Optimizing Molecular Diagnostics for Diabetic Foot: Integrating Biomarkers, Machine Learning, and Novel Targets
This article synthesizes cutting-edge advancements in molecular diagnostics for diabetic foot complications, addressing the critical need for precise, non-invasive tools.
Optimizing Molecular Diagnostics for Diabetic Foot: Integrating Biomarkers, Machine Learning, and Novel Targets
Abstract
This article synthesizes cutting-edge advancements in molecular diagnostics for diabetic foot complications, addressing the critical need for precise, non-invasive tools. We explore the foundational molecular pathways and current diagnostic challenges, including the differentiation between soft tissue infection and osteomyelitis. The review delves into methodological innovations, highlighting the application of explainable machine learning models for biomarker discovery and the validation of novel molecular targets like SCUBE1 and RNF103-CHMP3. We further examine troubleshooting strategies for diagnostic optimization and provide a comparative analysis of emerging technologies against conventional methods. Aimed at researchers, scientists, and drug development professionals, this comprehensive overview aims to bridge the gap between molecular discovery and clinical application, paving the way for improved diagnostic accuracy and personalized therapeutic strategies.
Unraveling Molecular Complexity: Pathophysiology and Current Diagnostic Hurdles in Diabetic Foot
FAQ: Troubleshooting Common Research Challenges
Q1: Our in vitro macrophage polarization assays under high glucose conditions are inconsistent. What are key factors to control?
A: Inconsistent macrophage polarization often stems from poorly defined glycemic conditions and contamination with endotoxins that skew results.
- Solution:
- Standardize Hyperglycemic Media: Prepare glucose solutions fresh and confirm concentrations with a glucometer. Use a stable, high-osmolality control (e.g., mannitol) to rule out osmotic effects.
- Monitor for Endotoxins: Use only cell culture-grade reagents and screen serum for endotoxin levels (<0.01 EU/mL) to prevent unintended activation of inflammatory pathways.
- Validate Polarization States: Do not rely on a single marker. Use a combination for M1 (e.g., CD86, TNF-α, iNOS) and M2 (e.g., CD206, Arg1, IL-10) phenotypes via flow cytometry and RT-qPCR [1].
Q2: When creating a rodent DFU model, how do we distinguish between impaired healing due to neuropathy versus ischemia?
A: Disentangling these contributors requires specific surgical and assessment techniques.
- Solution:
- Employ Selective Procedures: For a pure neuropathy model, use chemical agents like streptozotocin (STZ) and confirm neuropathy via sensory testing (e.g., von Frey filaments). For a combined neuro-ischemic model, follow STZ induction with a precise femoral or iliac artery ligation [1].
- Multimodal Confirmation: Quantify ischemia with laser Doppler perfusion imaging and confirm neuropathy by measuring reduced motor and sensory nerve conduction velocity [2] [3].
- Histological Endpoints: Analyze wound tissue for neuronal markers (e.g., PGP9.5 for nerve density) and vascular markers (e.g., CD31 for endothelial cells) to objectively assess the degree of neural and vascular deficit [1].
Q3: What is the best approach for isolating high-quality RNA from human DFU tissue for transcriptomic studies?
A: DFU tissue is often necrotic, contaminated, and rich in RNases, making RNA integrity a major challenge.
- Solution:
- Rapid Processing: Snap-freeze tissue biopsies immediately in liquid nitrogen and store at -80°C. Avoid multiple freeze-thaw cycles.
- Robust Lysis: Use a commercial lysis buffer containing strong chaotropic salts and β-mercaptoethanol to inactivate RNases. Mechanical homogenization (e.g., bead beating) is essential for complete tissue disruption.
- Quality Control: Always assess RNA Integrity Number (RIN) with a bioanalyzer. Proceed with sequencing or microarray only if RIN > 7.0. Pre-treat samples with RNase inhibitors during collection [4].
Q4: Which machine learning model is most effective for identifying biomarker genes from DFU transcriptomic data?
A: No single model is universally "best"; a consensus approach from multiple algorithms is most robust.
- Solution:
- Apply Multiple Algorithms: Run your dataset through several models, such as LASSO (for feature selection to avoid overfitting), Random Forest (to assess variable importance), and Support Vector Machine-Recursive Feature Elimination (SVM-RFE) [1] [4].
- Identify Consensus Genes: Select genes that are consistently ranked as important across all models for further validation. This was the strategy used to identify core genes like SAMHD1, DPYSL2, SCUBE1, and RNF103-CHMP3 [1] [4].
- Validate Independently: Test the predictive power of your candidate genes on a separate, independent transcriptomic dataset (e.g., from a public repository like GEO) [4].
Core Experimental Protocols
Protocol: Multi-Omics Integration for Biomarker Discovery
This protocol outlines the workflow for identifying core molecular targets by integrating transcriptomic data and machine learning, as employed in recent studies [1] [4].
- Objective: To identify and validate key biomarker genes and potential drug targets for DFU.
- Materials:
- Datasets: Publicly available DFU transcriptome data from GEO (e.g., GSE134431, GSE80178, GSE147890).
- Software: R software with packages:
limma(differential expression),WGCNA(co-expression networks),randomForest,glmnet(LASSO),e1071(SVM),clusterProfiler(enrichment analysis).
- Procedure:
- Data Acquisition & Preprocessing: Download raw data from GEO. Perform background correction, normalization, and batch effect removal.
- Differential Expression Analysis: Using the
limmapackage, identify genes with significant expression changes (e.g., |log2FC| > 1, adjusted p-value < 0.05) between DFU and control samples. - Weighted Gene Co-expression Network Analysis (WGCNA): Construct a co-expression network to identify modules of highly correlated genes. Correlate modules with DFU traits to find the most relevant module.
- Intersection Analysis: Take the intersection of genes from the significant WGCNA module and the differentially expressed genes (DEGs) to obtain a high-confidence gene set.
- Machine Learning Screening:
- Apply LASSO regression to shrink coefficients and select non-redundant features.
- Use Random Forest to rank genes by their importance in classifying DFU.
- Use SVM-RFE to recursively remove features with the smallest ranking criteria.
- Validation: Validate the expression and diagnostic value of the final core genes using ROC curve analysis on an independent test dataset.
- Enrichment Analysis: Perform GO and KEGG pathway analysis on the core gene set to interpret their biological functions.
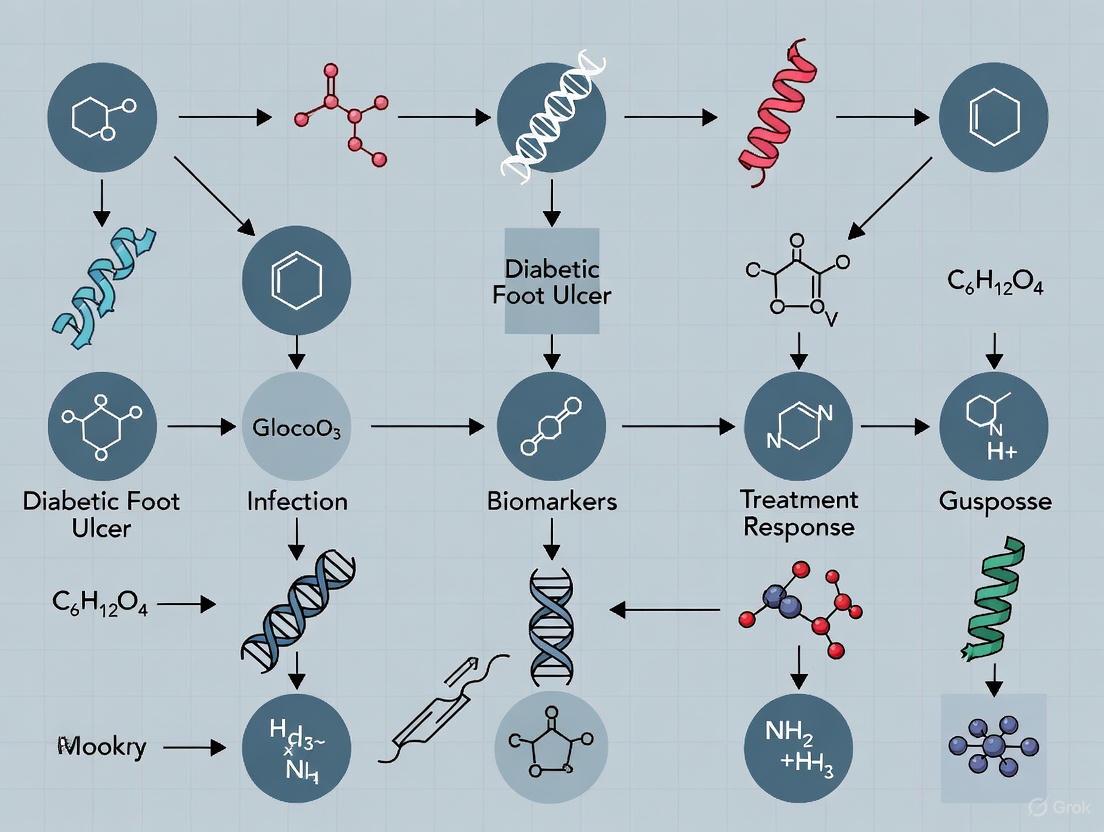
The following diagram visualizes this integrated bioinformatics workflow:
Protocol: Molecular Docking for Therapeutic Compound Screening
This protocol describes how to computationally assess the binding potential of a natural compound like quercetin to proteins encoded by core DFU target genes [1].
- Objective: To evaluate the binding affinity and stability of quercetin with target proteins (e.g., SAMHD1).
- Materials:
- Software: AutoDock Vina, PyMOL, Python.
- Ligand Structure: 3D chemical structure of quercetin (e.g., from PubChem in SDF format).
- Protein Structure: Crystal structure of the target protein (e.g., from Protein Data Bank, PDB).
- Procedure:
- Protein Preparation: Download the PDB file. Remove water molecules and heteroatoms. Add polar hydrogens and compute Gasteiger charges.
- Ligand Preparation: Convert the quercetin SDF to PDBQT format, setting rotatable bonds.
- Grid Box Definition: Define a 3D grid box around the protein's known active site. If the active site is unknown, perform a blind docking over the entire protein surface.
- Molecular Docking: Run the docking simulation in AutoDock Vina. Set the exhaustiveness for accuracy and generate multiple binding poses.
- Analysis: Analyze the output for binding energy (in kcal/mol; lower values indicate stronger binding). Visually inspect the best poses in PyMOL to identify key hydrogen bonds and hydrophobic interactions.
Key Signaling Pathways in DFU Pathogenesis
The following diagram summarizes the core dysfunctional signaling pathways contributing to the pathophysiological triad in DFU, as detailed in the research [2] [3] [5].
Research Reagent Solutions
The following table compiles key reagents, datasets, and software tools essential for researching the DFU pathophysiological triad.
Table 1: Essential Research Resources for Investigating DFU Pathogenesis
| Category | Reagent / Resource | Specific Example / Catalog Number | Primary Function in DFU Research |
|---|---|---|---|
| Transcriptomic Data | GEO Datasets | GSE80178, GSE134431, GSE147890 [1] | Provide human DFU gene expression profiles for bioinformatics analysis and biomarker discovery. |
| Single-Cell Data | GEO Datasets | GSE165816, GSE223964 [1] | Enable cell-type-specific resolution of gene expression in DFU, crucial for understanding immune and endothelial contributions. |
| Machine Learning Tools | R Packages | randomForest, glmnet, e1071 [1] [4] |
Identify key biomarker genes from high-dimensional transcriptomic data and build diagnostic classifiers. |
| Bioinformatics Suites | R Packages | limma, WGCNA, clusterProfiler [1] [4] |
Perform differential expression, co-expression network analysis, and functional enrichment. |
| Molecular Docking | Software Suite | AutoDock 1.5.7, PyMOL [1] | Simulate and visualize interactions between potential therapeutic compounds (e.g., quercetin) and target proteins. |
| Validated Core Targets | Protein/Gene Targets | SAMHD1, DPYSL2 [1] | Macrophage-modulating targets implicated in quercetin's therapeutic mechanism; require antibodies for IHC/IF validation. |
| Validated Core Targets | Protein/Gene Targets | SCUBE1, RNF103-CHMP3 [4] | Biomarkers associated with immune cell infiltration and extracellular matrix interactions; potential diagnostic targets. |
| Animal Modeling | Chemical Inducer | Streptozotocin (STZ) [1] | Induces hyperglycemia in rodent models, replicating the metabolic dysfunction central to DFU development. |
Quantitative Data Synthesis
The following tables consolidate key quantitative findings from recent omics and experimental studies to facilitate comparison and hypothesis generation.
Table 2: Core Biomarker Genes Identified via Machine Learning in DFU Studies
| Gene Symbol | Log2FC Trend in DFU | Proposed Primary Function | Associated Cell Types | Identification Method |
|---|---|---|---|---|
| SAMHD1 | Upregulated | Macrophage modulation; putative quercetin target [1] | Macrophages [1] | WGCNA + RF, Lasso, XGBoost, SVM [1] |
| DPYSL2 | Upregulated | Macrophage & vascular endothelial cell modulation [1] | Macrophages, Vascular Endothelial Cells [1] | WGCNA + RF, Lasso, XGBoost, SVM [1] |
| SCUBE1 | Downregulated (post-cure) | Immune regulation; inflammatory response [4] | NK Cells, Macrophages [4] | LASSO + SVM-RFE [4] |
| RNF103-CHMP3 | Downregulated (post-cure) | Extracellular interactions; vesicular trafficking [4] | NK Cells, Macrophages [4] | LASSO + SVM-RFE [4] |
Table 3: Key Pathophysiological Pathways and Their Molecular Mediators in DFU
| Pathway / Process | Key Molecular Mediators | Experimental Evidence | Functional Consequence |
|---|---|---|---|
| Polyol Pathway | Aldose Reductase, Sorbitol Dehydrogenase, Fructose [2] [3] | Increased flux in hyperglycemia; NADPH depletion; oxidative stress [2] [3] | Neuronal damage, impaired nerve conduction [2] [3] |
| PKC Activation | Diacylglycerol (DAG), PKC-β, PKC-δ isoforms [2] | Increased DAG in vascular tissue; altered gene expression [2] | Vascular dysfunction, reduced blood flow, angiogenesis defects [2] |
| AGE/RAGE Signaling | Advanced Glycation End-products (AGEs), RAGE receptor [2] [5] | Binds RAGE, increasing inflammatory mediators and ROS [2] | Sustained inflammation, nerve & vascular damage [2] [5] |
| Immune Cell Dysregulation | Macrophages (M1/M2 imbalance), Neutrophils, IL-17 [1] [2] | Single-cell RNA-seq shows specific expression of core genes in macrophages; impaired phagocytosis [1] [2] | Failure to resolve inflammation, chronic non-healing wounds [1] [2] |
FAQ: What are the key host inflammatory markers for differentiating osteomyelitis from soft tissue infection, and what are their diagnostic thresholds?
