NGS platforms has fundamentally expanded the scope of viral genomics research, facilitating studies on viral quasispecies diversity, mutation rates, and evolutionary trajectories [4]. As these technologies continue to evolve, they offer increasingly sophisticated approaches to unravel the mutational landscape of viral populations, providing critical insights for drug development, vaccine design, and therapeutic interventions [39] [4].
For virologists and pharmaceutical researchers, understanding viral mutation rates is particularly crucial as it determines the ability of viruses to evolve, infect new hosts, evade immunity, and develop drug resistance [40]. The application of NGS in this context has moved beyond traditional consensus sequencing to enable the detection and quantification of low-frequency viral variants within genetically diverse quasispecies populations—many of which have significant therapeutic importance for understanding treatment outcomes and resistance pathways [4]. This application note details standardized protocols and analytical frameworks for leveraging NGS technologies to investigate viral mutation rates, with direct applications in viral discovery and outbreak investigation.
The selection of appropriate sequencing platforms is fundamental to successful viral genomics research. Current technologies are broadly categorized into second and third-generation sequencing platforms, each with distinct advantages for specific virological applications [39].
Second-generation sequencing platforms, primarily characterized by short-read technologies such as Illumina, provide high-throughput capabilities with exceptional accuracy (exceeding 99.9%) [5] [39]. These platforms utilize sequencing-by-synthesis chemistry with reversible dye terminators, enabling parallel sequencing of millions of DNA fragments [5] [41]. The high accuracy and throughput make these platforms ideal for variant detection and quantifying minor allele frequencies within viral quasispecies [4]. However, the shorter read lengths (typically 75-600 bases) can present challenges for de novo assembly of novel viruses and resolving complex genomic regions [41] [39].
Third-generation sequencing technologies, represented by PacBio's Single Molecule Real-Time (SMRT) sequencing and Oxford Nanopore Technologies (ONT), generate long reads ranging from thousands to millions of bases [5] [39]. PacBio's SMRT sequencing employs polymerase molecules immobilized in zero-mode waveguides (ZMWs) to monitor nucleotide incorporation in real-time [5]. This technology can produce high-fidelity (HiFi) reads through circular consensus sequencing, achieving base-level resolution with 99.9% single-molecule accuracy [39]. Nanopore sequencing represents a more fundamental departure from traditional methods, relying on the detection of electrical current changes as nucleic acid molecules pass through protein nanopores [5] [42] [39]. The key advantages of nanopore technology include extreme read lengths (theoretically limited only by molecule size), direct RNA sequencing capability, portability, and real-time data analysis [42] [39].
Table 1: Comparison of Sequencing Platforms for Viral Genomics
| Platform | Technology Type | Maximum Read Length | Accuracy | Key Advantages | Ideal Viral Applications |
|---|---|---|---|---|---|
| Illumina | Short-read sequencing-by-synthesis | 2×300 bp (NextSeq 2000) | >99.9% | High throughput, low cost per base, excellent for variant calling | Viral quasispecies diversity, minority variant detection, targeted sequencing |
| PacBio SMRT | Long-read sequencing-by-synthesis | 100 kb | 99.87% (HiFi reads) | Long reads, single-molecule resolution, detects base modifications | De novo viral assembly, haplotype resolution, complex region sequencing |
| Oxford Nanopore | Long-read nanopore sequencing | 4.2 Mb | <99.5% (simplex) | Portability, real-time analysis, direct RNA sequencing, low cost | Outbreak field deployment, novel virus discovery, RNA virus sequencing |
| Ion Torrent | Short-read semiconductor sequencing | 400 bp | Similar to Illumina | Rapid sequencing, lower initial investment | Rapid diagnostics, amplicon sequencing, mutation profiling |
The emerging paradigm for comprehensive viral genome analysis often involves hybrid approaches that leverage both short and long-read technologies, using Illumina data to polish assemblies generated from long-read platforms [39]. This integrated approach maximizes both accuracy and contiguity, providing optimal results for mutation rate studies and outbreak investigation.
Application Note 1: Viral Discovery and Characterization
Protocol: Metagenomic Sequencing for Viral Discovery
Principle: Untargeted metagenomic sequencing enables comprehensive detection of viral nucleic acids in clinical, environmental, or animal samples without prior knowledge of the viral content [43]. This approach has successfully identified numerous novel viruses, including influenza D virus, porcine circovirus 3, and various coronaviruses [43].
Workflow:
Sample Processing and Nucleic Acid Extraction
- Process 200-500 µL of clinical sample (serum, CSF, respiratory secretions, tissue homogenate)
- Extract total nucleic acids using silica membrane columns or magnetic bead-based systems
- Include DNase/RNase treatment steps to remove non-encapsidated nucleic acids
- Quantify using fluorometric methods (Qubit) – minimum 10 ng/µL required
Library Preparation
- Fragment DNA via acoustic shearing (200-500 bp) for Illumina or use native DNA for Nanopore
- Perform reverse transcription for RNA viruses using random hexamers and target-specific primers
- Use ultra-low input library preparation kits (1-10 ng input) for precious samples
- Employ dual indexing to enable sample multiplexing
Sequencing
- Illumina Platform: Sequence on NextSeq 2000 with 2×150 bp chemistry, targeting 20-50 million read pairs per sample
- Nanopore Platform: Use MinION flow cells (R10.4.1) with 48-hour sequencing runs for maximum yield
- Include positive control (phage PhiX174) and negative extraction controls
Bioinformatic Analysis
- Quality control: FastQC for Illumina, NanoPlot for Nanopore
- Host depletion: Map reads to host genome (human, porcine, etc.) using BWA or minimap2
- De novo assembly: Unicycler for hybrid approaches, metaSPAdes for Illumina-only, Canu for Nanopore
- Taxonomic classification: BLAST against viral RefSeq, use Kraken2 for rapid classification
- Phylogenetic analysis: Multiple sequence alignment (MAFFT) and tree building (IQ-TREE)
Figure 1: Viral Discovery Metagenomic Workflow. The complete pipeline from sample collection to viral characterization enables comprehensive detection of known and novel viruses.
Case Study: Novel Rhabdovirus Discovery in Nodding Syndrome
A compelling example of NGS-driven viral discovery comes from the identification of a novel rhabdovirus (provisionally named "Mundri virus") in a patient with nodding syndrome [43]. Researchers employed virus discovery cDNA-AFLP next-generation sequencing (VIDISCA-NGS) on patient plasma, generating sequence reads that assembled into a complete novel rhabdovirus genome. Despite this discovery, subsequent case-control analysis revealed no significant association between Mundri virus infection and nodding syndrome, demonstrating how NGS enables both discovery and epidemiological validation [43].
Key Outcomes:
- Full coding sequences obtained for all viral proteins (N, P, M, U1, U2, G, U3, and L)
- Classification as a novel species based on high divergence (<43% amino acid identity to known viruses)
- Development of serological assay (anti-nucleocapsid) to assess population exposure
- Determination that the virus commonly infects children in South Sudan without causal association to the neurological syndrome
Application Note 2: Mutation Rate Estimation and Quasispecies Analysis
Protocol: High-Fidelity Deep Sequencing for Mutation Rate Estimation
Principle: Accurate measurement of viral mutation rates requires extremely high sequencing fidelity to distinguish true biological mutations from technical artifacts [4] [40]. Duplex Sequencing (DS) provides this capability by tagging and sequencing both strands of DNA molecules, achieving error rates below 10â»â· [40].
Workflow for Adenovirus Mutation Rate Estimation [40]:
Viral Clone Purification
- Perform three serial endpoint dilution steps in 96-well plates to isolate viral clones
- Culture in permissive cell lines (HeLa for adenovirus) to expand population
- Execute two serial transfers at high MOI to minimize selective pressures
Viral DNA Extraction
- Harvest virus from cytoplasmic fraction to avoid host nuclear DNA contamination
- Extract DNA using phenol-chloroform with glycogen carrier
- Avoid PCR amplification to prevent introduction of polymerase errors
Duplex Sequencing Library Construction
- Fragment DNA to 200-300 bp fragments via acoustic shearing
- Repair ends and ligate with DS adapters containing unique molecular identifiers
- Size select libraries using double-sided SPRI beads
- Amplify with limited-cycle PCR (4-6 cycles)
Sequencing and Data Analysis
- Sequence on Illumina platform with 2×150 bp chemistry
- Process data using Duplex Sequencing analysis pipeline
- Identify mutation positions supported by both template strands
- Calculate mutation rate using the formula: μ = m / (N × G) where m = number of mutations, N = number of infectious cycles, G = genome size
Table 2: Mutation Rate Estimation for Human Adenovirus 5 Using High-Fidelity Sequencing [40]
| Parameter | Replicate 1 | Replicate 2 | Replicate 3 | Combined |
|---|---|---|---|---|
| Total sequenced bases | 93.2 Mb | 115.7 Mb | 123.7 Mb | 332.6 Mb |
| Single-base substitutions | 68 | 78 | 62 | 208 |
| Mutation frequency | 7.3×10â»â· | 6.7×10â»â· | 5.0×10â»â· | 6.4×10â»â· |
| Estimated mutation rate | 1.5×10â»â· | 1.3×10â»â· | 1.0×10â»â· | 1.3×10â»â· |
Key Findings: The study revealed a mutation rate of 1.3×10â»â· per base per cell infection cycle for adenovirus, significantly lower than RNA viruses and consistent with high replication fidelity and potential post-replicative repair [40]. Researchers observed mutation rate heterogeneity across the genome, with increased probability at GpC dinucleotides and reduced mutations in transcription units L3 and E1B-IVa2 [40].
Protocol: Error-Corrected Sequencing for Viral Quasispecies
Principle: Viral quasispecies represent complex distributions of genetically related variants that require specialized error-correction methods to accurately characterize [4]. Consensus-based approaches using unique molecular identifiers (UMIs) enable distinction between true biological variants and sequencing errors.