The Erythrocyte Sedimentation Rate (ESR) is a central host inflammatory marker for this differentiation. A recent meta-analysis provides clear quantitative thresholds for its use in diagnostic workflows, particularly for diabetic foot osteomyelitis (DFO).
Table 1: Diagnostic Performance of ESR for Diabetic Foot Osteomyelitis
| ESR Cutoff Value (mm/h) | Sensitivity | Specificity | Recommended Use Case |
|---|---|---|---|
| 51.6 | 80% | 67% | Optimal pooled cutoff for preliminary screening [6] |
| 70.0 | 61% | 83% | Higher specificity; recommended by IWGDF for screening DFO [6] |
Troubleshooting Guide: If your experimental results using these thresholds show high sensitivity but low specificity, consider the following:
- Patient Factors: Be aware that ESR is a nonspecific marker. Conditions like rheumatoid arthritis or other inflammatory states can cause elevated ESR independent of infection [7].
- Integrated Diagnosis: ESR should not be used in isolation. Combine quantitative ESR data with other evidence, such as a positive "probe-to-bone" test or imaging findings, to increase diagnostic certainty [8] [7].
FAQ: What are the primary bacterial immune evasion strategies specific to osteomyelitis?
The pathogen Staphylococcus aureus utilizes distinct molecular mechanisms to persist in bone that are less relevant in soft tissue infections. Understanding these is key to developing targeted diagnostics and therapies.
Key Mechanisms:
- Biofilm Formation: Bacteria encase themselves in a protective matrix on bone and implants, conferring resistance to antibiotics and immune cells [9].
- Intracellular Persistence: S. aureus can survive inside non-professional phagocytes, such as osteoblasts, creating a protected reservoir [10] [9].
- Invasion of the Osteocyte Lacuno-Canalicular Network (OLCN): This is a critical differentiator. S. aureus can invade the microscopic canalicular network that houses osteocytes, using the dense bone matrix as a physical barrier to evade the host immune system. This mechanism explains the persistent and recurrent nature of chronic osteomyelitis [9].
FAQ: How does the host's metabolic immune response differ between soft tissue and bone infections?
Single-cell RNA sequencing (scRNA-seq) studies reveal that metabolic reprogramming of immune and structural cells is a hallmark of non-healing diabetic foot ulcers (DFUs) and is central to the pathogenesis of osteomyelitis.
Key Metabolic Signatures: Research identifies three interconnected metabolic states in DFUs: hypoxia, glycolysis, and lactylation [11]. The shift to glycolysis in macrophages (M1 phenotype) and accumulation of lactate drives histone lactylation, which regulates pro-inflammatory gene expression [11] [12].
Differentiating Workflow: The diagram below outlines a protocol to characterize these metabolic differences in patient samples.
Experimental Protocol: Metabolic State Characterization via scRNA-seq
- Sample Acquisition & Preparation: Obtain foot skin samples from healthy non-diabetic individuals and patients with non-healing DFUs (with and without suspected osteomyelitis). Process tissue into single-cell suspensions [11].
- scRNA-seq Library Construction: Use the 10x Genomics platform for droplet-based single-cell capture. Generate raw count matrices for all samples [11].
- Quality Control & Normalization: Filter out cells with <200 or >6,000 detected genes or >10% mitochondrial gene content. Log-normalize the filtered gene-cell matrix [11].
- Data Integration & Clustering: Perform PCA-based dimensionality reduction. Use the Louvain algorithm for cell clustering and annotate cell types (e.g., keratinocytes, fibroblasts, macrophages) using canonical markers [11].
- Metabolic Signature Scoring: Calculate single-cell enrichment scores for hypoxia, glycolysis, and lactylation gene sets using the AUCell R package (v1.28.0) [11].
- Downstream Analysis:
- Perform KEGG/GO enrichment analysis to identify dysregulated pathways.
- Conduct pseudotime trajectory analysis using Monocle3 (v1.3.7) to map metabolic shifts during disease progression [11].
FAQ: How can I model the macrophage polarization imbalance that contributes to bone destruction in osteomyelitis?
The persistence of pro-inflammatory M1 macrophages over anti-inflammatory M2 macrophages drives chronic inflammation and bone resorption in osteomyelitis. This polarization is directly regulated by mitochondrial metabolism [12].
Molecular Mechanisms:
- M1 Macrophages (Pro-inflammatory): Rely on glycolysis. HIF-1α upregulates GLUT1 and hexokinase 2. A disrupted TCA cycle leads to accumulation of succinate, which stabilizes HIF-1α and promotes ROS production, creating a pro-inflammatory feedback loop [12].
- M2 Macrophages (Anti-inflammatory): Rely on oxidative phosphorylation (OXPHOS) and fatty acid oxidation (FAO) for energy. An intact TCA cycle and glutamine metabolism support anti-inflammatory gene expression [12].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Studying Metabolic Regulation in Osteomyelitis
| Reagent / Assay | Function in Experiment | Key Molecular Targets |
|---|---|---|
| AUCell R Package | Calculating single-cell metabolic enrichment scores from scRNA-seq data [11] | Hypoxia, glycolysis, and lactylation gene sets |
| Seurat R Package | scRNA-seq data processing, normalization, clustering, and cell type annotation [11] | Canonical cell markers (e.g., CD86 for M1, CD163 for M2) |
| Monocle3 | Pseudotime trajectory analysis to model cellular state transitions [11] | Gene expression changes over inferred time |
| Anti-HIF-1α Antibody | Inhibiting/Detecting key regulator of M1 glycolysis and inflammation [12] | Hypoxia-Inducible Factor 1-alpha (HIF-1α) |
| 2-Deoxy-D-Glucose (2-DG) | Glycolysis inhibition to shift polarization from M1 to M2 [12] | Hexokinase |
| Recombinant IL-4 | Polarizing macrophages toward M2 phenotype in vitro [12] | IL-4 Receptor |
| RANKL | Stimulating osteoclast differentiation in co-culture models [12] | Receptor Activator of NF-κB Ligand |
Frequently Asked Questions (FAQs) for Diagnostic Challenges in Diabetic Foot Osteomyelitis Research
FAQ 1: What are the specific clinical limitations of percutaneous bone biopsy for diagnosing diabetic foot osteomyelitis (DFO)?
While bone biopsy with culture is the reference standard for identifying causative pathogens in DFO, its clinical application faces several limitations [13] [14]:
- Invasiveness and Patient Risk: The procedure is invasive, requiring a needle to be inserted into the bone, which can cause pain, carries a risk of infection, bleeding, or potential injury to surrounding structures, and may be contraindicated in patients with certain bleeding disorders [15].
- Feasibility and Access: The procedure is perceived as cumbersome and too invasive for widespread routine use, which limits its application in clinical practice [13] [14].
- Diagnostic Delays: Final culture results can take between five to seven days, delaying the initiation of targeted therapy [15].
FAQ 2: How does the microbiological concordance between deep tissue cultures and bone biopsy impact diagnostic reliability?
A 2025 comparative diagnostic study found only moderate concordance between deep tissue and bone biopsy cultures [13].
- The overall concordance rate was 51.8%.
- Concordance was highest for Staphylococcus aureus (44.4%) but substantially lower for Gram-negative bacteria (31.9%) and other Gram-positive microorganisms (24.2%).
- In 16.5% of cases, bone cultures were positive when deep tissue cultures were negative, indicating a significant rate of potential false negatives if relying solely on deep tissue sampling [13].
FAQ 3: What are the key specificity challenges with MRI in diagnosing DFO?
MRI, while excellent for detecting bone marrow edema, faces specificity challenges because it cannot always distinguish between infection (osteomyelitis) and other non-infectious inflammatory conditions that cause similar fluid shifts and edema, such as Charcot neuro-osteoarthropathy, recent surgery, or traumatic fractures [14].
FAQ 4: What are the analytical limitations of molecular diagnostics like PCR and Whole Genome Sequencing (WGS) for pathogen detection?
Molecular methods, despite their speed, can have a higher limit of detection (LOD) for heteroresistant infections (mixed drug-susceptible and resistant populations) compared to phenotypic culture methods [16].
- A 2024 study on Mycobacterium tuberculosis heteroresistance demonstrated that the agar proportion method (a phenotypic gold standard) could detect a resistant minority population at a proportion of 1%.
- In comparison, the LOD was 10% for both WGS and GeneXpert MTB/RIF Ultra, and 60% for the standard GeneXpert MTB/RIF assay [16]. This indicates that low levels of resistant pathogens might be missed by molecular assays.
FAQ 5: How is artificial intelligence (AI) being applied to address diagnostic challenges in diabetic foot care?
AI and machine learning are showing promise in several areas to complement existing diagnostics [17] [18] [19]:
- Automated Wound Assessment: Deep learning models can segment and classify tissues in diabetic foot ulcer images (e.g., granulation, necrosis, gangrene) with high accuracy, aiding in standardized Wagner grading [18].
- Risk Stratification: Machine learning models analyze biomechanical data from wearable insoles or thermal images to stratify patients based on ulceration risk, enabling early intervention [19].
- Improving Specificity: AI algorithms are being developed to integrate multiple data types (e.g., images, biomechanics, biomarkers) to improve diagnostic specificity beyond what a single modality like MRI can achieve alone [17].
Troubleshooting Guides
Problem 1: Low Concordance Between Deep Tissue and Bone Biopsy Cultures
| Potential Cause | Solution | Rationale |
|---|---|---|
| Polymicrobial Infection | Use molecular methods (e.g., 16S rRNA PCR) on the bone sample to identify fastidious or difficult-to-culture organisms missed by standard cultures. | Deep tissue cultures may not accurately represent the true pathogen profile within the bone, particularly for Gram-negative and polymicrobial infections [13]. |
| Sampling Through Ulcer Bed | Ensure percutaneous bone biopsy is obtained through aseptic skin adjacent to the ulcer, not through the ulcer bed itself. | Sampling through the ulcer bed can capture colonizing bacteria that are not the true causative pathogens of the osteomyelitis, leading to misleading results [14]. |
| Prior Antibiotic Use | Obtain cultures before initiating or after a sufficient washout period of antibiotic therapy. | Even sub-therapeutic antibiotic levels can suppress bacterial growth in cultures, yielding false-negative results. |
Problem 2: Differentiating Osteomyelitis from Charcot Neuro-osteoarthropathy on MRI
| Potential Cause | Solution | Rationale |
|---|---|---|
| Overlapping Imaging Features | Correlate MRI findings with clinical signs (e.g., presence of an open wound, probing to bone, local inflammation) and serologic markers (e.g., ESR, CRP). | Both conditions can present with bone marrow edema, joint effusions, and soft tissue swelling on MRI. Clinical context is essential for accurate interpretation [14]. |
| Lack of Specific Sequences | Utilize advanced sequences like Diffusion-Weighted Imaging (DWI) and Dynamic Contrast-Enhanced (DCE) perfusion. | Research suggests these sequences may help differentiate infected bone from neuropathic edema by assessing tissue cellularity and vascularity, though they are not yet universally standardized for this purpose. |
Problem 3: Molecular Diagnostic Results Do Not Align with Phenotypic Culture/Susceptibility
| Potential Cause | Solution | Rationale |
|---|---|---|
| Heteroresistance | Use a phenotypic reference method (e.g., agar proportion method) to confirm the presence of a resistant subpopulation. | Molecular tests may fail to detect resistant subpopulations that are below their limit of detection (LOD), leading to a discrepancy where culture shows resistance but molecular methods indicate susceptibility [16]. |
| Silent Mutations | Perform functional assays to confirm the phenotypic impact of any genetic mutations identified. | Not all genetic mutations detected by sequencing confer an actual change in antibiotic susceptibility. |
| Contamination | Strictly adhere to sterile sampling techniques and include negative controls in molecular workflows. | Contaminating DNA during sample collection or processing can lead to false-positive results in highly sensitive molecular assays. |
Table 1: Microbiological Concordance Between Deep Tissue and Bone Biopsy Cultures in DFO Diagnosis (n=107) [13]
| Metric | Result |
|---|---|
| Overall Concordance | 51.8% |
| Concordance for Staphylococcus aureus | 44.4% |
| Concordance for Gram-negative bacteria | 31.9% |
| Concordance for other Gram-positive microorganisms | 24.2% |
| Pathogens isolated only from deep tissue | 21.2% |
| Pathogens isolated only from bone (missed by deep tissue) | 16.5% |
Table 2: Limit of Detection (LOD) Comparison for Heteroresistance Identification [16]
| Diagnostic Method | Limit of Detection (LOD) for Minority Resistant Population |
|---|---|
| Agar Proportion Method (Phenotypic Gold Standard) | 1% |
| Whole Genome Sequencing (WGS) | 10% |
| GeneXpert MTB/RIF Ultra | 10% |
| GeneXpert MTB/RIF | 60% |
Table 3: Performance of Deep Learning Models in DFU Image Segmentation and Classification [18]
| Model | Mean Intersection over Union (IoU) | Wagner Grade Classification Accuracy | Area Under the Curve (AUC) |
|---|---|---|---|
| Mask2Former | 65% | 91.85% | 0.9429 |
| Deeplabv3plus | 62% | Not Reported | Not Reported |
| Swin-Transformer | 52% | Not Reported | Not Reported |
Experimental Protocols
Protocol 1: Percutaneous Bone Biopsy for Microbiological Culture in DFO
This protocol is based on the methodology described in the BeBoP randomized controlled trial [14].
1. Pre-Procedure Preparation:
- Imaging Guidance: Identify the site of infected bone using MRI, FDG-PET/CT, or plain X-ray.
- Patient Assessment: Check blood coagulation parameters and adjust anticoagulant medication if necessary. Obtain informed consent [15].
- Anesthesia: Use local anesthesia at the biopsy site. Conscious sedation may be considered based on patient need.
2. Biopsy Procedure:
- Aseptic Technique: Sterilize a wide area of skin surrounding the biopsy site.
- Biopsy Needle: Use an 11-gauge or similar bone biopsy needle.
- Sampling Path: Insert the needle through intact, anesthetized skin adjacent to the ulcer. Do not pass the needle through the ulcer bed to avoid contamination with colonizing flora [14].
- Sample Collection: Obtain a core sample of the bone lesion.
- Sample Handling: Aseptically divide the bone sample. Place one portion in a sterile container for microbiological culture and another in a separate container for molecular analysis (if planned).
3. Post-Procedure Care:
- Apply pressure to the site to prevent bleeding and cover with a sterile bandage.
- Monitor the patient for several hours for potential complications.
- Transport the sample immediately to the microbiology laboratory.
Protocol 2: Deep Learning-Based Segmentation of Diabetic Foot Ulcer Images
This protocol is adapted from a 2025 study that achieved a mean IoU of 65% using the Mask2Former model [18].
1. Data Curation and Preprocessing:
- Image Collection: Collect a dataset of DFU images from patient records. Ensure images have sufficient resolution and clarity.
- Expert Annotation: Have experienced clinicians manually annotate (label) the images using software like Labelme. Annotations should include:
- Ulcer boundary
- Periwound erythema
- Internal wound components: granulation tissue, necrotic tissue, exposed tendon, exposed bone, gangrene.
- Data Standardization: Resize all images to a uniform dimension (e.g., 1024x1024 pixels) using bilinear interpolation.
- Data Augmentation: Apply transformations to increase dataset size and model robustness, including:
- Brightness and contrast adjustment
- Horizontal and vertical flipping
- Image transposition
2. Model Training and Validation:
- Model Selection: Choose an instance segmentation model such as Mask2Former, Deeplabv3plus, or Swin-Transformer. Pre-trained weights from ImageNet are recommended as a starting point.
- Dataset Splitting: Randomly split the annotated dataset into a training set (e.g., 80%) and a test set (e.g., 20%).
- Model Fine-Tuning: Train (fine-tune) the selected model on the DFU training dataset. Monitor the loss function and accuracy on both training and test sets to avoid overfitting.
- Performance Evaluation: Use the held-out test set to evaluate the final model's performance using metrics such as Intersection over Union (IoU), Dice coefficient, accuracy, and Area Under the Curve (AUC).
Diagnostic and Research Workflow Visualization
DFO Diagnostic Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for DFO Diagnostic Studies
| Item | Function/Application in Research |
|---|---|
| 11-Gauge Bone Biopsy Needle | For percutaneous collection of bone specimens for both microbiological and molecular analysis [14]. |
| Mannitol Salt Agar (MSA) | A selective growth medium used for the isolation of Staphylococcus aureus from clinical samples [20]. |
| HiCrome-Rapid MRSA Agar | A chromogenic medium for the selective and differential identification of methicillin-resistant Staphylococcus aureus (MRSA) [20]. |
| Primers for mecA and nuc genes | Essential reagents for multiplex PCR to genetically confirm the presence of S. aureus and its methicillin resistance gene [20]. |
| Labelme Software | An open-source tool for manual annotation and segmentation of diabetic foot ulcer images to create ground-truth datasets for AI model training [18]. |
| Pre-trained Deep Learning Models (e.g., Mask2Former) | Neural network architectures with weights pre-trained on large public datasets (e.g., ImageNet), which can be fine-tuned for specific medical image segmentation tasks, reducing required data and training time [18]. |
| Multiplex PCR Panels | Molecular diagnostic kits capable of simultaneously detecting a syndromic panel of common bacterial pathogens and antibiotic resistance genes from a single sample [21]. |
Diabetic foot osteomyelitis (DFO) is a common and severe complication of diabetic foot infections, present in approximately 20% of patients with diabetic foot infections and 50% of those with severe infections [6]. Its timely and accurate diagnosis is critical for preventing catastrophic outcomes, including lower-limb amputation. In the context of optimizing molecular diagnostic patterns for diabetic foot research, conventional clinical tools like the Probe-to-Bone (PTB) test and Erythrocyte Sedimentation Rate (ESR) measurement remain foundational. They serve as rapid, accessible first-line tests that can guide the need for more advanced (and often more costly and invasive) molecular and imaging diagnostics. This technical support document provides researchers and drug development professionals with a rigorous, evidence-based framework for implementing and evaluating these conventional tools within their experimental and diagnostic workflows.
Diagnostic Performance at a Glance
The following tables summarize the aggregated diagnostic accuracy data for the Probe-to-Bone test and Erythrocyte Sedimentation Rate, providing a quick reference for expected performance metrics.
Table 1: Diagnostic Accuracy of the Probe-to-Bone Test for Diabetic Foot Osteomyelitis
| Metric | Pooled Value (95% CI) | Study Context |
|---|---|---|
| Sensitivity | 0.87 (0.75 - 0.93) [22] | Systematic Review & Meta-Analysis |
| Specificity | 0.83 (0.65 - 0.93) [22] | Systematic Review & Meta-Analysis |
| Positive Predictive Value | 0.57 [23] | Cohort with 12% OM prevalence |
| Negative Predictive Value | 0.98 [23] | Cohort with 12% OM prevalence |
| Positive Likelihood Ratio | 4.41 [24] | Validation against bone histology |
| Negative Likelihood Ratio | 0.02 [24] | Validation against bone histology |
Table 2: Diagnostic Accuracy of ESR for Diabetic Foot Osteomyelitis
| Metric | Value | Context / Model |
|---|---|---|
| Area Under the Curve (AUC) | 0.71 [6] | Hierarchical Summary ROC (HSROC) Model |
| Summary Sensitivity | 0.76 [6] | HSROC Model |
| Summary Specificity | 0.73 [6] | HSROC Model |
| Optimal Pooled Cutoff | 51.6 mm/h [6] | DICS Model (Youden Index) |
| Sensitivity at 51.6 mm/h | 0.80 [6] | DICS Model |
| Specificity at 51.6 mm/h | 0.67 [6] | DICS Model |
| Sensitivity at 70 mm/h | 0.61 [6] | GLMM Prediction |
| Specificity at 70 mm/h | 0.83 [6] | GLMM Prediction |
| Accuracy Designation | "Fair" [25] | ROC AUC 0.70 (95% CI: 0.62-0.79) |
Detailed Experimental Protocols
Probe-to-Bone Test Protocol
The following workflow outlines the standardized procedure for performing and validating the Probe-to-Bone test, based on a prospective study using bone histology as the reference standard [24].
Objective: To clinically diagnose osteomyelitis in a diabetic foot ulcer by detecting exposed bone [24].
Materials:
- Sterile, blunt metal probe (e.g., surgical instrument)
- Sterile saline and gauze
- Personal protective equipment (PPE)
Step-by-Step Procedure:
- Patient Preparation: Position the patient comfortably. Explain the procedure.
- Ulcer Cleaning: Briefly clean the ulcer surface with sterile saline and gauze to remove debris and exudate [24].
- Probing Technique: Using the sterile blunt probe, gently explore the base of the ulcer and any associated sinus tracts. Apply minimal pressure [24].
- Interpretation: The test is considered positive if a hard, gritty, non-give surface—assumed to be bone—is palpated. The test is negative if no such hard surface is encountered [24] [23].
- Documentation: Record the finding in the patient's record. A positive test should trigger a referral for confirmatory testing.
Key Validation Data: In a study of 132 wounds with a high prevalence (79.5%) of osteomyelitis confirmed by bone histology, the PTB test demonstrated an efficiency of 94%, sensitivity of 98%, and specificity of 78% [24]. A separate meta-analysis reported pooled sensitivity and specificity of 0.87 and 0.83, respectively [22].
ESR Measurement Protocol for DFO Suspicion
The diagram below illustrates the role of ESR in the diagnostic pathway for suspected diabetic foot osteomyelitis.
Objective: To measure the erythrocyte sedimentation rate as an inflammatory marker to aid in the diagnosis of diabetic foot osteomyelitis [25] [6].
Materials:
- Venous blood collection kit (needle, tourniquet, etc.)
- Vials containing Ethylenediaminetetraacetic acid (EDTA) anticoagulant
- Equipment for ESR analysis (e.g., automated analyzer using the modified Westergren method) [25]
Step-by-Step Procedure:
- Blood Collection: Draw a 6 mL peripheral blood sample under aseptic conditions and transfer it to a vial containing EDTA anticoagulant [25].
- Sample Analysis: Analyze the blood sample using a validated method. The modified Westergren method is commonly used and reported [25].
- Interpretation: Interpret the result against predefined cutoffs. A recent meta-analysis recommends a cutoff of 51.6 mm/h as optimal for screening, with a sensitivity of 80% and specificity of 67% [6]. The traditional cutoff of 70 mm/h offers higher specificity (83%) but lower sensitivity (61%) [6].
- Contextualization: Always interpret the ESR value in the context of the clinical presentation and other diagnostic tests. An elevated ESR should increase the index of suspicion for DFO and warrant further investigation.
Key Validation Data: A 2025 meta-analysis of 12 studies (1,674 subjects) determined the summary AUC for ESR in diagnosing DFO to be 0.71, with a sensitivity of 0.76 and specificity of 0.73 [6]. Another cross-sectional study reported an AUC of 0.70 for ESR, classifying its accuracy as "fair" [25].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Diagnostic Validation Studies
| Item | Function / Application in Research | Specification / Standardization |
|---|---|---|
| Sterile Surgical Probe | Performing the PTB test to detect bone exposure in ulcers. | Blunt metal instrument; sterilization between uses is critical [24]. |
| EDTA Blood Collection Tubes | Anticoagulation of venous blood samples for subsequent ESR analysis. | Standard 6 mL draw volume [25]. |
| ESR Analyzer & Kits | Quantifying the erythrocyte sedimentation rate. | Adherence to standardized methods (e.g., modified Westergren) [25]. |
| Bone Biopsy Instrumentation | Obtaining bone specimens for histopathological analysis (reference standard). | Requires surgical intervention; samples preserved in 10% buffered formalin [24]. |
| Semmes-Weinstein Monofilament | Assessing peripheral neuropathy, a key risk factor for DFU and DFO. | 5.07 / 10 gram monofilament for standardized testing [24]. |
| Microbiology Transport Medium | Transporting soft tissue and bone specimens for microbial culture. | Sterile vessel with transport medium (e.g., Copan Innovation) [24]. |
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: The PTB test shows high sensitivity in studies, but my clinical team finds it has a low positive predictive value. What is the explanation for this discrepancy?
A: This is a classic example of the impact of disease prevalence on predictive values. The PTB test's positive predictive value (PPV) is highly dependent on the underlying prevalence of osteomyelitis in the studied population [23]. In a population with a low prevalence of osteomyelitis (e.g., 12%), even a highly specific test will yield a lower PPV. In the referenced study, with a 12% prevalence, the PPV was 57%, meaning almost half of the positive tests were false positives. However, the negative predictive value (NPV) remained very high (98%), making it an excellent "rule-out" tool [23]. In high-prevalence settings (e.g., >70%), the PPV rises significantly [24] [22].
Q2: When validating ESR in our patient cohort, what is the single most evidence-based cutoff value we should use to define a positive test for osteomyelitis?
A: A 2025 systemic review and meta-analysis specifically addressed this using advanced modeling (DICS model) to calculate an optimal pooled cutoff. The study recommends 51.6 mm/h as the optimal cutoff, which balances sensitivity (80%) and specificity (67%) for screening purposes [6]. If your research priority is to maximize specificity (e.g., for patient enrollment in a clinical trial), the traditional cutoff of 70 mm/h (specificity 83%) may be more appropriate, albeit with a loss of sensitivity (61%) [6].
Q3: How does the diagnostic accuracy of ESR compare to C-Reactive Protein (CRP) for detecting DFO?
A: Both are acute-phase reactants with modest accuracy for DFO. Direct comparative studies have shown that ESR generally has slightly superior performance. One cross-sectional study found the AUC for ESR was 0.70 ("fair" accuracy) compared to 0.67 ("poor" accuracy) for CRP. The same study reported the best cut-off for CRP was 35 mg/L, with a sensitivity of 76% and specificity of 55% [25]. CRP rises and falls more rapidly than ESR, so it may be more useful for monitoring treatment response rather than initial diagnosis.
Q4: What is the recommended reference standard against which we should validate new molecular diagnostics for DFO?
A: The most definitive reference standard is bone histopathology. The consensus criteria for diagnosis include the presence of inflammatory cell infiltrate (e.g., lymphocytes, plasma cells, neutrophils), bone necrosis, and reactive bone neoformation [24]. Bone culture is also used, often in conjunction with histology. While MRI is a highly sensitive imaging modality, it is still often validated against histology as the ultimate benchmark [24] [6]. Your experimental protocols should clearly state the chosen reference standard.