Workflow:
Library Preparation with UMIs
- Design reverse transcription primers with random UMIs (8-12 nt) for RNA viruses
- Use high-fidelity polymerases with proofreading capability during amplification
- Employ tiled amplicon approach for complete genome coverage
- Include control templates with known mutation frequencies
Sequencing Strategy
- Sequence on Illumina platform with sufficient coverage (>1000× per amplicon)
- Include spike-in controls to validate detection sensitivity
- Balance read length and quality (2×250 bp for mid-output runs)
Bioinformatic Analysis Pipeline
- UMI clustering and consensus sequence generation
- Reference-based alignment using BWA or Bowtie2
- Variant calling with LoFreq or VarScan2 with minimum frequency threshold of 0.1%
- Linkage analysis for haplotype reconstruction
- Population genetics metrics calculation (diversity, entropy, Fst)
Figure 2: Viral Quasispecies Analysis Workflow. Error-corrected sequencing with unique molecular identifiers enables accurate characterization of minority variants within diverse viral populations.
Application Note 3: Genomic Epidemiology and Outbreak Investigation
Protocol: Whole Genome Sequencing for Outbreak Resolution
Principle: High-resolution whole genome sequencing enables precise identification of transmission pathways during outbreaks by detecting minute genetic differences between isolates [42] [44]. This approach has transformed public health responses to infectious disease threats.
Workflow for Foodborne Outbreak Investigation [44]:
Bacterial Isolation and DNA Preparation
- Culture clinical isolates on selective media (MacConkey for E. coli, XLD for Salmonella)
- Extract high-molecular-weight DNA using automated systems (Maxwell, QIACube)
- Quantify using fluorometry and assess purity (A260/A280 >1.8)
Whole Genome Sequencing
- Use Illumina NextSeq 2000 for routine surveillance with 2×150 bp chemistry
- Target coverage >50× for confident variant calling
- Include quality control standards in each run (positive controls, PhiX)
Bioinformatic Analysis
- De novo assembly using SPAdes or Shovill
- Multilocus sequence typing (MLST) and serotype prediction
- Identification of antimicrobial resistance genes and virulence factors
- SNP-based phylogenetic analysis with recommended thresholds:
- 0-5 SNPs: Highly related, likely same transmission chain
- 5-10 SNPs: Possibly related, requires epidemiological support
- >10 SNPs: Unlikely to be directly related
Data Integration and Reporting
- Integrate phylogenetic analysis with epidemiological data
- Upload genomes to centralized databases (PulseNet, NCBI)
- Generate actionable reports for public health intervention
Impact: The transition to whole genome sequencing in PulseNet has significantly improved outbreak detection sensitivity, allowing identification of previously undetectable clusters and enabling earlier intervention [44]. This approach has been successfully applied to numerous foodborne pathogens including Listeria, Salmonella, E. coli, and Campylobacter [44].
Case Study: Real-Time Genomic Surveillance during Ebola Outbreak
During the 2015 Ebola outbreak in Guinea, researchers demonstrated the power of portable sequencing for real-time outbreak investigation [42]. A complete nanopore sequencing laboratory was transported to the outbreak zone in standard luggage, enabling in-country genomic surveillance without exporting samples.
Key Outcomes [42]:
- 142 Ebola virus genomes sequenced on site, typically within one working day
- Data transmitted to cloud for analysis with results returned within 24 hours
- Actionable information provided for epidemic response despite logistical challenges
- Demonstrated feasibility of portable sequencing in resource-limited settings
Technical Specifications:
- Platform: Oxford Nanopore MinION
- Sample preparation time: <30 minutes
- Sequencing throughput: 100-200 Mb per flow cell
- Analysis: Real-time basecalling and phylogenetic placement
Essential Research Reagents and Computational Tools
Table 3: Research Reagent Solutions for Viral NGS Applications
| Reagent Category | Specific Products | Application | Key Features |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp Viral RNA Mini Kit, MagMAX Viral/Pathogen Kit | Viral nucleic acid purification from clinical samples | Inhibitor removal, low elution volume, high sensitivity |
| Library Preparation | Illumina DNA Prep, Nextera XT, SQK-LSK114 (Nanopore) | Library construction for NGS | Low input requirements, streamlined workflow, compatibility |
| Enzymes | SuperScript IV Reverse Transcriptase, Q5 High-Fidelity DNA Polymerase | cDNA synthesis and amplification | High fidelity, processivity, resistance to inhibitors |
| Target Enrichment | Twist Pan-Viral Panel, SeqCap EZ Choice | Viral sequence enrichment | Comprehensive probe design, high specificity |
| Quality Control | Qubit dsDNA HS Assay, Agilent 4200 TapeStation | Quantification and quality assessment | Sensitivity, accuracy, fragment size distribution |
| Negative Controls | HEK293 DNA, nuclease-free water | Contamination monitoring | Certified DNA-free, process validation |
Computational Resources:
- Quality Control: FastQC, MultiQC, NanoPlot
- Alignment Tools: BWA-MEM, Bowtie2, minimap2
- Variant Callers: LoFreq, VarScan2, FreeBayes
- Visualization: IGV, GGV, Tablet
- Phylogenetics: IQ-TREE, BEAST2, Nextstrain
The application of NGS technologies has fundamentally transformed our approach to viral discovery, mutation rate estimation, and outbreak investigation. Moving beyond simple surveillance, these powerful tools provide unprecedented insights into viral dynamics, evolution, and transmission patterns. The protocols and applications detailed in this document provide researchers with standardized methodologies to investigate viral mutation rates and diversity with high precision, enabling more effective drug and vaccine development strategies.
As sequencing technologies continue to evolve, several emerging trends promise to further enhance these applications. Third-generation sequencing platforms are achieving higher accuracy while maintaining long-read capabilities, and new computational methods are improving the resolution of minority variant detection [39] [4]. The integration of genomic data with epidemiological information through platforms like Nextstrain provides powerful frameworks for real-time outbreak response [42]. For pharmaceutical researchers, these advances translate to improved ability to predict antiviral resistance pathways, design robust vaccine candidates, and develop targeted therapeutics that account for viral evolutionary trajectories.
The future of viral genomics lies in the seamless integration of these technologies into routine public health and clinical practice, enabling a proactive rather than reactive approach to emerging viral threats. By adopting the standardized protocols outlined in this application note, researchers can generate comparable, high-quality data that advances our collective understanding of viral evolution and improves preparedness for future outbreaks.
Optimizing NGS Workflows: Overcoming Technical Challenges and Improving Data Quality
Next-generation sequencing (NGS) has become an indispensable tool for studying viral mutation rates, enabling critical research into drug resistance, vaccine development, and outbreak surveillance. However, the accuracy of NGS-based mutation detection is compromised by errors introduced throughout the sequencing workflow, from initial template preparation to final base calling. These errors are particularly problematic in viral research, where distinguishing true low-frequency mutations from technical artifacts is essential for understanding viral evolution and treatment efficacy. Error-corrected sequencing technologies have emerged as powerful solutions, with methods like duplex sequencing achieving up to a 1000-fold improvement in accuracy compared to standard NGS approaches [45]. This Application Note provides a comprehensive framework for identifying, quantifying, and mitigating NGS error sources specifically within the context of viral mutation rate studies, complete with validated protocols and analytical tools for obtaining reliable mutation data from viral populations.
The journey from viral sample to sequenced data contains multiple potential error sources, each with distinct characteristics and impacts on mutation detection. Understanding these sources is the first step toward developing effective error mitigation strategies.
Template Preparation and Amplification Artifacts
The initial stages of NGS library preparation introduce significant errors, particularly through polymerase mistakes during amplification. Amplification bias can skew variant representation, while PCR errors become fixed in subsequent sequencing rounds, creating false positives that mimic true viral mutations. Studies comparing sequencing methods have demonstrated that template preparation protocols significantly impact observed mutation rates, with heat treatment during DNA extraction increasing per-base mutation rates by approximately 6.8-fold compared to non-heat treatments [46]. The choice of polymerase also critically affects error rates; high-fidelity enzymes like Q5 polymerase demonstrated a 50% reduction in per-base mutation rates compared to standard PlatII polymerase in controlled experiments [46].
Sequencing Chemistry and Platform-Specific Errors
Different NGS platforms exhibit distinct error profiles based on their underlying biochemistry. Illumina's Sequencing-by-Synthesis typically shows low overall error rates (<0.1%) but is prone to substitution errors during nucleotide incorporation and phasing errors in homopolymer regions [47] [46]. Oxford Nanopore Technologies exhibits higher overall error rates (1.3-2.2% in AAV studies) dominated by insertions and deletions, particularly in homopolymer regions, though its duplex sequencing mode can improve accuracy to Q30 (>99.9%) [47] [46]. Pacific Biosciences' HiFi sequencing achieves high accuracy (Q30-Q40) through circular consensus sequencing, which mitigates random errors by repeatedly sequencing the same molecule [47].
Table 1: Quantitative Error Profiles of Major NGS Platforms in Viral Genome Sequencing
| Platform | Chemistry | Per-Base Error Rate | Primary Error Type | Impact on Viral Mutation Studies |
|---|---|---|---|---|
| Illumina | Sequencing-by-Synthesis | 0.013-0.1% [46] | Substitution | False SNVs in viral populations |
| Oxford Nanopore (simplex) | Nanopore sensing | 1.3-2.2% [46] | Insertions/Deletions | Indels in homopolymer regions of viral genomes |
| Oxford Nanopore (duplex) | Dual-strand nanopore | ~0.1% (Q30) [47] | Balanced errors | Improved variant calling in quasispecies |
| PacBio HiFi | Circular consensus | 0.01-0.1% (Q30-Q40) [47] | Random errors | Accurate haplotype reconstruction |
| Sanger (STA-Sanger) | Dideoxy termination | 0.016% [46] | Substitution | Gold standard but low throughput |
Base Calling and Bioinformatic Artifacts
The computational interpretation of raw sequencing data introduces additional error sources. Signal deconvolution errors occur when fluorescent dyes or current signals are incorrectly assigned, particularly in late sequencing cycles as signal quality degrades. Homopolymer compression in pyrosequencing and early nanopore technologies led to inaccurate length determination in repetitive regions common in viral genomes. Algorithmic limitations in variant callers may misclassify technical artifacts as true biological variants, especially at low frequencies. Bioinformatic errors are particularly insidious as they can systematically affect entire datasets and require specialized tools for detection and correction.
Error Correction Methodologies and Experimental Protocols
Several advanced methodologies have been developed specifically to address NGS errors in mutation detection studies. These approaches can be categorized into molecular and computational strategies, with the most effective implementations combining both approaches.
Duplex Sequencing for Ultra-Sensitive Mutation Detection
Duplex sequencing (DS) employs molecular barcoding of both DNA strands to enable error correction, allowing detection of true mutations with frequencies as low as 1×10â»â· [48]. This method is particularly valuable for viral quasispecies analysis, where minority variants comprising less than 1% of the population may have clinical significance for drug resistance.