Technical Troubleshooting Guides
Troubleshooting SCUBE1 Expression Analysis
Problem: Inconsistent SCUBE1 detection in DFU patient samples via qRT-PCR
| Problem Area | Possible Cause | Solution | Verification |
|---|---|---|---|
| Low RNA Quality | Degraded RNA from necrotic DFU tissue | Implement rigorous RNA integrity number (RIN) assessment; accept only samples with RIN >7.0 | Bioanalyzer electropherogram shows intact 18S and 28S ribosomal RNA peaks |
| Low Abundance Target | SCUBE1 significantly downregulated in cured DFU [26] [4] | Use highly sensitive detection chemistry (TaqMan vs. SYBR Green); increase RNA input to 100ng per reaction | Standard curve with dilution series shows efficient amplification (90-105%) |
| Sample Heterogeneity | Varying degrees of immune cell infiltration in biopsy sites | Standardize biopsy location; use single-cell RNA sequencing for cellular resolution | Single-cell validation shows SCUBE1 expression primarily in NK cells and macrophages [26] |
| Data Normalization | Unstable reference genes in pathological tissue | Validate reference genes (e.g., GAPDH, β-actin) using geNorm or NormFinder; use multiple reference genes | Coefficient of variation <0.2 across sample groups after normalization |
Problem: Poor SCUBE1 antibody performance in Western blotting
| Problem Area | Possible Cause | Solution | Verification |
|---|---|---|---|
| Protein Extraction | SCUBE1 is a secreted/ membrane-associated protein [27] | Use combination detergent (1% Triton X-100) with mild sonication; include protease inhibitors | Detection of positive control (recombinant SCUBE1) confirms extraction efficiency |
| Glycosylation Issues | Extensive N-glycosylation in spacer region alters mobility [27] | Treat samples with PNGase F; expect mobility shift from ~100kDa to ~80kDa | Sharp band appears after deglycosylation |
| Specificity | Non-specific binding in complex wound tissue | Include peptide competition control; use blocking buffer with 5% BSA + 5% normal serum | Signal abolished with competing peptide |
Troubleshooting RNF103-CHMP3 Functional Studies
Problem: High variability in extracellular interaction assays for RNF103-CHMP3
| Problem Area | Possible Cause | Solution | Verification |
|---|---|---|---|
| Cellular Model | Endogenous expression interferes with overexpression | Use CRISPR/Cas9 knockout cell line before transfection; confirm knockout via sequencing | Western blot shows complete absence of endogenous protein |
| Assay Timing | Dynamic changes during epithelial-mesenchymal transition | Perform time-course experiments (0, 6, 12, 24, 48h) post-wounding in scratch assay | Phase-contrast microscopy shows consistent migration patterns |
| Cell-Cell Communication | Disruption of extracellular matrix interactions [26] | Include ECM components (collagen I, fibronectin) in coating; measure soluble factors in conditioned media | Proteomic analysis of secretome identifies interaction partners |
Frequently Asked Questions (FAQs)
Q1: What is the clinical relevance of SCUBE1 and RNF103-CHMP3 as therapeutic targets in diabetic foot ulcers?
SCUBE1 and RNF103-CHMP3 represent promising therapeutic targets because they were identified as significantly downregulated in patients who were successfully cured of DFU, suggesting their expression patterns are closely linked to healing response [26] [4]. SCUBE1 plays a role in immune regulation, particularly in the body's response to inflammation and infection, which are critical factors in DFU pathogenesis [26]. RNF103-CHMP3 is involved in extracellular interactions, suggesting importance in cellular communication and tissue repair mechanisms [26]. Their discovery offers new theoretical foundations and molecular targets for DFU diagnosis and treatment optimization [26] [4].
Q2: What are the recommended experimental models for studying SCUBE1 function in DFU pathogenesis?
For in vitro studies, primary human keratinocytes or fibroblast cell lines under hyperglycemic conditions (25mM glucose) can model diabetic skin. Oxidative stress can be induced with H₂O₂ (0.3mM) to examine SCUBE1's protective role, as demonstrated in granulosa cells [28]. For immune function studies, co-culture systems with macrophages (e.g., THP-1 cells) allow investigation of SCUBE1's role in immune cell infiltration [26]. For in vivo approaches, diabetic mouse models (e.g., db/db mice) with excisional wounds represent the gold standard. Single-cell RNA sequencing of wound tissue can pinpoint specific cellular sources of SCUBE1 expression, which has been localized to NK cells and macrophages in DFU [26].
Q3: How does RNF103-CHMP3 influence extracellular interactions in the DFU microenvironment?
While the precise mechanisms are still under investigation, RNF103-CHMP3 has been associated with extracellular interactions that are crucial for proper cellular communication during wound healing [26]. As a protein potentially involved in endosomal sorting and membrane trafficking (inferred from the CHMP3 domain), it may regulate the secretion of extracellular matrix components or signaling molecules that facilitate cell-cell communication. In the dysfunctional DFU microenvironment, downregulation of RNF103-CHMP3 may disrupt these critical extracellular interactions, impairing the coordinated cellular responses needed for effective tissue repair [26].
Q4: What computational approaches are available for identifying additional targets like SCUBE1 and RNF103-CHMP3?
The original identification of SCUBE1 and RNF103-CHMP3 employed machine learning analysis of transcriptome data from the GEO dataset GSE230426 [26] [4]. This integrated approach combined differential expression analysis (using limma package in R with thresholds of │logFC│>1 and p<0.05) with machine learning algorithms including LASSO regression and SVM-RFE for feature selection [26]. Validation in independent datasets (GSE80178, GSE165816) confirmed reliability [26] [4]. Similar workflows can be applied, incorporating additional methods like weighted gene co-expression network analysis (WGCNA) [29] [30] and single-cell RNA sequencing analysis [11] to uncover novel targets in DFU.
Q5: What are the key considerations for validating SCUBE1 and RNF103-CHMP3 as diagnostic biomarkers?
Analytical Validation: Establish reliable detection assays (qRT-PCR, ELISA) with determined precision, accuracy, and sensitivity. Define reference ranges in appropriate control populations [26]. Clinical Validation: Correlate expression levels with DFU severity (e.g., Wagner grade), healing trajectory, and clinical outcomes in prospective cohorts [26] [4]. Specificity Assessment: Evaluate expression patterns in other wound etiologies to ensure specificity to DFU pathophysiology. Sample Standardization: Standardize sample collection procedures (e.g., biopsy location, RNA stabilization) due to the heterogeneity of DFU tissue [26].
Research Reagent Solutions
Key Reagents for SCUBE1 and RNF103-CHMP3 Research
| Reagent Category | Specific Product/Assay | Function/Application | Key Considerations |
|---|---|---|---|
| Detection Antibodies | Anti-SCUBE1 (Bioss, bs-9903R) [28] | IHC, WB for protein localization and expression | Validate with peptide competition; note glycosylation state in WB |
| Anti-RNF103-CHMP3 | IP, IF for protein interaction studies | Confirm specificity in knockout cell lines | |
| Recombinant Proteins | rhSCUBE1 (Abnova) [28] | Functional studies (e.g., 5ng/mL pretreatment) | Test bioactivity in migration/proliferation assays |
| Cell Lines | KGN granulosa cell line [28] | Model for oxidative stress studies | Adapt for DFU research with hyperglycemic conditions |
| Primary human keratinocytes | Relevant DFU cell type for mechanistic studies | Use early passages (P3-P5) for consistency | |
| Animal Models | db/db mice | In vivo wound healing studies | Monitor blood glucose >350mg/dL before wounding |
| Critical Assays | Single-cell RNA-seq [26] [11] | Cellular resolution of target expression | Process fresh tissue; target 10,000 cells/sample |
| AUCell analysis [11] | Metabolic state assessment (hypoxia, glycolysis) | Use hallmark gene sets from GSEA |
Experimental Protocols
Transcriptomic Analysis Pipeline for Target Identification
This protocol follows the methodology that successfully identified SCUBE1 and RNF103-CHMP3 [26] [4].
Step 1: Data Acquisition and Preprocessing
- Download DFU transcriptome data from GEO (e.g., GSE230426, GSE80178, GSE165816)
- Perform quality control: RIN >7.0 for RNA-seq, presence of internal controls for arrays
- Normalize data: RMA for microarray data, TPM/FPKM for RNA-seq data
- Batch effect correction: Use ComBat or sva package in R [30]
Step 2: Differential Expression Analysis
- Utilize limma package in R with thresholds: │logFC│>1 and adjusted p-value <0.05 [26]
- Generate volcano plots using ggplot2 package
- Identify 403-500 differentially expressed genes typically observed in DFU studies [30]
Step 3: Enrichment Analysis
- Perform GO, KEGG, and Disease Ontology enrichment using clusterProfiler [26]
- Focus on immune regulation, extracellular matrix, and cell communication pathways
- Identify significantly enriched pathways (p-value <0.05, FDR <0.1)
Step 4: Machine Learning Feature Selection
- Apply LASSO regression (glmnet package) for dimensionality reduction [26] [30]
- Implement SVM-RFE algorithm for feature ranking [26]
- Use 10-fold cross-validation to determine optimal parameters [30]
- Identify top candidate genes (e.g., SCUBE1, RNF103-CHMP3) [26]
Step 5: Validation
- Validate key genes in independent datasets (e.g., GSE80178) [26]
- Examine expression at single-cell level in datasets like GSE165816 [26] [11]
- Correlate gene expression with clinical outcomes (healing status)
SCUBE1 Functional Analysis in Oxidative Stress Model
This protocol adapts SCUBE1 oxidative stress protection assessment for DFU-relevant cell types [28].
Step 1: Cell Culture and Treatment
- Culture relevant cells (keratinocytes, fibroblasts) in high glucose (25mM) DMEM/F12 with 10% FBS
- Plate cells in 6-well plates (2×10^5 cells/well) for apoptosis analysis or 96-well plates (5×10^3 cells/well) for viability
- Pretreat experimental group with 5ng/mL rhSCUBE1 for 24h [28]
- Induce oxidative stress with 0.3mM H₂O₂ for 24h [28]
Step 2: Viability and Apoptosis Assessment
- MTT assay: Add 0.5mg/mL MTT, incubate 4h, dissolve in DMSO, measure 570nm absorbance
- Annexin V/PI staining: Analyze by flow cytometry within 1h of staining
- Caspase-3 activity: Use fluorometric assay with DEVD-AFC substrate
Step 3: ROS and Mitochondrial Function
- Intracellular ROS: Load cells with 10μM DCFH-DA for 30min, measure fluorescence (Ex/Em 485/535nm)
- Mitochondrial membrane potential: Stain with 5μg/mL JC-1 for 15min, calculate red/green fluorescence ratio
Step 4: Western Blot Analysis
- Extract proteins with RIPA buffer + protease inhibitors
- Separate 30μg protein on 10% SDS-PAGE, transfer to PVDF
- Block with 5% non-fat milk, incubate with primary antibodies (1:1000) overnight at 4°C
- Target: Bcl-2, Bax, cleaved caspase-3, p53 [28]
- Incubate with HRP-conjugated secondary antibodies (1:5000), develop with ECL
Step 5: Data Analysis
- Normalize viability to untreated control (set as 100%)
- Express apoptosis as % Annexin V-positive cells
- Quantify Western blots by densitometry, normalize to β-actin
- Statistical analysis: One-way ANOVA with Tukey's post-hoc test, p<0.05 significant
Single-Cell RNA Sequencing Analysis for Cellular Localization
This protocol validates cell-type specific expression of targets like SCUBE1 and RNF103-CHMP3 [26] [11].
Step 1: Sample Preparation and Sequencing
- Process fresh DFU biopsies (3-5mm) within 30min of collection
- Digest tissue with collagenase IV (1mg/mL) for 45min at 37°C with agitation
- Filter through 40μm strainer, resuspend in PBS + 0.04% BSA
- Target cell viability >85% before loading on 10X Chromium
- Sequence to depth of 50,000 reads/cell minimum
Step 2: Data Processing and Quality Control
- Process raw data using Cell Ranger (10X Genomics)
- Filter cells with <200 or >6,000 genes, >10% mitochondrial content [11]
- Normalize using SCTransform (Seurat) or comparable methods
- Integrate multiple samples using harmony or CCA anchors
Step 3: Cell Clustering and Annotation
- Perform PCA and UMAP dimensionality reduction
- Cluster cells using Louvain algorithm (resolution 0.5-1.2) [11]
- Annotate cell types using canonical markers:
- Keratinocytes: KRT5, KRT14, KRT10
- Fibroblasts: DCN, COL1A1, PDPN
- Endothelial: PECAM1, VWF
- Immune: PTPRC (CD45)
- Macrophages: CD68, CD163, MRC1
- T cells: CD3D, CD3E
- NK cells: NKG7, GNLY [26]
Step 4: Target Gene Expression Analysis
- Extract expression values for SCUBE1 and RNF103-CHMP3
- Visualize using feature plots, violin plots, and dot plots
- Compare expression between cell types and conditions (non-healing vs. healing)
- Validate findings with immunohistochemistry on parallel tissue sections
Step 5: Cellular Communication Analysis
- Use CellChat or NicheNet to infer intercellular communication
- Identify altered signaling pathways in DFU vs. normal skin
- Focus on pathways involving SCUBE1 and RNF103-CHMP3
Next-Generation Diagnostic Tools: From Biomarker Panels to Explainable AI Models
FAQs and Troubleshooting Guides
Data Acquisition and Preprocessing
Q1: What are the critical inclusion and exclusion criteria for patient data when building a dataset to differentiate Diabetic Foot Infection (DFI) from Osteomyelitis (OM)?
A: Ensuring a clean, well-defined cohort is paramount for model generalizability. Adhere to the following criteria based on established study designs [31]:
- Inclusion Criteria:
- Patients aged 18 years or older.
- A confirmed diagnosis of diabetes mellitus.
- A definitive final diagnosis of either DFI or OM, based on a composite reference standard that can include clinical findings, imaging (e.g., MRI), laboratory results, and bone biopsy or surgical debridement findings.
- Exclusion Criteria:
- Primary foot pathology unrelated to DFI/OM (e.g., Charcot neuroarthropathy without infection, major trauma).
- Concurrent systemic conditions that confound biomarker interpretation (e.g., active autoimmune disease, sepsis from another source, active malignancy).
- Incompleteness of the core routine blood biomarker dataset (e.g., >30% missing values for key variables).
Q2: My dataset has missing values for some biomarkers. How should I handle this?
A: The handling of missing data is a critical step in the preprocessing pipeline.
- Best Practice: First, investigate the pattern of missingness. If data is Missing Completely At Random (MCAR), you can use imputation techniques.
- Recommended Technique: For routine laboratory biomarkers, multiple imputation or k-nearest neighbors (KNN) imputation are robust methods. However, if the missing data is extensive (e.g., exceeding 30% for a specific biomarker in your dataset), consider excluding that variable or patient record, as was done in the referenced study [31].
- Troubleshooting: If model performance is poor, check the impact of your imputation method. Sensitivity analysis (comparing complete-case analysis with imputed results) is highly recommended.
Model Development and Training
Q3: Which machine learning algorithms are most effective for building a diagnostic model with these biomarkers?
A: Multiple classifiers should be evaluated and compared. A recent large-scale study found the LightGBM (Light Gradient Boosting Machine) model to be the top-performing algorithm for this specific task, outperforming others when using a compact set of routine biomarkers [31].
- Recommended Workflow:
- Train Multiple Models: Experiment with a suite of models, including Random Forests, Support Vector Machines (SVM), and XGBoost, in addition to LightGBM.
- Evaluate Performance: Use the Area Under the Receiver Operating Characteristic Curve (AUC) as a primary metric, supplemented by the Brier score for calibration.
- Select Final Model: Choose the model that demonstrates the highest AUC and is well-calibrated on your internal validation set.
Q4: How can I ensure my model is trustworthy and not a "black box" for clinicians?
A: Model interpretability is non-negotiable for clinical adoption. Integrate Explainable AI (XAI) techniques directly into your workflow.
- Solution: Employ SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations). These tools quantify the contribution of each biomarker (e.g., HbA1c, ESR) to individual predictions [31]. This allows a clinician to see why a case was classified as DFI or OM, fostering trust and providing actionable insights.
Model Validation and Deployment
Q5: What is the gold standard for validating the performance of my diagnostic model?
A: Beyond standard internal validation (e.g., train-test split or cross-validation), external validation is critical.
- Protocol: Reserve a portion of your data from a completely different clinical center or geographic location as an independent external validation cohort. A model that achieves an AUC of 0.942 on an external cohort, as demonstrated in recent research, provides strong evidence of its generalizability and robustness [31].
- Troubleshooting: A significant performance drop in external validation indicates overfitting to your development data or underlying population differences. Revisit feature selection and model regularization.
Q6: How can I make my model accessible for other researchers and clinicians?
A: Develop a user-friendly, publicly accessible tool.
- Proven Method: Create a web-based calculator. This allows users to input the six key biomarkers (Age, HbA1c, Creatinine, Albumin, ESR, Sodium) and receive a risk prediction for OM vs. DFI. This approach translates your research into a low-cost, clinically applicable tool, especially useful in resource-limited settings [31].
Experimental Protocols
Protocol: Developing and Validating an Explainable ML Model for DFI/OM Differentiation
This protocol outlines the methodology for building a diagnostic model based on a successful two-center study [31].
1. Objective To develop and validate an explainable machine learning model using routine blood biomarkers (Age, HbA1c, Creatinine, Albumin, ESR, Sodium) to accurately differentiate between Diabetic Foot Infection (DFI) and Osteomyelitis (OM).
2. Materials and Dataset Preparation
- Data Collection: Collect retrospective data from patient electronic health records. Ensure ethical approval and data anonymization.
- Cohort Definition: Define DFI and OM cases based on a composite reference standard (e.g., clinical exam, imaging, bone biopsy). Apply strict inclusion/exclusion criteria [31].
- Feature Selection: Extract the six key biomarkers. Normalize numerical values (e.g., Z-score standardization).
3. Machine Learning Workflow
- Data Partitioning: Split the dataset from Center 1 into a training set (75%) and an internal validation set (25%). Use data from Center 2 as a hold-out external validation set.
- Model Training: Train multiple ML classifiers (LightGBM, Random Forest, SVM, etc.) on the training set using 5-fold cross-validation.
- Hyperparameter Tuning: Optimize model parameters using techniques like Bayesian optimization or grid search on the validation set.
- Model Evaluation: Evaluate the final selected model on the internal and external validation sets. Key metrics include AUC, accuracy, sensitivity, specificity, and Brier score.
4. Explainability and Clinical Translation
- Explainable AI (XAI): Apply SHAP analysis to the final model to generate global feature importance plots and local explanations for individual predictions.
- Deployment: Develop a web calculator using a framework like Flask or Shiny to host the model for public use.
Table 1: Performance Metrics of a LightGBM Model for Differentiating DFI from OM on an External Validation Cohort (n=341) [31]
| Metric | Value (95% Confidence Interval) |
|---|---|
| Area Under the Curve (AUC) | 0.942 (0.936 - 0.950) |
| Sensitivity | Not specified in results |
| Specificity | Not specified in results |
| Brier Score (Lower is better) | Not specified in results |
Table 2: Key Biomarkers and Their Hypothesized Pathophysiological Roles in DFI/OM [31]
| Biomarker | Biological Function & Rationale for Inclusion |
|---|---|
| HbA1c | Reflects long-term glycemic control. Hyperglycemia impairs immune function and wound healing, increasing susceptibility to severe infection. |
| ESR | A non-specific marker of inflammation. Typically elevated in both DFI and OM, but levels may vary with severity and bone involvement. |
| Creatinine | Indicator of renal function. Renal impairment can alter drug pharmacokinetics (antibiotics) and is a comorbidity in diabetic patients. |
| Albumin | A marker of nutritional status and systemic inflammation. Low levels are associated with poorer healing outcomes and increased morbidity. |
Research Reagent Solutions
Table 3: Essential Materials for ML-Based Diagnostic Model Development
| Item | Function/Description |
|---|---|
| Clinical Data Repository | Anonymized electronic health records from patients with confirmed DFI or OM. |
| Computing Environment | Python or R programming environment with libraries (e.g., scikit-learn, LightGBM, SHAP, pandas). |
| Statistical Software | R or Python for data preprocessing, statistical analysis, and generation of performance metrics. |
| Web Development Framework | Flask (Python) or Shiny (R) for building an interactive web interface to deploy the final model. |
Workflow and Pathway Diagrams
Diagram 1: End-to-end workflow for developing and deploying an explainable ML model.
Diagram 2: Logical relationship between model prediction and explainable AI for clinical support.
Troubleshooting Guide: SHAP and LIME for Diabetic Foot Diagnostics
Frequently Asked Questions
Q1: Why do my SHAP values show unexpected feature importance rankings that don't match clinical understanding?
This commonly occurs due to highly correlated molecular features in diabetic foot ulcer (DFU) datasets. When features are strongly correlated, SHAP values might distribute importance in ways that appear counterintuitive [32] [33]. The VeriStrat test case study found correlations between features ranging from 0.310 to 0.996, which significantly affected importance distributions [33].
Solution:
- Calculate exact Shapley values instead of approximations when possible, especially with smaller datasets [32]
- Use Shapley-based interaction indices (SIIs, STIIs) to identify feature interactions [33]
- Apply domain knowledge to evaluate if correlated features represent similar biological pathways
Q2: My LIME explanations are unstable - they change significantly with each run for the same patient. How can I increase reliability?
LIME generates explanations by sampling perturbed instances around your prediction, and this randomness can cause instability, particularly with complex molecular data [34] [35].
Solution:
- Increase the
sample_sizeparameter in LIME to generate more perturbed samples [35] - Set a random seed for reproducible explanations
- For tabular data, ensure
discretize_continuous=Trueto create more stable categorical features [35] - Consider using SHAP for more mathematically grounded explanations [36]
Q3: Which XAI method is better for explaining differential diagnosis of diabetic foot infections versus osteomyelitis?
In a recent two-center study comparing DFI and OM differentiation, SHAP provided more quantitative insights into biomarker contributions, while LIME offered intuitive local explanations [37]. The study achieved an AUC of 0.942 using a LightGBM model with six key biomarkers [37].
Solution:
- Use SHAP for global model interpretability and understanding overall feature importance
- Use LIME for case-specific explanations to present to clinical colleagues
- Implement both methods as complementary approaches
Q4: How can I extract global model understanding from local explanation methods?
Both SHAP and LIME can be aggregated to provide global insights [34] [35].
Solution for SHAP:
- Calculate mean absolute SHAP values across all predictions for global feature importance
- Plot SHAP summary charts showing feature impact versus value
Solution for LIME:
- Implement "Submodular Pick" methodology to select diverse, representative explanations [35]
- Aggregate local explanations across multiple patient subgroups
- Create frequency analysis of top features across numerous local explanations
Performance Comparison Table: XAI Methods in Clinical Diagnostics
Table 1: Quantitative performance of XAI-enhanced models in diabetic complications research
| Study Focus | Best Performing Model | Accuracy Metrics | XAI Method Used | Key Features Identified |
|---|---|---|---|---|
| Diabetic Foot Ulcer Identification [38] | Siamese Neural Network (SNN) | 98.76% accuracy, 99.3% precision, 97.7% recall, 98.5% F1-score | Grad-CAM, SHAP, LIME | Heat map localization for visual interpretation |
| Differential Diagnosis: DFI vs. Osteomyelitis [37] | LightGBM | AUC: 0.942 (external validation) | SHAP, LIME | Age, HbA1c, Creatinine, Albumin, ESR, Sodium |
| Molecular Diagnostic Test (VeriStrat) [32] [33] | 7-Nearest Neighbor | Clinical validation in 40,000+ samples | Exact Shapley Values | 8 proteomic features with varying importance per sample |
Table 2: Technical comparison of SHAP vs. LIME for clinical applications
| Characteristic | SHAP | LIME |
|---|---|---|
| Explanation Scope | Global & local interpretability | Focus on local interpretability |
| Mathematical Foundation | Game theory (Shapley values) | Local surrogate models |
| Computational Demand | Higher for exact calculations | Generally faster |
| Data Type Compatibility | Tabular, text, images | Tabular, text, images |
| Clinical Implementation | Quantitative contribution scores | Intuitive "push-pull" explanations |
| Handling of Correlated Features | Can be challenging with approximations | Affected by perturbation strategy |
Experimental Protocols for Diabetic Foot Ulcer Research
Protocol 1: Implementing SHAP for Molecular Diagnostic Patterns
Materials Required:
- Pre-trained ML model for DFU classification
- Patient dataset with molecular features
- SHAP Python library (
pip install shap)
Procedure:
- Load and prepare your trained model and preprocessing pipeline
- Initialize appropriate SHAP explainer:
- Use
TreeExplainerfor tree-based models - Use
KernelExplainerfor model-agnostic applications - Use
DeepExplainerfor neural networks
- Use
- Calculate SHAP values on representative data sample:
- Generate global feature importance plot:
- Create individual force plots for specific patient explanations
- Calculate mean absolute SHAP values for overall feature ranking
Troubleshooting Tip: For small datasets (<1000 samples), use exact Shapley value calculation instead of approximations to avoid qualitative differences in explanations [32].
Protocol 2: LIME for Case-Specific DFU Explanations
Materials Required:
- Trained classification model with
predict_probamethod - LIME Python library (
pip install lime) - Individual patient case data
Procedure:
- Initialize LIME Tabular Explainer with training data statistics:
- Generate explanation for specific case:
- Visualize explanation:
- Save explanation as HTML for clinical reporting:
Troubleshooting Tip: If explanations seem sparse or incomplete, adjust the num_features parameter and try different feature_selection methods ('auto', 'lasso_path', or 'none') [35].
Research Reagent Solutions for Diabetic Foot Ulcer Diagnostics
Table 3: Essential materials and computational tools for XAI experiments
| Resource Type | Specific Tool/Resource | Application in DFU Research |
|---|---|---|
| Programming Libraries | SHAP (Python library) | Quantitative feature contribution analysis for molecular markers |
| Programming Libraries | LIME (Python library) | Case-by-case explanation generation for clinical review |
| Model Architectures | Siamese Neural Networks [38] | DFU image classification with 98.76% accuracy |
| Model Architectures | LightGBM [37] | Differential diagnosis of foot infections with high AUC |
| Clinical Validation Tools | Grad-CAM heat maps [38] | Visual localization of ulcer features in image data |
| Biomarker Panels | Routine blood tests [37] | Six-key biomarker panel (HbA1c, Creatinine, Albumin, ESR, etc.) |
| Molecular Assays | Mass spectrometry proteomics [33] | VeriStrat test with 8 protein features for classification |
Workflow Visualization
XAI Clinical Diagnostics Workflow
Correlation Challenges in Molecular Data
FAQs: Technical Guidance for Researchers
FAQ 1: What are the top-performing deep learning architectures for diabetic foot ulcer (DFU) segmentation, and how do they compare quantitatively?
The performance of deep learning models for DFU segmentation is typically evaluated using metrics like Intersection over Union (IoU) and Dice coefficient. Below is a comparative analysis of leading architectures.
Table 1: Performance Comparison of DFU Segmentation Models
| Model Architecture | Reported Mean IoU | Key Strengths | Notable Applications/Studies |
|---|---|---|---|
| Mask2Former | 65% [18] | Best overall performance; excels in multi-label recognition and global feature modeling [18]. | Segmentation and classification of periwound erythema, ulcer boundaries, and internal tissues (granulation, necrotic tissue, etc.) [18]. |
| Deeplabv3plus | 62% [18] | Well-established CNN-based model; widespread application in semantic segmentation [18]. | Served as a baseline model in performance comparisons [18]. |
| UFOS-Net | Dice: 0.7745 [39] | Incorporates an Enhanced Multi-scale Segmentation (EMS) block; optimized for small-scale mask identification [39]. | Ranked highly on the DFUC2022 leaderboard; validated on the SRRSH-DF dataset [39]. |
| Swin-Transformer | 52% [18] | Leverages Transformer architecture to handle long-range dependencies [18]. | Suitable for recognizing complex features in DFU images [18]. |
FAQ 2: How can I address the challenge of limited and imbalanced DFU image datasets in my model training?
Data augmentation is a cornerstone technique for mitigating dataset limitations. Beyond standard methods (rotation, flipping), researchers have developed tailored strategies for DFU images.
- Multi-Operator Data Augmentation (MODA): This method simultaneously applies multiple augmentation operators specifically chosen for DFU characteristics, significantly expanding the dataset and improving model generalization [39].
- Standard Augmentation Techniques: The following five techniques are commonly employed to enhance model robustness [18]:
- Brightness Adjustment
- Contrast Adjustment
- Horizontal Flip
- Vertical Flip
- Transposition
FAQ 3: My model confuses ulcer areas with healthy skin of similar color. How can I improve segmentation accuracy for complex lesions?
This is a common challenge, particularly when model parameters are reduced for efficiency [39]. Consider these approaches:
- Architecture Enhancement: Integrate modules designed for detailed feature extraction. The EMS Block in UFOS-Net, which uses depthwise separable convolutions, helps capture more comprehensive features with a reduced parameter count, improving the handling of texture details [39].
- Advanced Feature Fusion: Leverage models that incorporate small-scale feature fusion, which can enhance the identification of subtle boundaries between ulcers and normal skin [39].