Table 2: Research Reagent Solutions for Duplex Sequencing in Viral Studies
| Reagent/Equipment | Function | Implementation Example |
|---|---|---|
| Molecular Barcodes (UMIs) | Unique identification of original DNA molecules | Tag both strands of double-stranded viral DNA |
| High-Fidelity Polymerase | Reduces amplification errors during library prep | Q5, KAPA HiFi for viral cDNA amplification |
| Duplex Sequencing Adapters | Specialized adapters with unique molecular identifiers | ONT Q30 Duplex Kit14 [47] |
| Strand-Separation Protocol | Physical separation of complementary strands | Agarose gel extraction or magnetic bead purification |
| Error-Correction Bioinformatics | Computational pipeline for consensus generation | DeepChek Software, CODEC pipeline [14] [45] |
Experimental Protocol: Duplex Sequencing for Viral Mutation Detection
Nucleic Acid Extraction: Extract viral RNA/DNA using non-heat methods with TE buffer as diluent, which has been shown to reduce per-base mutation rates by approximately 69% compared to water-based diluents [46].
Molecular Barcoding:
- Fragment viral nucleic acids to appropriate size (300-500bp for Illumina, longer for nanopore)
- Ligate duplex sequencing adapters containing unique molecular identifiers (UMIs) to both ends of each fragment
- Use uracil-containing adapters to enable enzymatic removal of duplicates
Library Amplification:
- Perform limited-cycle PCR (4-8 cycles) with high-fidelity polymerase
- Validate library quality using TapeStation or similar fragment analyzer
- Target 100-200ng of final library material for sequencing
Sequencing:
- Sequence on appropriate platform (Illumina for maximum depth, Nanopore for long reads)
- Maintain minimum 100x coverage after deduplication for viral genome analysis
Bioinformatic Analysis:
- Group reads by UMIs to identify read families derived from original molecules
- Generate consensus sequences for each family, requiring agreement between both strands
- Call variants only when supported by both strands of original duplex
- Apply additional filters for mapping quality, base quality, and strand bias
CODEC: Concatenating Original Duplex for Error Correction
The CODEC method represents an advanced hybrid approach that combines the throughput of NGS with single-molecule resolution, enabling unprecedented accuracy for detecting ultra-rare mutations in viral populations. This method is particularly valuable for monitoring drug resistance emergence in patients undergoing antiviral therapy.
Experimental Protocol: CODEC Workflow Implementation
Template Preparation:
- Extract viral nucleic acids using silica-column based methods to maximize yield
- Fragment DNA to 200-300bp using controlled enzymatic fragmentation
- Ligate specially designed CODEC adapters containing unique barcodes
Molecule Concatenation:
- Perform intramolecular ligation to create circular molecules
- Amplify using phi29 polymerase for multiple displacement amplification
- Digest with restriction enzymes to linearize concatenated templates
Library Preparation and Sequencing:
- Prepare standard Illumina-compatible libraries
- Sequence with 2x150bp paired-end configuration
- Target minimum 50x coverage for viral genomes
Computational Analysis:
- Identify read pairs derived from same original molecule via barcode matching
- Apply consensus algorithm requiring agreement between technical replicates
- Generate final variant calls with quality scores
The CODEC method has demonstrated capability to detect mutation frequencies as low as 2.72×10â»â¸, making it particularly suitable for identifying extremely rare drug-resistant variants in viral populations [45].
Platform Selection and Validation for Viral Mutation Studies
Selecting the appropriate sequencing platform and implementing rigorous validation protocols are essential for obtaining reliable viral mutation data. The optimal choice depends on the specific research question, variant frequency, and available resources.
Comparative Performance of NGS Platforms
Table 3: Platform Comparison for Viral Mutation Rate Studies
| Platform/Method | Optimal Variant Frequency Range | Key Strengths | Key Limitations | Best Applications in Virology |
|---|---|---|---|---|
| Standard Illumina | >1% | High throughput, low cost per base | Limited sensitivity for rare variants | Dominant variant tracking, consensus sequencing |
| Nanopore (simplex) | >5% | Long reads, real-time analysis | High error rate obscures rare variants | Large structural variations, haplotype phasing |
| Nanopore (duplex) | 0.1-1% | Long reads with improved accuracy | Lower throughput, higher cost | Recombinant detection, complex quasispecies |
| PacBio HiFi | 0.1-1% | High accuracy long reads | Higher input requirements, cost | Complete viral genomes, haplotype-resolved assembly |
| Duplex Sequencing | 0.0001-1% | Ultra-sensitive detection | Complex workflow, high cost | Drug resistance emergence, transmission clusters |
| CODEC | 0.00001-1% | Maximum sensitivity and precision | Very complex protocol | Reservoir characterization, ultra-rare variant detection |
Validation Framework for Viral Mutation Detection
Establishing a rigorous validation protocol is essential for generating clinically or research-relevant viral mutation data. The following framework ensures reliable results:
Control Materials:
- Include synthetic viral sequences with known mutations at predetermined frequencies
- Use well-characterized viral reference materials when available
- Spike-in controls for extraction, amplification, and sequencing steps
Cross-Platform Validation:
- Confirm key findings with at least two independent sequencing methods
- Compare to single-template amplification Sanger sequencing when possible
- Resolve discrepancies with orthogonal methods (e.g., digital PCR)
Limit of Detection (LOD) Determination:
- Establish sample-specific LOD using dilution series of known variants
- Define minimum read depth and variant allele frequency thresholds
- Account for biological and technical variation in LOD calculations
Performance Metrics:
- Monitor standard QC metrics (Q-scores, mapping rates, coverage uniformity)
- Track assay reproducibility through replicate measurements
- Report false positive and false negative rates using control materials
A recent study implementing this approach demonstrated high concordance for majority variants across Illumina, MGI, and Nanopore platforms, though significant variability was observed in minority variant detection (<20%), particularly with Nanopore technology which showed higher numbers of minority mutations [14].
Addressing NGS error sources requires a systematic approach spanning experimental design, wet-lab procedures, and bioinformatic analysis. For viral mutation studies, the following evidence-based recommendations ensure reliable results:
For routine surveillance of dominant viral variants (>5% frequency), standard Illumina sequencing provides the optimal balance of cost, throughput, and accuracy. For drug resistance monitoring where detection of variants at 1-5% frequency is required, Illumina with unique molecular identifiers (UMIs) or nanopore duplex sequencing provide sufficient sensitivity. For characterizing viral reservoirs and detecting ultra-rare variants (<0.1%), advanced error-corrected methods like duplex sequencing or CODEC are necessary, despite their higher complexity and cost.
Implementation of these methods requires careful attention to potential pitfalls: inadequate input material leads to increased amplification artifacts; improper UMI implementation provides false confidence in error correction; and overzealous bioinformatic filtering can eliminate true biological signals. Regular validation using control materials with known mutation profiles is essential for maintaining assay performance. As the field advances, the integration of these error-corrected sequencing approaches into standardized viral surveillance pipelines will enhance our ability to track viral evolution, understand treatment failure, and develop effective countermeasures against emerging viral threats.
The accurate detection of low-frequency mutations is a critical challenge in viral research using next-generation sequencing (NGS). Viral populations often exist as complex mixtures of genetic variants, with key mutations—such as those conferring drug resistance or immune evasion—frequently present at fractions below the detection limit of standard NGS protocols [10]. In standard Illumina sequencing, background error rates of approximately 0.5% per nucleotide obscure true biological variants occurring at lower frequencies, complicating efforts to understand viral evolution, treatment failure, and pathogenicity [49] [50].
Error-corrected NGS (ecNGS) technologies have emerged as powerful solutions, enabling the detection of ultra-rare mutations with frequencies as low as 10â»â· to 10â»âµ per nucleotide [48] [50]. These methods are revolutionizing viral mutation rate research by allowing scientists to track the emergence of resistant variants earlier, characterize mutational spectra with higher resolution, and obtain more accurate measurements of mutation frequencies in viral populations. This Application Note details practical strategies and protocols to enhance sensitivity for detecting low-frequency viral mutations, providing researchers with methodologies essential for advancing viral genomics research and drug development.
Advanced NGS Methodologies for Low-Frequency Detection
Error-Correction Strategies
To overcome the inherent error rates of standard NGS, several sophisticated error-correction strategies have been developed, each with distinct mechanisms and applications for viral genomics research.
Table 1: Error-Corrected NGS Methodologies for Low-Frequency Variant Detection
| Method Category | Example Methods | Core Principle | Theoretical Detection Limit | Key Applications |
|---|---|---|---|---|
| Single-Strand Consensus | Safe-SeqS, SiMSen-Seq [49] [50] | Tags and sequences individual DNA molecules; creates consensus from multiple reads of the same original strand. | VAF ~10â»âµ [50] | General variant detection, viral population sequencing |
| Tandem-Strand Consensus | o2n-Seq, SMM-Seq [49] | Links two complementary strands from the same DNA molecule; calls variants only if present in both strands. | MF ~10â»â· per nt [50] | High-specificity variant calling, eliminating artifacts |
| Parent-Strand Consensus (Duplex Sequencing) | DuplexSeq, NanoSeq, SaferSeq [49] [48] [50] | Tags both strands of the original DNA duplex independently; requires mutation to appear in both complementary strands. | MF <10â»â¹ per nt [49] [50] | Ultralow-frequency mutation detection, gold-standard validation |
Single-strand consensus methods provide a foundational approach to error correction, offering significant improvements over standard NGS. These methods utilize unique molecular identifiers (UMIs) to tag individual DNA molecules before amplification. By comparing multiple sequencing reads derived from the same original molecule, a consensus sequence is generated that filters out random errors introduced during PCR or sequencing [51]. While highly effective, these methods primarily correct for errors occurring after the tagging step.
Duplex sequencing represents the gold standard in error correction, achieving exceptional sensitivity and specificity by tracking both strands of the original DNA duplex independently. This method uses a dual-indexing system where each double-stranded DNA molecule receives a unique double-stranded barcode, enabling bioinformatic reconstruction of the original molecule's sequence. A true mutation is only called if it is present in both complementary strands, while errors (which typically affect only one strand) are discarded [48] [50]. This approach reduces the error rate by several orders of magnitude, enabling detection of mutations at frequencies as low as one per billion nucleotides [49].
Bioinformatic Tools for Variant Calling
The selection of appropriate variant calling algorithms is equally critical for sensitive mutation detection. These tools can be broadly categorized into raw-reads-based and UMI-based callers.
Table 2: Performance Comparison of Low-Frequency Variant Calling Tools
| Variant Caller | Type | Reported Sensitivity (at 0.1% VAF) | Reported Precision/Specificity | Considerations |
|---|---|---|---|---|
| DeepSNVMiner [51] | UMI-based | 88% | 100% | High performance, requires UMI implementation |
| UMI-VarCal [51] | UMI-based | 84% | 100% | High performance, requires UMI implementation |
| MAGERI [51] | UMI-based | Not Detected | 100% | Theoretical detection limit of 0.1% |
| smCounter2 [51] | UMI-based | Low | High | Detection limit of 0.5-1% |
| VarScan2 [52] | Raw-reads-based | 97% (at 1-8% VAF) | >99% PPV (in coding regions) | Good for moderate frequencies |
| LoFreq [51] | Raw-reads-based | Moderate | Moderate | Detects variants as low as 0.05% |
| SiNVICT [51] | Raw-reads-based | Moderate | Moderate | Detects variants as low as 0.5% |
| GATK [52] | Raw-reads-based | >94% (at 10% VAF) | High | Optimal for VAF ≥10% |
UMI-based variant callers generally outperform raw-reads-based callers, particularly at variant allele frequencies (VAFs) below 1% [51]. Tools like DeepSNVMiner and UMI-VarCal demonstrate excellent sensitivity and near-perfect specificity at VAFs as low as 0.1% by leveraging the error-correction capacity inherent in UMI-labeled data [51]. Sequencing depth has minimal impact on the performance of UMI-based callers once a minimum threshold is reached, whereas raw-reads-based callers show significant performance variation with coverage depth [51].
For viral genomics applications where detecting emerging resistant variants is crucial, UMI-based approaches combined with DeepSNVMiner or UMI-VarCal are recommended for optimal sensitivity and specificity. These tools enable reliable detection of variants present in tiny subpopulations of the viral quasispecies, providing early warning of treatment resistance emergence.
Experimental Protocols
Duplex Sequencing Workflow for Viral Genomes
Figure 1: Duplex sequencing workflow for ultra-sensitive viral mutation detection. Key steps include adapter ligation with double-stranded barcodes (DSB) and bioinformatic analysis.
Protocol: Duplex Sequencing for Viral Mutation Detection
Principle: This protocol utilizes double-stranded barcoding to achieve the highest possible sensitivity for detecting ultra-rare mutations in viral populations, with theoretical detection limits below 10â»â¸ errors per nucleotide [48] [50].
Materials:
- High-quality viral DNA/RNA extraction kit
- Duplex sequencing adapter kit (commercially available or custom-synthesized)
- PCR reagents and high-fidelity DNA polymerase
- Next-generation sequencer (Illumina recommended)
- Bioinformatics pipeline supporting duplex sequencing analysis
Procedure:
Nucleic Acid Extraction and Quality Control:
- Extract viral nucleic acids using a high-quality kit optimized for your sample type (clinical specimens, cell culture supernatants, etc.).
- Assess nucleic acid quality and quantity using fluorometry. For RNA viruses, perform reverse transcription to generate cDNA.
- Fragment DNA to ~200-300 bp using acoustic shearing or enzymatic fragmentation.
Adapter Ligation with Double-Stranded Barcodes:
- Ligate duplex sequencing adapters containing random double-stranded barcodes to both ends of fragmented viral DNA.
- These adapters uniquely tag each individual DNA molecule, enabling tracking of both strands through subsequent steps [48].
- Purify the ligation product using SPRI beads to remove excess adapters.
PCR Amplification:
- Amplify the adapter-ligated library using PCR with 8-12 cycles.
- Use a high-fidelity DNA polymerase to minimize introduction of errors during amplification.
- Clean up the PCR product with SPRI beads and quantify the final library by qPCR.
Sequencing:
- Sequence the library on an NGS platform (Illumina recommended for high accuracy).
- Aim for high sequencing depth (>1000X per unique original molecule) to ensure sufficient coverage for consensus building [52].
Bioinformatic Analysis:
- Demultiplexing: Sort reads by sample-specific barcodes.
- Consensus Building: Group reads sharing the same double-stranded barcode into families. Generate single-strand consensus sequences (SSCS) for each family.
- Duplex Consensus: Pair complementary SSCS to create duplex consensus sequences (DCS). Only mutations present in both strands are considered true variants.
- Variant Calling: Align DCS to the reference viral genome and call variants using a sensitive variant caller.
Troubleshooting Notes:
- Low library complexity may indicate insufficient input DNA or inefficient adapter ligation.
- High error rates after consensus building suggest potential issues with barcode design or PCR conditions.
- For viral populations with high mutation rates, adjust variant frequency thresholds accordingly.
UMI-Based Targeted Sequencing Protocol
Protocol: Targeted Sequencing with UMIs for Viral Drug Resistance Mutation Detection
Principle: This protocol uses unique molecular identifiers (UMIs) for error correction in targeted sequencing of specific viral genomic regions, balancing sensitivity with practical implementation for clinical research applications [51].
Materials:
- Viral nucleic acid sample
- UMI-containing adapters (commercially available)
- Target enrichment system (hybridization capture or amplicon-based)
- High-fidelity PCR reagents
- NGS sequencer
Procedure:
Library Preparation with UMI Ligation:
- Fragment viral DNA to appropriate size for your target enrichment method.
- Ligate UMI-containing adapters to both ends of each DNA fragment.
- The UMIs should be sufficiently complex (8-12 random nucleotides) to uniquely tag each original molecule [51].
Target Enrichment:
- Option A - Hybridization Capture: Hybridize the library to biotinylated probes complementary to your target viral regions (e.g., HIV reverse transcriptase, protease, integrase). Capture using streptavidin beads.
- Option B - Amplicon Sequencing: Perform PCR with UMI-compatible primers targeting specific viral regions.
- Clean up the enriched library and perform a limited-cycle PCR to add platform-specific sequencing adapters.
Sequencing and Data Analysis:
- Sequence the library to a depth sufficient for your sensitivity requirements (typically >5000X raw coverage) [52].
- Process the data using a UMI-aware bioinformatic pipeline:
- Group reads by their UMI sequences to create read families.
- Generate consensus sequences for each family.
- Align consensus sequences to the reference genome.
- Call variants using a UMI-aware variant caller such as DeepSNVMiner or UMI-VarCal [51].
Application Note: This approach is particularly valuable for monitoring drug resistance mutations in HIV, where detecting minor variants present at 1-5% can predict treatment failure [10]. The method can be adapted for other viruses with known resistance-associated mutations.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Low-Frequency Mutation Detection
| Reagent/Kit | Function | Application Note |
|---|---|---|
| High-Fidelity DNA Polymerase | Amplification with minimal errors during PCR | Essential for all ecNGS methods to prevent introduction of artifactual mutations during library prep [53] |
| Duplex Sequencing Adapter Kit | Labels both strands of DNA duplex with unique barcodes | Enables highest sensitivity detection; commercially available or custom-synthesized [48] [50] |
| UMI Adapter Kits | Labels individual DNA molecules before amplification | Reduces errors from PCR and sequencing; compatible with various NGS platforms [51] |
| Hybridization Capture Probes | Enriches for specific viral genomic regions | Allows deep sequencing of target genes (e.g., viral polymerase); improves cost-efficiency [52] |
| Reference Standard Materials | Controls with known mutation frequencies | Validates assay performance; Horizon Discovery Tru-Q and OncoSpan are examples [54] |
| Nucleic Acid Preservation Solution | Stabilizes viral nucleic acids in clinical samples | Prevents artifactual mutations from sample degradation; crucial for accurate low-VAF detection |
The strategies outlined in this Application Note provide researchers with powerful methodologies to overcome the fundamental challenge of detecting low-frequency mutations in viral populations. By implementing error-corrected NGS approaches—ranging from practical UMI-based methods to the highly sensitive duplex sequencing protocol—scientists can achieve unprecedented resolution in monitoring viral evolution. The appropriate combination of wet-lab protocols and bioinformatic tools detailed herein enables detection of rare viral variants that are critical for understanding drug resistance mechanisms, viral pathogenesis, and treatment outcomes. These advanced methodologies represent essential tools for researchers and drug development professionals working to advance viral genomics and precision medicine.
Bioinformatics Pipeline Optimization for Accurate Variant Calling
Within viral genomics research, the precise identification of mutations is fundamental to understanding viral evolution, drug resistance, and pathogenicity. Next-generation sequencing (NGS) enables the detection of these variants, but the accuracy of the results is critically dependent on the bioinformatics pipeline that processes the raw data [55]. Variant calling—the process of identifying single-nucleotide polymorphisms (SNPs) and insertions/deletions (indels) from sequencing data—is susceptible to errors introduced during library preparation, sequencing, and data analysis. An unoptimized pipeline can generate false positives or miss true variants, compromising the validity of downstream conclusions. Therefore, systematic optimization is not merely a technical exercise but a prerequisite for generating reliable, reproducible, and actionable data in viral mutation studies, directly impacting the development of diagnostics, therapeutics, and vaccines [7] [56].
Key Optimization Strategies for Variant Calling
Optimizing a bioinformatics pipeline involves refining each stage to maximize accuracy, efficiency, and reproducibility. The following strategies address common challenges and significantly enhance the fidelity of variant calls in viral NGS data.