- Hybrid Feature Extraction: For classification tasks, combining handcrafted features (e.g., ORB, LBP) with deep features from pretrained CNNs can create a more robust and noise-resistant model, as demonstrated in frameworks for plantar thermograms [40].
FAQ 4: How is the Wagner classification system integrated into deep learning models for automated DFU grading?
The Wagner classification system provides a standardized framework for assessing ulcer severity. In deep learning, it is used as the ground truth for training and evaluating classification models.
- Adaptation for Model Training: Models are trained to categorize DFU images into Wagner grades. For instance, one study grouped Wagner grades 1-2 into a single category due to similar treatment strategies, and trained the Mask2former model to classify wounds into W1-2, W3, and W4 [18].
- Model Performance: In such a task, the Mask2former model achieved an accuracy of 0.9185 and an Area Under the Curve (AUC) of 0.9429 [18].
- System Overview:
- Grade 0: No open lesions [41] [42].
- Grade 1: Superficial ulcer limited to the skin [41] [42].
- Grade 2: Deeper ulcer extending to ligaments and muscle [41] [42].
- Grade 3: Deep ulcer with abscess, osteomyelitis (bone infection), or joint sepsis [41] [42].
- Grade 4: Partial gangrene in the forefoot [41] [42].
- Grade 5: Extensive gangrene involving the entire foot [41] [42].
Troubleshooting Guides
Issue 1: Poor Segmentation Performance on Small or Complex Ulcer Regions
- Symptoms: Low IoU or Dice scores for specific tissue types like tendons or periwound erythema; failure to detect subtle lesion boundaries.
- Investigation Checklist:
- Examine the distribution of your annotated masks. Are small-scale ulcers adequately represented?
- Verify the model's decoder. Does it incorporate multi-scale feature fusion to preserve details from early layers?
- Inspect the data augmentation pipeline. Are you using strategies like MODA to increase the diversity of complex lesion appearances? [39]
- Resolution Steps:
- Model Selection: Prioritize architectures known for detail capture, such as UFOS-Net with its EMS block [39] or Mask2Former for its strong multi-class performance [18].
- Data Curation: Consider using more comprehensive datasets like SRRSH-DF [39] or the DFUC 2022 dataset [43], which contain a wide spectrum of pathological features.
- Post-Processing: Apply contour refinement algorithms (e.g., active contours) to the model's raw output to better align with clinical delineations [43].
Issue 2: Model Fails to Generalize to Images from Different Sources
- Symptoms: High accuracy on the test set from the same source as training data, but significant performance drop on external datasets or new hospital data.
- Investigation Checklist:
- Check for domain shift. Are the new images from different devices, lighting conditions, or patient demographics?
- Review your preprocessing. Have you standardized image scaling (e.g., using bilinear interpolation to a fixed size like 1024x1024)? [18]
- Assess the training data. Does your dataset encompass the variability found in real-world clinical settings? [39]
- Resolution Steps:
- Data Augmentation: Aggressively employ photometric augmentations (brightness, contrast adjustments) to simulate domain variation [18].
- Transfer Learning: Fine-tune models that were pre-trained on large, diverse natural image datasets (e.g., ImageNet) [18].
- Hybrid Models: Explore frameworks that fuse traditional feature descriptors (like ORB) with deep learning features, as they can be more robust to image distortions [40].
Issue 3: High Computational Cost and Model Size Hindering Deployment
- Symptoms: Long training and inference times; model too large for target hardware (e.g., mobile devices or edge computers).
- Investigation Checklist:
- Profile the model. How many parameters does it have? Is the backbone network overly complex for the task?
- Evaluate the architecture. Are you using standard convolutions where depthwise separable convolutions could be applied? [39]
- Resolution Steps:
- Architecture Optimization: Adopt models designed for efficiency. The UFOS-Net's use of depthwise separable convolutions in its EMS block significantly reduces parameters while maintaining performance [39].
- Lightweight Classifiers: For classification tasks, the core feature extractor can be paired with a lightweight classifier (e.g., a DNN with two hidden layers of 32 neurons) for real-time operation [40].
Experimental Protocols & Workflows
Protocol 1: Building a Deep Learning Pipeline for DFU Segmentation and Wagner Classification
This protocol details the end-to-end process for training a model to segment DFU tissues and classify wound severity.
Table 2: Key Research Reagent Solutions for DFU Image Analysis
| Reagent / Resource | Type | Function in the Experiment | Example / Source |
|---|---|---|---|
| DFU Image Datasets | Data | Provides ground-truth images and annotations for model training and benchmarking. | DFUC 2022 [43], SRRSH-DF [39], FUSeg2021 [39] |
| Annotation Software | Tool | Used by clinical experts to manually delineate ulcer boundaries and tissue types. | Labelme [18], VGG Image Annotator (VIA) [43] |
| Deep Learning Models | Algorithm | Core architectures for segmentation and classification tasks. | Mask2Former [18], UFOS-Net [39], Deeplabv3plus [18] |
| Pre-trained Weights | Model Parameters | Provides initialization for model training, improving convergence and performance. | ImageNet [18] |
| Evaluation Metrics | Metric | Quantifies model performance for comparison and validation. | IoU, Dice Coefficient [18], Accuracy, AUC [18] |
Workflow Overview: The following diagram illustrates the sequential steps for a standard DFU image analysis pipeline.
Step-by-Step Methodology:
Data Collection and Curation:
Data Preprocessing and Annotation:
- Resizing: Scale images to a uniform size (e.g., 1024x1024) using bilinear interpolation to preserve critical details [18].
- Annotation: Have clinical experts use software like Labelme to meticulously annotate:
- Ulcer boundary.
- Tissue components: Granulation, necrotic tissue, tendon, bone, gangrene.
- Periwound erythema (indicating infection) [18].
- Data Augmentation: Apply techniques like brightness/contrast adjustment and flipping to increase dataset size and robustness [18] [39].
Model Selection and Training:
- Selection: Choose an appropriate model (e.g., Mask2Former for overall performance, UFOS-Net for complex lesions) [18] [39].
- Initialization: Use pre-trained weights (e.g., from ImageNet) as a starting point for training [18].
- Fine-tuning: Train the model on your annotated DFU dataset, monitoring loss and accuracy metrics until convergence [18].
Evaluation and Output:
- Quantitative Evaluation: Use the test set to calculate IoU, Dice, and for classification tasks, accuracy and AUC [18].
- Output: The model generates:
- Segmentation Masks: Pixel-wise identification of ulcers and internal tissues.
- Wagner Classification: A severity grade (e.g., W1-2, W3, W4) based on the detected features [18].
Protocol 2: Molecular Diagnostic Integration via Gene Expression Analysis
This protocol connects image-based findings with molecular diagnostics, aligning with the thesis context of optimizing molecular diagnostic patterns.
Workflow Overview: The diagram below shows how computational biology methods can identify diagnostic gene signatures linked to DFUs.
Step-by-Step Methodology:
- Data Acquisition: Obtain DFU-related gene expression datasets from public repositories like the Gene Expression Omnibus (GEO) [44].
- Bioinformatic Analysis:
- Identify Differentially Expressed Genes (DEGs) between DFU and control samples.
- Use Weighted Gene Co-expression Network Analysis (WGCNA) to find gene modules correlated with DFU traits.
- Intersect DEGs with key modules and analyze Protein-Protein Interaction (PPI) networks to screen for hub genes [44].
- Signature Identification: Apply machine learning algorithms (e.g., LASSO regression) to the candidate genes to finalize a concise diagnostic signature (e.g., genes DCT, PMEL, KIT) [44].
- Validation and Interpretation:
- Perform Gene Set Enrichment Analysis (GSEA) to uncover signaling pathways (e.g., MAPK, PI3K-Akt) influenced by the key genes [44].
- Correlate gene signatures with clinical features and image-based Wagner grades to build a multi-modal diagnostic profile.
FAQs: Data Acquisition and Preprocessing from GEO
Q1: What are the first critical steps after downloading a transcriptomic dataset for Diabetic Foot Infections (DFI) from the GEO database? The initial steps involve rigorous data preprocessing to ensure comparability and quality. Your first actions should be:
- Batch Effect Removal & Normalization: Use techniques like ComBat or surrogate variable analysis to correct for technical variations introduced by different experimental batches or platforms [45] [46]. This is crucial when integrating multiple DFI studies.
- Differential Gene Expression (DGE) Analysis: Apply established tools like DESeq2, edgeR, or limma to identify Differentially Expressed Genes (DEGs) between DFI samples and healthy controls [45] [47]. Standard cutoffs are a p-value < 0.05 and an absolute log2 Fold Change (logFC) > 0.5 [47].
Q2: How can I handle missing data and the integration of datasets from different sequencing platforms in a meta-analysis?
- Missing Data: Employ imputation methods such as k-nearest neighbor (KNN) imputation to estimate missing gene expression values based on the available data patterns [46].
- Data Integration (Meta-analysis): To combine datasets from different sources (e.g., microarray and RNA-seq):
- Standardize Gene Identifiers: Map all gene identifiers to a common system, such as official gene symbols or Entrez IDs [46].
- Normalize Data: Use appropriate normalization methods for each data type, such as TPM or RPKM for RNA-seq, and robust multi-array average (RMA) for microarrays [46].
- Assess and Correct Batch Effects: Apply advanced batch-effect correction tools like ComBat to harmonize the integrated dataset before downstream analysis [46].
FAQs: Machine Learning Analysis and Model Building
Q3: Which machine learning algorithms are most effective for narrowing down a large list of DEGs to a few high-value therapeutic targets for DFI? Intersecting results from multiple machine learning algorithms improves robustness. The following methods are highly effective for feature selection:
- LASSO (Least Absolute Shrinkage and Selection Operator): Performs both variable selection and regularization to enhance prediction accuracy [45].
- Support Vector Machine-Recursive Feature Elimination (SVM-RFE): Iteratively constructs an SVM model and removes the feature with the smallest ranking criterion [45].
- Random Forest (RF): An ensemble method that provides importance scores for each gene, allowing you to select the most informative features [45]. A best practice is to apply all three and prioritize genes consistently identified by multiple algorithms [45].
Q4: How can I validate the diagnostic performance of a predictive model built from these key genes?
- Develop a Nomogram: Construct a nomogram model based on the identified key genes to visualize the predictive model [45].
- Evaluate with AUC: Assess the model's diagnostic performance by calculating the Area Under the Curve (AUC) of the Receiver Operating Characteristic (ROC) curve. An AUC of 0.97 indicates excellent performance, as demonstrated in atrial fibrillation research, a benchmark to strive for [45].
Q5: What advanced analyses can provide deeper biological context to my machine-learning findings for DFI?
- Gene Set Enrichment Analysis (GSEA): Move beyond individual genes to identify biological pathways and processes that are collectively enriched in your DFI samples. Use multiple algorithms (e.g., camera, fgsea, gsva) and intersect their results for higher confidence [47].
- Immune Infiltration Analysis: Use deconvolution algorithms to characterize the composition of immune cells in the DFI tissue microenvironment, as the immune response plays a critical role in DFI pathology [45] [48].
- Single-Cell RNA Sequencing (scRNA-seq) Analysis: If data is available, perform or integrate scRNA-seq to investigate the cell-type-specific expression patterns of your candidate genes, which can pinpoint the exact cellular actors in DFI [45].
Troubleshooting Guides
Problem: Low Model Accuracy or Poor Generalization
- Cause 1: Inadequate Preprocessing. Insufficient batch effect correction or normalization can introduce noise that obscures true biological signals.
- Solution: Revisit data preprocessing steps. Ensure batch effects are rigorously corrected and normalization is appropriate for your data type [46].
- Cause 2: Overfitting. The model learns the noise in the training data instead of the underlying pattern, failing to perform well on new data.
- Solution: Implement cross-validation during model training. Use techniques like LASSO regularization, which inherently helps prevent overfitting [45].
- Cause 3: High Heterogeneity in DFI Samples. The "DFI" label may encompass patients with different underlying etiologies (e.g., neuropathic vs. ischemic).
- Solution: Assess study heterogeneity using statistical measures like Cochran's Q test or the I² statistic. If high, consider subgroup analysis or a random-effects model for meta-analysis [46].
Problem: Inconsistent or Conflicting Gene Signatures Across Studies
- Cause: Biological and Technical Variability. Differences in patient cohorts, sample collection sites, and experimental protocols can lead to divergent results.
- Solution: Perform a meta-analysis to identify robust gene expression patterns that persist across multiple independent studies. This improves statistical power and mitigates the impact of study-specific noise [46].
Problem: Difficulty in Identifying Spatially Variable Genes in DFI Tissue Sections
- Cause: Standard DGE analysis does not incorporate spatial information, which can be critical for understanding localized infection and immune responses in diabetic foot wounds.
- Solution: Utilize specialized software packages designed for spatial transcriptomics data.
Experimental Protocols for Validation
Protocol 1: Bioinformatics Meta-Analysis of Public GEO Datasets
- Define Objective: Clearly state the research question (e.g., "Identify conserved transcriptional signatures in DFI").
- Search & Select Studies: Query GEO using keywords ("diabetic foot", "transcriptomics", "Homo sapiens"). Establish inclusion/exclusion criteria based on sample type, platform, etc. [50] [46].
- Data Curation & Preprocessing:
- Download series matrix files.
- Standardize gene identifiers.
- Normalize data and correct for batch effects using ComBat.
- Impute missing data with KNN imputation [46].
- DGE and Meta-Analysis:
- Perform DGE on each study with DESeq2/limma (p<0.05, logFC>0.5).
- Use a random-effects model to combine effect sizes if significant heterogeneity is present (I² statistic > 50%) [46].
- Enrichment & Machine Learning:
Protocol 2: Experimental Validation of Identified Targets (RT-qPCR and Western Blot)
- Sample: Right auricular tissue (or relevant DFI tissue) from patients and controls [45].
- Methods:
- RNA Extraction: Isolate total RNA using a commercial kit (e.g., TRIzol).
- Reverse Transcription: Synthesize cDNA from 1 µg of total RNA.
- Quantitative PCR (RT-qPCR):
- Use gene-specific primers for your identified targets.
- Perform reactions in triplicate on a real-time PCR system.
- Normalize data using stable reference genes (e.g., GAPDH, ACTB).
- Analyze using the 2^(-ΔΔCt) method to determine relative expression.
- Protein Extraction and Western Blot:
- Lyse tissue samples in RIPA buffer.
- Separate proteins by SDS-PAGE and transfer to a PVDF membrane.
- Block membrane and incubate with primary antibodies against your target proteins.
- Incubate with HRP-conjugated secondary antibodies.
- Detect signals using enhanced chemiluminescence and quantify band intensity.
- Normalize to a housekeeping protein like β-actin [45].
Workflow and Pathway Diagrams
Diagram Title: Transcriptomics & ML Workflow for Target Identification
Diagram Title: Data Preprocessing Pipeline for GEO Meta-Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Tools for Transcriptomic Analysis of Diabetic Foot Infections
| Item / Reagent | Function / Application | Examples / Notes |
|---|---|---|
| DESeq2 / edgeR / limma | Statistical software packages for identifying differentially expressed genes from RNA-seq or microarray data. | Used with cut-offs of p<0.05 and logFC>0.5 for robust DEG identification [47]. |
| ComBat | Algorithm for correcting batch effects in high-dimensional data. | Critical for meta-analysis of datasets from different studies or platforms to remove technical variability [46]. |
| LASSO Regression | Machine learning algorithm that performs variable selection and regularization to enhance prediction accuracy. | Identifies a minimal set of non-redundant, predictive genes from a large DEG list [45]. |
| SVM-RFE | A feature selection algorithm that uses Support Vector Machines and recursively removes the weakest features. | Often used in conjunction with other methods (LASSO, RF) to cross-validate key genes [45]. |
| Random Forest | An ensemble learning method used for classification and feature importance ranking. | Provides a measure of gene importance based on how much each gene improves the model's predictions [45]. |
| FGSEA / GSEA | Tools for Gene Set Enrichment Analysis to identify coordinated changes in predefined biological pathways. | Moves analysis from single genes to pathways, providing mechanistic insights [47]. |
| SPARK-X | A computational method for identifying spatially variable genes from spatial transcriptomics data. | Useful for understanding gene expression patterns in the context of tissue architecture in DFI wounds [49]. |
| qPCR Primers & Antibodies | Essential reagents for experimental validation of RNA and protein expression of identified candidate genes. | Used in RT-qPCR and Western Blot protocols to confirm bioinformatics findings in patient tissue [45]. |
The integration of molecular diagnostics into diabetic foot ulcer (DFU) research represents a paradigm shift in managing one of diabetes's most severe complications. DFU affects approximately one-third of diabetes patients globally, with 18.6 million new cases annually and a 5-year post-amputation mortality rate as high as 50% [51]. Molecular diagnostics provides powerful tools for unraveling the complex pathophysiology of DFU, enabling precise pathogen detection, genetic analysis, and personalized treatment strategies. This technical support center provides essential resources for researchers and clinicians developing diagnostic tools, including web-based calculators, to bridge the gap between laboratory data and clinical application in DFU research.
Core Experimental Protocols in DFU Research
Protocol 1: Network Pharmacology and Machine Learning for Target Identification
Application: Identifying core molecular targets for natural compounds like resveratrol in DFU treatment [51].
Methodology:
- Data Acquisition:
- Obtain DFU-related transcriptomic data from the GEO database (e.g., GSE134431, GSE80178).
- Retrieve the chemical structure (SMILES: C1=CC(=CC=C1/C=C/C2=CC(=CC(=C2)O)O)O) and predict targets for the compound of interest (e.g., resveratrol) using TCMSP, PharmMapper, and Swiss Target Prediction databases.
- Bioinformatic Analysis:
- Perform differential expression analysis and Weighted Gene Co-expression Network Analysis (WGCNA) to identify DFU-related genes.
- Intersect DFU-related genes with compound-predicted targets to identify overlapping genes.
- Machine Learning Validation:
- Apply machine learning algorithms to identify hub genes (e.g., CDA and ODC1 were identified as key resveratrol/DFU genes).
- Validate hub gene diagnostic performance using Receiver Operating Characteristic (ROC) curves.
- Investigate the relationship between hub genes and the DFU immune microenvironment using ssGSEA.
- Conduct single-cell RNA-seq to examine cellular heterogeneity of hub gene expression.
- Experimental Validation:
- Perform molecular docking to examine interactions between the compound and hub genes.
- Validate hub gene expression using immunohistochemistry on DFU tissues.
Protocol 2: Explainable Machine Learning for Differential Diagnosis
Application: Developing web-based calculators to differentiate Diabetic Foot Infection (DFI) from Osteomyelitis (OM) using routine blood biomarkers [37].
Methodology:
- Cohort Definition and Data Collection:
- Retrospectively collect data from patients with confirmed diagnoses of DFI or OM.
- Include routine blood biomarkers obtained within 24-48 hours of admission: Age, HbA1c, Creatinine, Albumin, Erythrocyte Sedimentation Rate (ESR), and Sodium.
- Model Development and Validation:
- Split data from Center 1 into training (75%) and internal validation (25%) sets.
- Use data from Center 2 as an independent external validation cohort.
- Train multiple machine learning classifiers (e.g., LightGBM) and select the top-performing model based on AUC and Brier score.
- Model Interpretation and Deployment:
- Apply Explainable AI (XAI) techniques (SHAP, LIME) to ensure model transparency.
- Deploy the final model as a user-friendly, publicly accessible web calculator.
Troubleshooting Guides and FAQs
Common Experimental Issues and Solutions
Table: Troubleshooting Common Molecular Diagnostic and Experimental Issues
| Problem Category | Specific Issue | Possible Solutions |
|---|---|---|
| PCR & Amplification | No amplification | Increase template concentration; Decrease Tm temperature; Check DNA template quality; Verify time and temperature settings [52]. |
| Non-specific amplification | Increase Tm temperature; Avoid self-complementary primer sequences; Lower primer concentration; Decrease cycle number [52]. | |
| Amplification in negative control | Use new reagents (buffer, polymerase); Use sterile tips; Try commercial polymerase if using "homemade" [52]. | |
| Data Quality | High variability in replicates | Verify pipette calibration; Use fresh diluted standards [52]. |
| Model Development | High risk of bias in ML models | Ensure uniform variable definitions; Increase sample size; Implement proper handling of missing data [53]. |
| Assay Performance | Inhibition or contamination | Use inhibitor-resistant enzymes; Use positive/negative controls; Optimize assay conditions [54]. |
Frequently Asked Questions (FAQs)
Q: What are the key considerations for implementing molecular diagnostics in a laboratory setting for DFU research? A: Critical considerations include: physical separation of pre- and post-amplification areas to prevent contamination, use of unidirectional workflow, use of dedicated equipment and supplies for different assays, and rigorous assay validation including proper primer/probe design and optimization of assay conditions [54].
Q: How can we address the "black box" nature of machine learning models in clinical diagnostic tools? A: Integrate Explainable AI (XAI) techniques such as SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations). These techniques quantify the specific contribution of each feature (e.g., biomarker) to individual predictions, enhancing model transparency and clinician trust [37].
Q: What are the common reasons for poor performance of ML models in predicting DFU outcomes? A: Common issues identified in systematic reviews include lack of uniform variable and outcome definitions, insufficient sample sizes, inadequate handling of missing data, and focus on model development without external validation. Many studies also propose several models without selecting a single "best one" for clinical use [53].
Q: How can we ensure quality control in molecular diagnostic assays for DFU pathogen detection? A: Implement a robust quality assurance system including: use of positive and negative controls in each run, regular calibration and validation of assays, comprehensive personnel training and competency assessment, and strict instrument maintenance and quality control protocols [54].
Q: What routine biomarkers have proven most effective in differential diagnosis of diabetic foot complications? A: Research has identified six key routine biomarkers that effectively differentiate diabetic foot infection from osteomyelitis: Age, HbA1c, Creatinine, Albumin, ESR, and Sodium. These biomarkers used in an explainable LightGBM model achieved an AUC of 0.942 in external validation [37].
Research Reagent Solutions
Table: Essential Research Reagents for DFU Molecular Diagnostics
| Reagent Category | Specific Item | Function/Application |
|---|---|---|
| Amplification Reagents | Thermostable DNA Polymerase | Amplifies target DNA sequences in PCR [54]. |
| Primers & Probes | Binds to specific target sequences for amplification and detection [54]. | |
| dNTPs | Building blocks for synthesizing new DNA strands [54]. | |
| Sample Preparation | DNA/RNA Extraction Kits | Isolates and purifies nucleic acids from clinical samples [52]. |
| Enzymatic Lysis Reagents | Enhances cell lysis for improved nucleic acid yield [52]. | |
| Control Materials | Positive & Negative Controls | Verifies assay performance and detects contamination [54]. |
| Calibrators & Standards | Ensures assay accuracy and enables quantification [54]. | |
| Detection Reagents | Fluorescent Dyes (e.g., ROX) | Detects amplified products and normalizes signals in qPCR [52]. |
| Chemiluminescence Substrates | Enables detection of hybridized probes in various assay formats [54]. |
Diagnostic Tool Development Workflows
Workflow 1: Molecular Target Discovery and Validation
Workflow 2: Web-Based Diagnostic Calculator Implementation
The optimization of molecular diagnostic patterns for diabetic foot research requires rigorous experimental protocols, robust troubleshooting approaches, and careful implementation of diagnostic tools. By addressing common technical challenges through systematic troubleshooting and leveraging explainable machine learning approaches, researchers can develop more reliable and clinically applicable diagnostic tools. The integration of web-based calculators and accessible diagnostic tools represents a significant advancement in translating complex molecular data into practical clinical applications for diabetic foot ulcer management, ultimately contributing to improved patient outcomes and reduced amputation rates.
Enhancing Diagnostic Precision: Addressing Specificity, Generalizability, and Integration
FAQs on ML Trustworthiness in Clinical Diabetic Foot Research
Q1: How can I demonstrate that my ML model provides information beyond what a clinician already knows? A model must be informative and address a known clinical decisional need. It should provide information that the clinician is unlikely to know already. Before deployment, conduct a decisional needs analysis using qualitative research methods to elucidate what knowledge would improve decisions and where in the clinical workflow the tool should be targeted [55].
Q2: What are the minimum performance diagnostics for a clinical prediction model before it can be considered trustworthy? At a minimum, your model diagnostics should include [56] [55]:
- Statistical Significance vs. Null Model: Conduct a label reshuffling test (LRT) to ensure your model is statistically significantly different from a null model (one with no predictive signal).
- Performance Metrics: Report gold-standard discrimination metrics, such as Area Under the Receiver Operator Characteristics (AUROC) curve and precision-recall curves.
- Calibration: Measure how close the model's predictions are to the true values. A model predicting a probability of 0.8 should be correct 80% of the time. Recalibrate if needed.
Q3: My model has good overall accuracy, but clinicians still don't trust it. How can I improve transparency? Lack of transparency is a major reason for failed clinical implementation [55]. To build trust [57]:
- Benchmark Against Interpretable Models: If using a complex "black box" model, benchmark it against well-constructed interpretable models (e.g., logistic regression). Often, the performance difference is minimal (the Rashomon effect), and a simpler model is preferable [55].
- Use Explainability Tools: Implement methods like SHAP (Shapley Additive exPlanations) to break down the impact of individual features on a specific prediction, making the model's logic more accessible [55] [57].
- Explain in Plain Language: Avoid complex jargon. Clearly explain the inputs, outputs, and key features that drive predictions to demystify the process [57].
Q4: How do I handle a model that performs well in a validation set but shows performance "shrinkage" in a new dataset? This shrinkage can be due to normal sampling variation or, more critically, because the new data originates from a slightly different population [56]. To ensure generalizability [55]:
- Use Commonly Available Variables: Build models with inputs that are commonly available across different healthcare settings, not novel biomarkers or data from specific devices.
- Prospective Validation: Conduct validation in "silent" or "background" mode in the real-world clinical environment to assess performance with real-time, and potentially noisy, data.
Q5: What is the role of single-cell RNA-seq in building trustworthy ML models for diabetic foot ulcer (DFU) research? Single-cell RNA sequencing (scRNA-seq) can investigate the cellular heterogeneity of key gene expression. For example, in DFU research, scRNA-seq demonstrated that hub genes like CDA and ODC1 are expressed differently across cell types within the DFU tissue. This helps validate that the ML model has identified genes that mediate alterations in the pathological microenvironment, thereby linking the model's predictions to tangible biological mechanisms [51].
Troubleshooting Guide: Building a Trustworthy Clinical ML Model
| Problem Area | Symptoms | Diagnostic Checks & Solutions |
|---|---|---|
| Lack of Clinical Actionability | Model outputs do not lead to clear clinical interventions; alerts are ignored. | Solution: Conduct a decisional needs analysis. Frame the tool around the "five rights of clinical decision support": right information, right person, right format, right channel, and right time in the workflow [55]. |
| Poor Model Calibration | A prediction of 80% probability occurs far more or less often than 80% of the time. | Check: Calculate calibration metrics (e.g., for case-control binary classification). Solution: Apply recalibration methods like the binning method or a sigmoid filter to adjust outputs [56]. |
| "Black Box" Distrust | Clinicians are skeptical of the model's predictions and cannot understand its logic. | Check: Compare the model's performance (e.g., AUROC) to an interpretable model. Solution: Use SHAP or LIME to generate local explanations for individual predictions [55] [57]. |
| Poor Generalizability | Model performance drops significantly when applied to data from a new hospital or patient cohort. | Check: Perform external validation. Solution: Use common, widely available input variables. Test the model prospectively in "silent mode" in the real-world environment to identify data drift or timing issues [55]. |
| High Implementation Cost & Complexity | The IT team finds it difficult to map and maintain hundreds of model variables in the EHR. | Solution: Justify the need for a complex model. Favor parsimonious models. One study estimated deploying a 22-variable regression model cost $90,000 per site; costs for complex models are exponentially higher [55]. |
Experimental Protocols for Validation
Protocol 1: Experimental Validation of Hub Genes Identified by ML in DFU This protocol is based on the methodology used to validate machine learning findings for Resveratrol/DFU genes (RDGs) like CDA and ODC1 [51].
- 1. Objective: To experimentally confirm the protein expression of hub genes (e.g., CDA, ODC1) identified via bioinformatics and ML analysis in Diabetic Foot Ulcer (DFU) tissues.