Table 1: Key Optimization Strategies for Variant Calling Pipelines
| Strategy | Description | Impact on Variant Calling |
|---|---|---|
| Utilizing Unique Molecular Identifiers (UMIs) | Incorporating random nucleotide tags (Primer IDs) during cDNA synthesis to uniquely label each original RNA template [56]. | Dramatically reduces errors from reverse transcription, PCR amplification, and sequencing by generating a consensus sequence from reads sharing the same UMI. Lowers error rates to ~1 in 10,000 nucleotides [56]. |
| Robust Workflow Management | Implementing workflow managers like Nextflow or Snakemake to automate and orchestrate pipeline steps [57] [58]. | Ensures reproducibility, simplifies scaling across large datasets, and manages complex software dependencies, reducing human error and processing bottlenecks [59] [58]. |
| Rigorous Preprocessing & Quality Control | Performing stringent quality checks on raw reads (FastQC) followed by adapter trimming and quality filtering. | Removes low-quality data and technical sequences that cause misalignments, leading to cleaner data and more accurate alignment, the foundation of reliable variant calling. |
| Optimized Computational Resources | Leveraging cloud computing (AWS Batch, Google Cloud) and dynamic resource allocation via tools like Nextflow [59] [58]. | Prevents pipeline failures due to insufficient memory or CPU and enables the processing of large datasets (e.g., 300,000 genomes) efficiently, reducing computation time by up to 70% [59] [58]. |
Experimental Protocol: Primer ID NGS for Viral Mutation Rates
This detailed protocol, adapted from a peer-reviewed method for studying antiviral-induced mutations in coronaviruses, leverages UMIs (Primer IDs) to achieve highly accurate measurement of viral mutation spectra and error rates [56].
Research Reagent Solutions
Table 2: Essential Reagents and Materials for Primer ID NGS Protocol
| Item | Function / Application |
|---|---|
| SuperScript III Reverse Transcriptase | Reverse transcription of viral RNA into cDNA; chosen for high fidelity and efficiency [56]. |
| Primer ID cDNA Primers | Custom primers with a degenerate nucleotide block to tag each RNA template with a unique molecular identifier [56]. |
| KAPA2G Robust / HiFi HotStart PCR Kits | Amplification of cDNA libraries; high-fidelity polymerase minimizes PCR-introduced errors [56]. |
| AMPure XP & RNAClean XP Beads | Solid-phase reversible immobilization (SPRI) for purification and size selection of cDNA and PCR products [56]. |
| MiSeq Reagent Kit v3 (600-cycle) | Sequencing chemistry for Illumina MiSeq platform, enabling paired-end sequencing for better error correction [56]. |
Step-by-Step Procedure
- Primer Design and Synthesis: Design cDNA and PCR primers targeting specific regions of the viral genome (e.g., ORF1b for MERS-CoV) using NCBI Primer-BLAST. The cDNA primer must include a 5' anchor, an 11-base degenerate Primer ID region, and a 3' template-specific sequence [56].
- RNA Extraction and Qualification: Extract viral RNA from cell culture supernatant or infected tissue (e.g., total lung RNA). Quantify RNA using a fluorometric method, noting that viral RNA quantity may be very low.
- Primer ID-tagged cDNA Synthesis:
- Set up a reverse transcription reaction containing viral RNA, Primer ID primers, dNTPs, SuperScript III Reverse Transcriptase, and RNaseOUT.
- Incubate to synthesize cDNA, ensuring each original RNA molecule is labeled with a unique Primer ID.
- Degrade the RNA template with RNase H and purify the first-strand cDNA using RNAClean XP beads [56].
- PCR Amplification of cDNA Libraries:
- Perform a first-round PCR using the purified cDNA as template and primers that bind to the anchor sequence and a nested viral sequence.
- Conduct a second-round PCR to add Illumina sequencing adapters and sample-specific barcodes (e.g., i5 and i7 indices) using a high-fidelity polymerase like KAPA2G HiFi.
- Purify the final PCR product using AMPure XP beads [56].
- Library Qualification and Sequencing:
- Quantify the final library using the Qubit dsDNA BR Assay and assess its size distribution and quality with an Experion DNA 12K chip or similar.
- Dilute the library to the appropriate concentration (e.g., 4 nM) and mix with other barcoded libraries in an equimolar pool.
- Combine the pooled library with the MiSeq reagent kit and a 5-10% spike-in of PhiX control to add base diversity.
- Sequence on the Illumina MiSeq platform using a 2x300 paired-end run [56].
- Bioinformatic Analysis and Template Consensus Sequence (TCS) Generation:
- Demultiplexing: Assign raw sequencing reads to individual samples based on their barcodes.
- Primer ID Processing and TCS Generation: Use a specialized pipeline (e.g., the Template Consensus Sequence web-app) to group raw reads by their unique Primer ID sequence. Generate a consensus sequence for each group of reads that originated from the same original RNA template. This step effectively eliminates most PCR and sequencing errors [56].
- Variant Calling: Align the high-fidelity TCS reads to a reference viral genome and call variants. The resulting mutation profile reflects the true sequence of the original viral population, allowing for accurate calculation of mutation rates and spectra (e.g., identifying an increase in C-to-U transitions after NHC antiviral treatment) [56].
Workflow Visualization
The following diagram illustrates the complete optimized protocol, from wet-lab procedures to bioinformatic analysis.
Diagram 1: Primer ID NGS workflow for accurate viral variant calling.
Implementation and Concluding Remarks
Successfully implementing an optimized pipeline requires careful planning. Begin by selecting a workflow management system like Nextflow, which facilitates reproducibility and portability across different computing environments (local, HPC, cloud) [57] [58]. A phased approach to optimization is recommended: first, integrate the most critical analysis tools (e.g., the TCS generator); second, implement the workflow orchestrator for dynamic resource management; and third, configure a cost-optimized execution environment, often in the cloud [58]. Investing in this optimization early, even if it takes two months, can yield long-term time and cost savings of 30-75% by preventing bottlenecks and inefficient resource use as data scales [58].
In conclusion, accurate variant calling in viral NGS data is not achievable through a single tool but through a holistic, optimized pipeline. The integration of wet-lab methods like Primer ID tagging with a robust, well-managed bioinformatic workflow is paramount. This rigorous approach ensures the high-quality data necessary for reliable insights into viral mutation rates, directly supporting critical research in drug development and pandemic preparedness.
Ensuring Accuracy: Platform Comparisons, Validation Frameworks and Quality Control
Next-generation sequencing (NGS) technologies have revolutionized viral genomics research, enabling rapid characterization of viral genomes, tracking of mutation rates, and identification of emerging variants. For researchers and drug development professionals, selecting the appropriate sequencing platform is crucial for generating reliable data for epidemiological surveillance, therapeutic development, and understanding viral evolution. This application note provides a detailed comparison of three major sequencing platforms—Illumina, Oxford Nanopore, and Ion Torrent—for viral sequencing applications, with a specific focus on generating data for viral mutation rates research.
The technologies differ fundamentally in their underlying biochemistry, performance characteristics, and practical implementation. Illumina employs sequencing-by-synthesis with reversible dye-terminators [5], Oxford Nanopore detects nucleotide sequences through changes in electrical current as DNA strands pass through protein nanopores [5], and Ion Torrent utilizes semiconductor technology to detect hydrogen ions released during DNA polymerization [5]. These fundamental differences translate into distinct performance trade-offs that researchers must consider when designing viral sequencing studies.
Performance Comparison and Platform Selection
Table 1: Key Technical Specifications of Major Sequencing Platforms for Viral Applications
| Parameter | Illumina | Oxford Nanopore | Ion Torrent |
|---|---|---|---|
| Sequencing Chemistry | Sequencing-by-synthesis with reversible dye-terminators [5] | Electrical impedance detection via protein nanopores [5] | Semiconductor detection of H+ ions [5] |
| Typical Read Length | 36-300 bp (short-read) [5] | Average 10,000-30,000 bp (long-read) [5] | 200-400 bp (short-read) [5] |
| Accuracy/Error Rate | High accuracy; >99.9% at Q30 [60] | Higher error rate (~95.84%-96.84% accuracy) [61] | Challenges with homopolymer regions [5] |
| Typical Applications in Viral Research | Viral genome assembly, variant calling, mutation tracking [62] [63] | Rapid screening, full-length viral genome assembly, real-time surveillance [64] [65] | Targeted viral sequencing, variant detection [66] [67] |
| Hands-on Time | Variable depending on system | Lowest among compared platforms [63] | Low with automated systems (e.g., Ion Chef) [67] |
| Run Time | Hours to days | Shortest sequence runtime [63] | 3.5 hours for SARS-CoV-2 WGS [67] |
| Cost Efficiency | High at maximum capacity [67] | Lower cost for rapid analyses [61] | Cost-effective with multiplexed samples [67] |
| Best For | High-accuracy variant calling, reference-grade assemblies | Rapid results, long-range haplotyping, field deployment | Rapid targeted sequencing, clinical research settings |
Table 2: Performance Metrics in Viral Sequencing Studies
| Virus/Application | Illumina Performance | Oxford Nanopore Performance | Ion Torrent Performance |
|---|---|---|---|
| SARS-CoV-2 | 99.8% genome coverage (AmpliSeq protocol) [63] | 81.6% genome coverage (custom protocol) [63] | 99% genome coverage; effective across varied viral loads [67] |
| Clostridioides difficile | 99.68% average read quality (Q25); gold standard for epidemiology [61] | 96.84% average read quality (Q15); suitable for rapid virulence gene detection [61] | Not specifically tested in provided studies |
| Viral Detection Sensitivity | Standard sensitivity | 3-log improvement with specialized prep (CoNS-seq); detects viruses at 0.001 vg per cell [65] | Analyzes samples with viral loads as low as 20 copies [66] |
| SNP Concordance | 99.5% concordance between MiSeq and iSeq for viral SNPs [62] | Higher error rate affects SNP calling accuracy [61] | Lower substitution errors for SNVs reported [66] |
| Workflow Advantages | Equivalent assembly statistics between MiSeq and iSeq enable cost optimization [62] | Real-time basecalling; rapid detection (hours) [65] | Automated workflow with Ion Chef system [67] |
Platform Selection Guidance
For high-resolution epidemiological surveillance requiring maximum accuracy for single nucleotide variant (SNV) calling and mutation rate analysis, Illumina platforms remain the gold standard, with MiSeq and iSeq demonstrating 99.5% SNP concordance in viral sequencing [62]. This high accuracy is crucial for detecting low-frequency variants and precisely calculating mutation rates.
For rapid outbreak investigation and real-time surveillance where speed is prioritized over ultra-high accuracy, Oxford Nanopore technology offers significant advantages with its portability and real-time analysis capabilities, enabling same-day results [65]. The long-read capability additionally enables haplotyping and structural variant analysis that can inform understanding of viral evolution.
For targeted viral sequencing in clinical research settings with limited batch sizes, Ion Torrent provides an attractive solution with fast turnaround times (as low as 3.5 hours) and automated workflows that reduce hands-on time and expertise requirements [67].
Experimental Protocols for Viral Sequencing
Tiled Amplicon Sequencing for Viral Genomes (Illumina and Oxford Nanopore)
The tiled amplicon approach, successfully used for SARS-CoV-2 and hepatitis B virus (HBV) sequencing, enables complete viral genome coverage even from low-titer samples [68].
Protocol Steps:
- Nucleic Acid Extraction: Extract viral RNA/DNA using appropriate kits (e.g., QIAgen MinElute Virus Spin Kit for HBV [68]).
- Reverse Transcription (for RNA viruses): Use SuperScript IV reverse transcriptase with random hexamers (Illumina) or SuperScript VILO cDNA synthesis kit (Ion Torrent) [67].
- Multiplex PCR Amplification: Design primer pools to generate overlapping amplicons (400bp with 70bp overlaps for SARS-CoV-2) using primal scheme tools [67] [68].
- Library Preparation:
- Sequencing: Run on appropriate platform with balanced library pooling based on viral load.
Sensitive Viral Detection with Background Reduction (Oxford Nanopore)
For detecting low-level viral contaminants in gene therapy manufacturing or low viral load clinical samples, the CoNS-seq workflow significantly improves detection sensitivity [65].
Protocol Steps:
- Sample Concentration: Concentrate viral particles from larger sample volumes.
- Nuclease Digestion: Treat with micrococcal nuclease to degrade unprotected host nucleic acids [68].
- Nucleic Acid Extraction: Extract viral nucleic acids using optimized kits.
- Sequence-Independent Single Primer Amplification (SISPA): Amplify viral sequences using agnostic PCR to enrich viral targets [65].
- Library Preparation and Sequencing: Prepare libraries using Oxford Nanopore rapid barcoding kits and sequence on MinION devices.
This approach achieves a three-log improvement in detection sensitivity, enabling virus detection at 0.001 viral genomes per cell [65].
Targeted Viral Panel Sequencing (Ion Torrent)
For focused viral mutation profiling, targeted panels like the Ion AmpliSeq SARS-CoV-2 Insight Research Assay provide optimized workflows [66].
Protocol Steps:
- cDNA Synthesis: Use SuperScript VILO cDNA Synthesis Kit with diluted nucleic acids.
- Targeted Amplification: Employ Ion AmpliSeq SARS-CoV-2 Research Panel with 247 primer pairs covering the viral genome.
- Library Preparation: Utilize Ion AmpliSeq Library Kit Plus with partial primer digestion and adapter ligation.
- Template Preparation: Automate template preparation using Ion Chef system.
- Sequencing: Sequence on Ion GeneStudio S5 Series or Genexus Integrated Sequencer.
This approach generates >98% reads on target and successfully sequences samples with viral loads as low as 20 copies [66].
Research Reagent Solutions
Table 3: Essential Research Reagents for Viral Sequencing
| Reagent/Kit | Function | Compatible Platform(s) | Key Features |
|---|---|---|---|
| AmpliSeq SARS-CoV-2 Research Panel | Targeted viral amplification | Illumina | 247 amplicons; covers >99% of SARS-CoV-2 genome [63] |
| Ion AmpliSeq SARS-CoV-2 Insight Research Assay | Targeted viral sequencing | Ion Torrent | Two primer pools; 125-275bp amplicons; automated workflow [66] |
| Oxford Nanopore Rapid Barcoding Kits (SQK-RBK114-96) | Library preparation | Oxford Nanopore | Fast library prep; multiplexing capability [61] |
| EasySeq RC-PCR SARS-CoV-2 Kit | cDNA synthesis and amplification | Illumina | One-step procedure with adapters and unique dual indices [63] |
| Nextera DNA Flex Library Prep Kit | Library preparation | Illumina | Dual indexing; compatible with amplicon inputs [67] |
| CoNS-seq Workflow Components | Viral enrichment | Oxford Nanopore | Concentration, nuclease digestion, SISPA for sensitivity [65] |
The selection of an appropriate sequencing platform for viral mutation research depends on the specific research questions, throughput requirements, and resource constraints. For large-scale genomic surveillance studies requiring the highest accuracy for detecting low-frequency mutations, Illumina platforms provide the most reliable data, with MiSeq and iSeq demonstrating equivalent assembly statistics for viral genomes [62]. The high base-calling accuracy (Q30 and above) enables confident variant identification essential for mutation rate calculations.
Oxford Nanopore technologies offer distinct advantages for rapid outbreak investigations and applications requiring long-read information for haplotyping or structural variant analysis. While the per-base accuracy is lower, the recent improvements in chemistry and flow cells (R10.4.1) have enhanced performance, and the platform's ability to generate ultra-long reads and provide real-time data makes it invaluable for rapid response scenarios [64]. The portability of MinION devices further enables deployment in field settings for point-of-outbreak sequencing.
Ion Torrent systems strike a balance between speed, automation, and accuracy, making them suitable for clinical research settings processing moderate sample batches. The semiconductor-based sequencing provides rapid turnaround times, and the integrated workflows with Ion Chef automation reduce technical variability [67]. The platform demonstrates excellent coverage uniformity across viral genomes, even from samples with low viral titers [66].
For comprehensive viral mutation studies, a hybrid approach leveraging the strengths of multiple platforms may be optimal—using Oxford Nanopore for rapid screening and Illumina for confirmation of detected variants. As sequencing technologies continue to evolve, improvements in accuracy, read length, and throughput will further enhance our ability to monitor viral evolution and understand mutation mechanisms, ultimately supporting development of more effective therapeutics and vaccines.
The Role of Sanger Sequencing in Confirming NGS Findings
Within viral mutation rate research, next-generation sequencing (NGS) provides unprecedented capacity to detect genetic variations across viral populations. However, the accuracy of critical findings—particularly low-frequency variants that may indicate emerging resistance or altered pathogenicity—requires confirmation by an orthogonal method. Sanger sequencing, long considered the gold standard for accuracy, plays an indispensable role in validating NGS-derived variants before they are reported or used in downstream analyses [69] [70] [71].
This application note details the implementation of Sanger sequencing as a confirmation method within a viral genomics research workflow. It provides validated protocols, quality thresholds, and practical guidance to ensure researchers can confidently verify NGS findings, thereby enhancing the reliability of viral mutation data for research and drug development purposes.
The Necessity of Orthogonal Validation in Viral Research
Limitations of NGS in Viral Mutation Detection
While NGS excels at detecting variants present at frequencies as low as 1%, its accuracy can be compromised in specific scenarios highly relevant to virology [72] [73]. Error sources include:
- Amplification artifacts during library preparation, which are especially pertinent when working with low viral load samples.
- Base-calling inaccuracies in homopolymer regions or sequences with systematic biases.
- Insufficient sequencing depth, leading to unreliable allele frequency estimates for emerging minority variants.
The complexity of viral population dynamics necessitates high confidence in reported mutations. Sanger sequencing provides a complementary technology based on distinct biochemical principles (chain-termination method vs. NGS's sequencing-by-synthesis), making it highly unlikely that both methods would produce the same artifact [74] [71]. This orthogonal validation is crucial for confirming mutations that have significant implications, such as those in viral spike proteins or polymerase genes targeted by therapeutics.
Establishing a Validation Policy
Recent studies indicate that not all NGS-derived variants require Sanger confirmation. A strategic approach involves defining quality thresholds to identify "high-quality" NGS variants that can be reported without orthogonal validation, thereby conserving resources [70].
Table 1: Suggested quality thresholds for determining when Sanger validation is required for NGS-derived viral variants.
| Parameter | Threshold for High-Quality Variants | Variant Requires Sanger Validation? |
|---|---|---|
| Coverage Depth (DP) | ≥ 15-20x [70] | No |
| Allele Frequency (AF) | ≥ 20-25% [70] | No |
| Quality Score (QUAL) | ≥ 100 [70] | No |
| FILTER Field | PASS | No |
| Any parameter below threshold | Any value below thresholds above | Yes |
Adopting this filtering policy can drastically reduce the number of variants requiring confirmation. One large-scale study demonstrated that applying such thresholds reduced the need for Sanger validation to only 1.2-4.8% of the initial variant set while maintaining 100% concordance for the high-quality variants [70].
Experimental Protocol for Sanger Sequencing Validation
This protocol is optimized for confirming viral variants identified through NGS, such as those in the SARS-CoV-2 spike gene or other regions of interest [75].
Sample and Primer Requirements
- Template DNA: Use the same amplified PCR product that was submitted for NGS or a re-amplification from the original sample. Ensure DNA is of high quality and concentration (>10 ng/μL).
- Sequencing Primer: Design a primer that binds 50-100 base pairs upstream of the variant to be confirmed. The primer should have:
- A melting temperature (Tm) of 55-65°C
- Length of 18-25 bases
- No secondary structure or self-complementarity
- Controls: Include a positive control (wild-type sequence) and negative control (no template) in each run.
Step-by-Step Workflow
The Sanger sequencing workflow can be completed in a single day [74] [71].
Diagram 1: Sanger sequencing confirmation workflow. The process from target identification to final validation typically takes 5-8 hours.
PCR Amplification and Clean-up
- Set up PCR reaction:
- Template DNA: 1-10 ng
- Forward and Reverse Primers: 0.5 μM each
- PCR Master Mix: 1X concentration
- Nuclease-free water to 25 μL
- Thermal cycling:
- Initial Denaturation: 94°C for 2 minutes
- 35 cycles of:
- Denature: 94°C for 20 seconds
- Anneal: 60°C for 30 seconds
- Extend: 72°C for 1 minute per kb
- Final Extension: 72°C for 2 minutes
- Hold at 4°C
- PCR clean-up: Use a spin column-based purification kit to remove excess primers and nucleotides. Elute in 20 μL nuclease-free water.
Cycle Sequencing and Clean-up
- Set up sequencing reaction:
- Purified PCR product: 1-5 μL (10-50 ng)
- Sequencing Primer: 1 μL (5 μM)
- Sequencing Master Mix: 2 μL
- Nuclease-free water to 10 μL
- Thermal cycling:
- Initial Denaturation: 96°C for 1 minute
- 25 cycles of:
- Denature: 96°C for 10 seconds
- Anneal: 50°C for 5 seconds
- Extend: 60°C for 2 minutes
- Hold at 4°C
- Sequencing clean-up: Remove unincorporated dye terminators using a spin column, ethanol precipitation, or matrix-based method.
Capillary Electrophoresis and Analysis
- Prepare samples for loading on the genetic analyzer according to instrument specifications.
- Run capillary electrophoresis using appropriate instrument settings.
- Analyze sequence data using software such as Geneious, Sequencher, or Applied Biosystems' Sequencing Analysis Software.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key research reagent solutions for Sanger sequencing confirmation.
| Item | Function | Example Products |
|---|---|---|
| High-Fidelity DNA Polymerase | Amplifies target region with minimal errors | Platinum Taq Polymerase, Q5 Hot Start Polymerase |
| PCR Purification Kit | Removes excess primers and nucleotides after amplification | PureLink PCR Purification Kit, QIAquick PCR Purification Kit |
| Cycle Sequencing Kit | Contains dye-terminator chemistry for sequence reaction | BigDye Terminator v3.1, SeqStudio Sequencing Kit |
| Sequencing Clean-up Kit | Removes unincorporated dye-terminators | BigDye XTerminator Purification Kit, ethanol/EDTA precipitation |
| Genetic Analyzer | Capillary electrophoresis for fragment separation | Applied Biosystems 3500 Series, SeqStudio Genetic Analyzer |
| Sequence Analysis Software | Converts chromatogram data to sequence and identifies variants | Geneious, Sequencher, Sequencing Analysis Software |
Data Interpretation and Quality Assessment
Analyzing Sequence Chromatograms
When validating an NGS-called variant, inspect the chromatogram at the specific genomic position:
- High-confidence confirmation: The base called at the variant position should be clear, with a single distinct peak and low background noise.
- Mixed base call: If the variant is heterozygous or represents a mixed viral population, two overlapping peaks may be visible at the same position. Sanger sequencing can typically detect variants present at >15-20% allele frequency [72] [73].
- Poor-quality sequence: If the chromatogram shows multiple overlapping peaks or high background, repeat the sequencing reaction or redesign the primer.
Concordance Reporting
Document the concordance between NGS and Sanger results for each variant. A well-optimized workflow should achieve >99.7% concordance for variants passing quality thresholds [70]. Maintain detailed records of:
- NGS allele frequency vs. Sanger confirmation status
- Quality metrics for both NGS and Sanger data
- Any discrepancies and their resolution
In viral mutation research, the combination of NGS for comprehensive variant discovery and Sanger sequencing for targeted confirmation creates a robust framework for generating highly reliable genetic data. By implementing the quality thresholds, experimental protocols, and analysis methods outlined in this application note, researchers can validate critical mutations with confidence, ensuring the integrity of data used for understanding viral evolution and guiding therapeutic development.
Quality Metrics and Controls for Reliable Viral Mutation Detection
Next-generation sequencing (NGS) has revolutionized the study of viral evolution by enabling the detection of mutations and minority variants within viral populations. For researchers investigating viral mutation rates, the reliability of these findings is contingent upon implementing stringent, comprehensive quality control (QC) measures throughout the entire NGS workflow. Even minor deviations in protocol or data quality can significantly skew the estimation of mutation frequencies, thereby impacting evolutionary models and the assessment of antiviral resistance. This application note details the essential quality metrics, controls, and experimental protocols required to generate robust and reproducible data for viral mutation rate research, providing a foundational framework for scientific and drug development professionals.
Essential Quality Metrics for Viral NGS
A multi-layered QC strategy is critical for accurate viral mutation detection. Key metrics must be evaluated at each stage of the workflow, from nucleic acid extraction to final bioinformatic analysis. The following table summarizes the core quantitative metrics that define a successful experiment.
Table 1: Essential Quality Metrics for Viral Mutation Detection NGS
| Metric | Definition | Target Value for Viral Mutation Studies | Impact on Mutation Detection |
|---|---|---|---|
| Coverage Depth | Number of times a specific base is sequenced [76]. | >1000X for low-frequency variants [31] [77]. | Increased confidence in SNP and rare variant calling; minimizes stochastic sequencing errors. |
| On-target Rate | Percentage of sequencing reads mapping to the viral target regions of interest [76]. | High percentage (e.g., >70%), specific threshold depends on panel design [76]. | Ensures efficient use of sequencing capacity; low rates may indicate poor enrichment and reduced sensitivity. |
| Duplication Rate | Fraction of mapped reads that are PCR duplicates [76]. | Minimized, ideally <10-20% [76]. | Preents overestimation of coverage and false-positive variant calls from amplification artifacts. |
| Base Quality (Q Score) | Phred-scaled score representing the probability of an incorrect base call [78] [79]. | Q30 (>99.9% accuracy) is standard for most applications [78]. | Directly affects the accuracy of each nucleotide call in the consensus sequence and variant identification. |
| Limit of Detection (LoD) | The lowest viral load at which mutations can be reliably detected [31]. | Must be established empirically; one NGS method reported 17,894.60 IU/mL for HCMV [31]. | Defines the minimum input requirement for the assay and its ability to detect variants in low-titer samples. |
Beyond these core metrics, researchers must also monitor for GC-bias, which causes uneven coverage in GC-rich or AT-rich regions of the viral genome, and Coverage Uniformity (measured by Fold-80 base penalty), which ensures all target regions are sequenced adequately without "drop-outs" [76]. Failure to account for these can lead to missing mutations in specific genomic contexts.
Experimental Protocol for Targeted Viral Sequencing
This protocol, adapted from a validated method for human cytomegalovirus (HCMV), provides a robust framework for targeted viral sequencing to detect mutations and antiviral resistance [31]. The workflow employs a multiplex-PCR approach for DNA enrichment, followed by high-throughput sequencing.
Primer Design and Multiplex PCR Setup
- Primer Design: Design primers to generate 400–800 bp amplicons with overlapping regions to ensure full coverage of the target genes (e.g., UL27, UL54, UL55, UL56, UL89, and UL97 for HCMV). Use tools like Primal Scheme and perform multiple sequence alignment against available genomic data to ensure primers target conserved regions and account for viral diversity. Incorporate degenerate bases if necessary [31].
- Multiplex PCR: Group primer sets into different multiplex reactions to avoid dimerization.
- Reaction Mix: Use a high-fidelity DNA polymerase (e.g., Q5 High-Fidelity DNA Polymerase). The master mix should contain primer pools at a final concentration of 0.08–0.1 µM, 1X reaction buffer, 0.2 mM dNTPs, <10 ng of viral DNA template, 0.02 U/µL polymerase, 1X GC Enhancer, and nuclease-free water to a 25 µL total volume [31].
- Thermocycling Conditions:
- Initial Denaturation: 98°C for 15 min
- 35 Cycles of:
- Denaturation: 95°C for 15 s
- Annealing/Extension: 62°C for 5 min
- Final Extension: 62°C for 5 min
- Hold: 4°C [31]
Library Preparation and Sequencing
- Purify the multiplex PCR amplicons using magnetic beads.
- Prepare sequencing libraries using a platform-specific kit (e.g., Illumina). This typically involves end-repair, adapter ligation, and optional index PCR.
- Quantify the final library using fluorometric methods and assess its size distribution with an instrument such as a Bioanalyzer to confirm the expected fragment size [77].
- Sequence the library on an appropriate high-throughput platform (e.g., Illumina MiSeq) to achieve the desired coverage depth [31].
Quality Control Checkpoints
- Nucleic Acid Input: Assess the quality and quantity of extracted viral RNA/DNA. For RNA, use an RNA Integrity Number (RIN) from systems like Bioanalyzer or TapeStation; a RIN >8 is desirable. For DNA, use a spectrophotometer (A260/A280 ratio ~1.8) or fluorometer [78] [77].
- Post-Amplification: Verify the size profile and yield of the multiplex PCR products using electrophoresis.
- Post-Library Preparation: Confirm the final library has the correct fragment size distribution and concentration before sequencing [77].
- Post-Seencing: Perform initial QC on the raw FASTQ files using tools like FastQC to assess per-base sequence quality, adapter contamination, and GC content [78] [79].
Bioinformatic Analysis and Validation
- Read Trimming and Filtering: Use tools like CutAdapt or Trimmomatic to remove low-quality bases (e.g., quality threshold
[78]. )> - Alignment and Variant Calling: Map the cleaned reads to a reference viral genome. Use variant callers such as VarScan or GATK to identify mutations, setting appropriate thresholds for allele frequency and read depth [77].
- Validation: Validate the entire NGS pipeline using well-characterized reference materials (e.g., wild-type strain AD-169 for HCMV) and compare results to those from an established method like Sanger sequencing. This confirms the assay's ability to accurately detect known mutations and identify low-frequency variants not visible by Sanger [31].
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of the protocol depends on critical reagents and materials. The following table lists essential components and their functions.
Table 2: Essential Research Reagents for Viral NGS Mutation Detection
| Reagent/Material | Function | Example Product/Note |
|---|---|---|
| High-Fidelity DNA Polymerase | Amplifies target viral genomic regions with minimal introduction of errors during PCR. | Q5 High-Fidelity DNA Polymerase (NEB) [31]. |
| Multiplex PCR Primer Pools | Specifically enrich for target viral genes; designed to cover regions of interest (e.g., associated with drug resistance). | Custom-designed primers targeting UL54, UL97, etc.; designed with tools like Primal Scheme [31]. |
| NGS Library Prep Kit | Prepares the amplified DNA fragments for sequencing by adding platform-specific adapters and indexes. | Illumina DNA Prep kits [31]. |
| Standardized Reference RNA/DNA | Acts as a positive control for extraction, amplification, and sequencing; validates variant calls. | Wild-type viral strains (e.g., HCMV AD-169); well-characterized clinical samples [31] [77]. |
| Nucleic Acid QC Kits/Instruments | Accurately quantifies and qualifies input nucleic acids to ensure they meet protocol thresholds. | Agilent TapeStation/Bioanalyzer, Thermo Scientific NanoDrop [78] [77]. |
Implementing the rigorous quality metrics, controls, and detailed protocols outlined in this document is paramount for generating reliable NGS data in viral mutation research. A disciplined approach to quality assurance, from wet-lab procedures to bioinformatic analysis, ensures that observed genetic variations accurately reflect the true biology of the viral population rather than technical artifacts. This foundational reliability is critical for advancing our understanding of viral evolution, drug resistance mechanisms, and for informing the development of effective antiviral therapeutics.
Conclusion
Next-generation sequencing has fundamentally transformed our ability to monitor and understand viral mutation rates, providing unprecedented insights into viral evolution and antiviral resistance mechanisms. The integration of sophisticated NGS methodologies with robust validation frameworks enables researchers and clinicians to detect mutations with high sensitivity and accuracy, directly informing drug discovery and personalized treatment strategies. As the field advances, future developments in long-read sequencing, artificial intelligence-powered bioinformatics, and multi-omics integration promise to further enhance our capabilities. The ongoing challenge remains in standardizing protocols, improving accessibility, and translating these powerful genomic tools into routine clinical practice to combat evolving viral threats and improve patient outcomes globally.
References
- 1. The mutational landscape of SARS-CoV-2 provides new ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12254267/]
- 2. Comparison of genome replication fidelity between SARS ... [https://www.nature.com/articles/s41598-023-40463-4]
- 3. Mutation Rates, Mutation Frequencies, and Proofreading- ... [https://www.mdpi.com/1999-4915/13/9/1882]
- 4. Applying next-generation sequencing to unravel the ... [https://www.sciencedirect.com/science/article/pii/S0168170219308986]
- 5. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 6. Next generation sequencing of multiple SARS-CoV-2 ... [https://www.nature.com/articles/s41598-024-84952-6]
- 7. Viral Metagenomic Next-Generation Sequencing for One ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524960/]
- 8. Choosing the most suitable NGS technology to combine ... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2025.1498921/full]
- 9. Targeted next generation sequencing tracks mutation ... [https://www.idtdna.com/page/support-and-education/decoded-plus/target-enrichment-identifies-mutations-that-confer-fitness-effects/]
- 10. Beyond surveillance: leveraging the potential of next ... [https://www.frontiersin.org/journals/tropical-diseases/articles/10.3389/fitd.2024.1512606/full]
- 11. Comparison of DNA Quantification Methods for Next ... [https://www.nature.com/articles/srep24067]
- 12. A novel statistical method for quantitative comparison of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4542775/]
- 13. Embracing Complexity: What Novel Sequencing Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574701/]
- 14. Advancing Drug Resistance Detection: Comparative ... [https://www.mdpi.com/2813-9038/2/3/14]
- 15. Review Targeted next-generation sequencing (tNGS): an ... [https://www.sciencedirect.com/science/article/pii/S1876034125002850]
- 16. Targeted next-generation sequencing - a promising approach ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12137396/]
- 17. Optimized high-throughput whole-genome sequencing ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01512-x]
- 18. Next-generation sequencing and its clinical application [https://pmc.ncbi.nlm.nih.gov/articles/PMC6528456/]
- 19. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 20. Next-Generation Sequencing Methods to Determine the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11861041/]
- 21. The Swiss HIV cohort study viral next generation sequencing ... [https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000825]
- 22. NGS Data Analysis for Illumina Platform—Overview and ... [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/next-generation-sequencing/ngs-data-analysis-illumina.html]
- 23. The Complete Guide to NGS Data Types and Formats [https://ngs101.com/the-complete-guide-to-ngs-data-types-and-formats-from-raw-reads-to-analysis-ready-files/]
- 24. Gaining deeper insight with targeted sequencing [https://www.pacb.com/blog/gaining-deeper-insight-with-targeted-sequencing/]
- 25. Development and Validation of Ampliconâ€Based Protocol for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365941/]
- 26. Targeted tiled amplicon based protocol for sequencing the ... [https://www.medrxiv.org/content/10.1101/2025.10.15.25338105v1]
- 27. Long-range PCR and Nanopore sequencing for localisation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628991/]
- 28. Scalable long-read nanopore HPV16 amplicon-based ... [https://www.nature.com/articles/s41598-025-18664-w]
- 29. Long Range PCR [https://pcrbio.com/applications/pcr/long-range-pcr/]
- 30. Development of a novel amplicon based whole-genome ... [https://www.nature.com/articles/s42003-025-08159-9]
- 31. A New Nextâ€Generation Sequencing Approach in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308776/]
- 32. Implementation of Next-Generation Sequencing-Based HIV ... [https://microbiologysociety.org/blog/implementation-of-next-generation-sequencing-based-hiv-drug-resistance-testing-enhancing-antiretroviral-treatment-monitoring-and-public-health-outcomes.html]
- 33. Novel cytomegalovirus variants in immunocompromised hosts [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623333/]
- 34. A crossâ€sectional study evaluating the frequency of HIV drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12367864/]
- 35. HIV drug resistance is declining over time [https://www.eatg.org/hiv-news/hiv-drug-resistance-is-declining-over-time/]
- 36. Hybrid next-generation sequencing protocol for testing HIV ... [https://pubmed.ncbi.nlm.nih.gov/39923901/]
- 37. Viral Genome Sequencing With NGS [https://www.thermofisher.com/us/en/home/life-science/sequencing/dna-sequencing/microbial-sequencing/microbial-identification-ion-torrent-next-generation-sequencing/viral-typing.html]
- 38. HIVGenoPipe: a nextflow pipeline for the detection of HIV-1 ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-025-06201-5]
- 39. Viral genome sequencing methods: benefits and pitfalls of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11346438/]
- 40. Genome-Wide Estimation of the Spontaneous Mutation Rate ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1006013]
- 41. Application of next-generation sequencing technologies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3709572/]
- 42. Next Generation Sequencing of Infectious Pathogens - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6682455/]
- 43. Applications of Next-Generation Sequencing in Virus ... [https://www.mdpi.com/journal/viruses/special_issues/next-generation-sequencing-viral-discovery]
- 44. PulseNet Next Generation Technology [https://www.cdc.gov/pulsenet/hcp/about/next-gen-wgs.html]
- 45. New method improves next-generation sequencing ... [https://frontlinegenomics.com/new-method-improves-next-generation-sequencing-accuracy-1000-fold/]
- 46. Quantifying DNA point mutations in commercially available ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12206035/]
- 47. A Primer on NGS Technologies and Their Specs (2025) [https://blog.latch.bio/p/a-primer-on-ngs-technologies-and]
- 48. Error-corrected next-generation sequencing mutagenicity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12477553/]
- 49. Next-generation sequencing methodologies to detect low ... [https://www.sciencedirect.com/science/article/abs/pii/S1383574223000194]
- 50. Next-Generation Sequencing Methodologies To Detect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10843083/]
- 51. Evaluating the performance of low-frequency variant ... [https://www.nature.com/articles/s41598-023-47135-3]
- 52. Performance of Common Analysis Methods for Detecting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3873500/]
- 53. An NGS Workflow Blueprint for DNA Sequencing Data and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4827795/]
- 54. Analysis of Interpret NGS software on low-frequency variants [https://www.ogt.com/resources/ngs-resources-and-support/ngs-resources/assessment-of-interpret-software-on-low-frequency-variants-using-reference-standards/]
- 55. Understanding the Basics of NGS: From Mechanism to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4633438/]
- 56. Primer ID Next - Generation for the Analysis of a Broad... Sequencing [https://bio-protocol.org/en/bpdetail?id=3938&type=0]
- 57. Bioinformatics Pipeline Tools [https://www.meegle.com/en_us/topics/bioinformatics-pipeline/bioinformatics-pipeline-tools]
- 58. Optimizing Bioinformatics Workflows: Why It Matters & ... [https://ardigen.com/optimizing-bioinformatics-workflows-why-it-matters-and-when-to-start-thinking-about-it/]
- 59. Automating and Optimizing Bioinformatics Pipelines [https://ptp.cloud/bioinformatics-pipelines/]
- 60. Sequencing Quality Scores [https://www.illumina.com/science/technology/next-generation-sequencing/plan-experiments/quality-scores.html]
- 61. Comparison of Illumina and Oxford Nanopore sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11783910/]
- 62. Illumina MiSeq and iSeq platforms yield comparable ... [https://www.sciencedirect.com/science/article/pii/S0166093425000953]
- 63. A comparison of five Illumina, Ion Torrent, and nanopore ... [https://link.springer.com/article/10.1007/s10096-023-04590-0]
- 64. Science unlocked: publication picks from May 2025 [https://nanoporetech.com/blog/science-unlocked-publication-picks-from-may-2025]
- 65. A sensitive sample preparation pipeline for adventitious ... [https://www.sciencedirect.com/science/article/pii/S2329050125000737]
- 66. Ion AmpliSeq SARS-CoV-2 Insight Research Assay [https://www.thermofisher.com/us/en/home/life-science/sequencing/dna-sequencing/microbial-sequencing/microbial-identification-ion-torrent-next-generation-sequencing/viral-typing/coronavirus-research.html]
- 67. Reflective Evaluation of Next-Generation Sequencing Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494147/]
- 68. Whole genome sequencing of hepatitis B virus using tiled ... [https://www.nature.com/articles/s41598-025-87721-1]
- 69. Next-Generation Sequencing (NGS) vs. Sanger ... [https://www.labmanager.com/next-generation-sequencing-ngs-vs-sanger-sequencing-which-dna-sequencing-method-is-right-for-you-33659]
- 70. Sanger validation of WGS variants | Scientific Reports [https://www.nature.com/articles/s41598-025-87814-x]
- 71. New to Sanger and NGS Technology [https://www.thermofisher.com/us/en/home/life-science/sequencing/sequencing-learning-center/sequencing-basics/sanger-next-generation-technology.html]
- 72. NGS vs Sanger Sequencing [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-sanger.html]
- 73. Sanger Sequencing vs. Next-Generation Sequencing (NGS) [https://www.cd-genomics.com/resource-sanger-sequencing-vs-next-generation-sequencing.html]
- 74. How to Conduct Sanger Sequencing [https://www.thermofisher.com/us/en/home/life-science/sequencing/sequencing-learning-center/capillary-electrophoresis-information/how-conduct-fragment-analysis0.html]
- 75. A Simplified Sanger Sequencing Method for Detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9689870/]
- 76. Making the Most of Your NGS Data: Understanding Metrics ... [https://sequencing.roche.com/us/en/article-listing/metrics-for-target-enriched-ngs.html]
- 77. Guide to Quality Control for Viral Sequencing [https://www.cd-genomics.com/resource/quality-control-for-viral-sequencing.html]
- 78. How-to: NGS Quality Control [https://frontlinegenomics.com/how-to-ngs-quality-control/]
- 79. Introduction to Next Generation Sequencing (NGS) Data and ... [https://bioinformatics.ccr.cancer.gov/docs/bioinformatics-for-beginners-2025/Module2_RNA_Sequencing/Lesson7/]