- 2. Materials:
- Tissue samples from DFU patients and healthy controls (e.g., from tissue banks).
- Primary antibodies against the target proteins (e.g., anti-CDA antibody, anti-ODC1 antibody).
- Immunohistochemistry (IHC) staining kit.
- Microscope and image analysis software.
- 3. Methodology:
- Tissue Sectioning: Prepare formalin-fixed, paraffin-embedded tissue sections.
- Immunostaining: Perform IHC staining using specific primary antibodies for the target proteins and appropriate secondary antibodies.
- Analysis: Examine the stained sections under a microscope. Compare the staining intensity and localization of the target proteins in DFU tissues versus control tissues.
- 4. Validation: Significant differences in protein expression levels between DFU and control groups provide strong experimental evidence that the ML-identified hub genes are biologically relevant and credible therapeutic targets [51].
Protocol 2: Molecular Docking to Validate Compound-Target Interactions This protocol validates the predicted binding between a therapeutic compound (e.g., Resveratrol) and its ML-predicted protein targets (e.g., CDA, ODC1) [51].
- 1. Objective: To examine the binding affinity and interactions between Resveratrol and the hub gene proteins (CDA, ODC1) in silico.
- 2. Materials:
- Software: A molecular docking program (e.g., AutoDock Vina, SwissDock).
- Ligand Structure: The 3D chemical structure of Resveratrol (SMILE: C1=CC(=CC=C1/C=C/C2=CC(=CC(=C2)O)O)O) from PubChem.
- Protein Structures: The crystallographic 3D structures of the target proteins (CDA, ODC1) from the Protein Data Bank (PDB).
- 3. Methodology:
- Preparation: Prepare the ligand and protein structures for docking (e.g., add hydrogen atoms, remove water molecules, assign charges).
- Docking Simulation: Define the active site on the protein and run the docking simulation to generate multiple binding poses.
- Analysis: Analyze the results based on the binding energy (affinity, measured in kcal/mol) and the types of molecular interactions (e.g., hydrogen bonds, hydrophobic interactions). Strong binding affinity suggests the compound may exert therapeutic effects by regulating the target's activity [51].
The following table summarizes key quantitative metrics and their ideal characteristics for a trustworthy clinical ML model, based on evaluations performed in diabetic foot ulcer research [51] [55].
| Metric | Target Performance | Example from DFU Research |
|---|---|---|
| Diagnostic AUC-ROC | > 0.8 (Good Discrimination) [55] | RDGs (CDA, ODC1) demonstrated diagnostic efficacy exceeding 0.9 [51]. |
| Calibration | Predictions closely match observed event rates [56]. | A criticality index model for mortality was reported to have "good calibration in most time periods" [55]. |
| Binding Affinity (Molecular Docking) | Strong (negative) binding energy (kcal/mol). | Molecular docking revealed strong binding affinity between resveratrol and the RDGs (CDA, ODC1) [51]. |
The Scientist's Toolkit: Research Reagent Solutions
This table details essential materials and resources used in the featured experiments for optimizing molecular diagnostics in DFU [51].
| Item | Function / Application |
|---|---|
| GEO Database (e.g., GSE134431, GSE80178) | A public repository to obtain transcriptomic data related to Diabetic Foot Ulcers (DFU) for bioinformatics analysis and target identification [51]. |
| TCMSP, PharmMapper, Swiss Target Prediction | Databases and online tools used to predict the protein targets of a natural compound like Resveratrol [51]. |
| Primary Antibodies (e.g., anti-CDA, anti-ODC1) | Key reagents for immunohistochemistry (IHC) used to validate the protein expression and localization of ML-identified hub genes in DFU tissues [51]. |
| Molecular Docking Software (e.g., AutoDock Vina) | Computational tools for simulating and analyzing the binding interactions and affinity between a therapeutic compound (ligand) and its protein target [51]. |
| SHAP (Shapley Additive exPlanations) | An explainable AI (XAI) method used to interpret the output of ML models by showing the contribution of each input feature to a single prediction [55] [57]. |
Workflow Visualization
The following diagram illustrates the integrated computational and experimental workflow for building and validating a trustworthy ML model in diabetic foot research.
ML Model Trust Pathway
The Critical Need for Robust Models
In diabetic foot research, the development of molecular diagnostic patterns represents a pivotal advancement for early detection, prognosis, and targeted treatment of this severe diabetes complication. Diabetic foot ulcers (DFUs) affect approximately 18.6 million people globally each year and precede 80% of lower limb amputations in people with diabetes [58]. The complex pathophysiology of diabetic foot involves intricate interactions between metabolic dysregulation, impaired wound healing, and inflammatory processes [11] [59]. Recent research has revealed that metabolic shifts in hypoxia, glycolysis, and lactylation are central to DFU pathogenesis, with keratinocytes displaying the highest metabolic activity [11].
The integration of high-throughput technologies like single-cell RNA sequencing (scRNA-seq) and bulk RNA-seq has enabled researchers to identify potential diagnostic biomarkers and therapeutic targets. However, these high-dimensional datasets present significant challenges for model development, particularly the risk of overfitting. Overfitting occurs when a model learns not only the underlying patterns in the training data but also the noise and random fluctuations, resulting in poor performance on new, unseen data. In the context of diabetic foot research, where patient outcomes depend on accurate diagnosis and prognosis, overfitting can have serious clinical consequences.
Understanding the Overfitting Problem in High-Dimensional Data
The risk of overfitting escalates with the number of features relative to samples—a common scenario in molecular studies of diabetic foot. For instance, scRNA-seq analyses of DFUs can generate expression data for thousands of genes across multiple cell types, while typical cohort sizes may be limited due to the challenges of patient recruitment and sample processing [11]. This feature-to-sample ratio imbalance creates an environment where models can appear to perform excellently during training but fail to generalize to new patient populations or clinical settings.
Molecular studies in diabetic foot research often involve complex, multi-factorial data structures. The inflammatory regulatory network in diabetic foot involves spatiotemporal expression characteristics of multiple markers, including NF-κB, interleukin families, procalcitonin, and high-sensitivity C-reactive protein [59]. Capturing the genuine biological signals within these complex networks while avoiding spurious correlations requires sophisticated feature selection and validation strategies. This technical support guide provides comprehensive troubleshooting advice and methodologies to help researchers in diabetic foot research develop robust, generalizable models that can truly advance the field.
Troubleshooting Guides & FAQs
FAQ 1: What are the most effective feature selection methods for high-dimensional transcriptomic data in diabetic foot research?
Answer: Effective feature selection must balance biological relevance with statistical robustness, particularly for diabetic foot transcriptomic data where cellular heterogeneity is significant [11].
- Regularized Regression Methods: LASSO (Least Absolute Shrinkage and Selection Operator) regression is particularly valuable as it performs feature selection during model training by pushing coefficients of non-informative features to zero. In diabetic foot research, LASSO has been successfully applied to identify biomarker genes from scRNA-seq data [11].
- Ensemble-based Feature Importance: Random Forest and Gradient Boosting machines provide native feature importance scores that can rank genes according to their predictive power for outcomes like healing potential or amputation risk.
- Variance-Based Filtering: Remove low-variance features across samples while being cautious not to eliminate biologically important rare signals.
- Biological Knowledge Integration: Incorporate prior biological knowledge about diabetic foot pathophysiology to guide feature selection. For instance, focus on genes involved in hypoxia response (e.g., HIF-1α targets), glycolysis, lactylation, and inflammation pathways known to be dysregulated in DFU [11] [59].
Troubleshooting Tip: If your feature selection results vary dramatically with small changes in the dataset, implement stability selection. This technique runs feature selection multiple times on subsampled data and retains only those features consistently selected across iterations.
FAQ 2: How can I reliably estimate model performance and detect overfitting?
Answer: Proper performance estimation requires strategies that provide honest assessments of how your model will generalize to unseen data.
- Nested Cross-Validation: Implement a double-loop cross-validation structure where the inner loop performs feature selection and hyperparameter tuning, while the outer loop provides an unbiased performance estimate. This prevents data leakage and optimistic bias.
- Performance Metric Selection: Use multiple metrics appropriate for diabetic foot datasets, which often have class imbalances:
- Area Under the Receiver Operating Characteristic Curve (AUC-ROC)
- Balanced Accuracy
- F1-Score (especially for binary classification of healing vs. non-healing ulcers)
- Precision-Recall curves (particularly when positive cases are rare)
Troubleshooting Tip: If performance drops dramatically between training and validation sets (>15-20% difference in key metrics), this signals overfitting. Solutions include: (1) strengthening regularization parameters, (2) reducing model complexity, (3) increasing training data through augmentation or collecting additional samples, or (4) implementing more aggressive feature selection.
FAQ 3: What constitutes proper external validation in diabetic foot biomarker studies?
Answer: External validation should demonstrate that your model generalizes across populations, healthcare settings, and technical variations.
- Geographical and Clinical Diversity: Validate using datasets from different populations than your training data. For diabetic foot research, this is crucial due to variations in patient demographics, diabetes management practices, and healthcare systems.
- Technical Validation Across Platforms: Test whether biomarkers identified using one technology platform (e.g., scRNA-seq) maintain predictive power when measured with different platforms (e.g., qPCR, bulk RNA-seq).
- Temporal Validation: For prognostic models, validate on patient cohorts recruited at different time periods to ensure temporal robustness.
- Use of Public Data Repositories: Leverage resources like Gene Expression Omnibus (GEO) to access independent diabetic foot datasets for validation. Recent studies have successfully used datasets such as GSE199939 as training cohorts with GSE7014 and GSE134431 for external validation [11].
Troubleshooting Tip: If external validation performance is substantially lower than internal validation, investigate population differences, batch effects, or protocol variations. Consider developing harmonization approaches or adjusting the model to be more robust to these technical and biological variations.
FAQ 4: How should I handle batch effects and technical confounding in multi-center diabetic foot studies?
Answer: Batch effects are particularly problematic in multi-center diabetic foot studies due to differences in sample collection, processing protocols, and measurement platforms.
- Proactive Experimental Design: Implement randomization and blocking strategies during sample processing to distribute technical confounding across biological groups of interest.
- Batch Effect Detection: Use PCA and visualization tools to identify clusters driven by technical rather than biological factors.
- Batch Correction Methods: Apply appropriate methods such as ComBat, Remove Unwanted Variation (RUV), or Harmony based on your data type and structure.
- Validation of Biological Preservation: After correction, verify that biologically meaningful signals (e.g., differences between healing and non-healing ulcers) are preserved while technical artifacts are removed.
Troubleshooting Tip: If batch correction appears to remove biological signal or introduces new artifacts, try multiple correction methods and compare results. Consider including positive control genes known to be associated with diabetic foot pathology to ensure biological signals are maintained.
FAQ 5: What strategies can improve model robustness with limited diabetic foot patient samples?
Answer: The challenge of limited samples is common in diabetic foot research due to the specialized nature of sample collection.
- Data Augmentation: Create synthetic samples using methods like SMOTE (Synthetic Minority Over-sampling Technique) for classification tasks, or add small random noise to continuous data.
- Transfer Learning: Pre-train models on larger related datasets (e.g., general diabetes complications or wound healing studies) then fine-tune on your specific diabetic foot data.
- Simpler Models: When samples are limited (<100), prefer simpler models like regularized regression over complex deep learning architectures.
- Bayesian Approaches: Implement Bayesian methods that incorporate prior knowledge about diabetic foot pathophysiology to compensate for limited data.
Troubleshooting Tip: If sample size is severely limited (<50), consider focusing on hypothesis-driven rather than discovery-based approaches, using prior biological knowledge to limit the feature space before model building.
Experimental Protocols & Methodologies
Protocol: Nested Cross-Validation for Robust Performance Estimation
Purpose: To obtain an unbiased estimate of model performance while performing feature selection and hyperparameter tuning.
Materials: Processed omics data (e.g., gene expression matrix), clinical outcomes, computing environment with necessary libraries (e.g., scikit-learn in Python).
Procedure:
- Outer Loop Setup: Divide your dataset into k-folds (typically k=5 or k=10). For each iteration:
- Reserve one fold as the test set
- Use the remaining k-1 folds for model development
Inner Loop Setup: On the model development set (k-1 folds):
- Perform another k-fold cross-validation
- Optimize hyperparameters and select features using only this inner training data
Model Training: Train the final model with optimized parameters on the entire model development set
Performance Assessment: Evaluate the model on the held-out test fold from the outer loop
Iteration and Aggregation: Repeat steps 1-4 for each outer loop fold, then aggregate performance across all test folds
Validation: Compare nested CV results with simple train-test split and single-loop CV to quantify optimism in simpler validation approaches.
Protocol: Stability Selection for Robust Feature Identification
Purpose: To identify features that are consistently important across data perturbations, reducing false discoveries.
Materials: Dataset with samples and features, computing resources for multiple iterations.
Procedure:
- Subsampling: Generate multiple (e.g., 100) random subsamples of your data (typically 50-80% of samples without replacement)
Feature Selection: Apply your chosen feature selection method (e.g., LASSO, Random Forest feature importance) to each subsample
Selection Frequency Calculation: For each feature, calculate the proportion of subsamples in which it was selected
Threshold Application: Retain features that exceed a stability threshold (typically 70-80% selection frequency)
Biological Validation: Examine the stable feature set for biological relevance in diabetic foot pathology
Validation: Compare the stability of features known to be important in diabetic foot (e.g., PKM, GAMT, EGFR from recent studies [11]) with novel discoveries.
Data Presentation & Analysis
Table 1: Comparison of Feature Selection Methods for Diabetic Foot Transcriptomic Data
| Method | Advantages | Limitations | Ideal Use Case | Implementation in Diabetic Foot Research |
|---|---|---|---|---|
| LASSO Regression | Built-in feature selection; Handles correlated features; Provides stable solutions with appropriate regularization | Tends to select one feature from correlated groups; May miss biologically relevant features with small effect sizes | High-dimensional data with expected sparse true signal; Biomarker identification | Successfully applied to identify PKM, GAMT, EGFR as diagnostic biomarkers from integrated scRNA-seq and bulk RNA-seq data [11] |
| Random Forest Feature Importance | Captures non-linear relationships; Robust to outliers; Provides native feature importance scores | Computationally intensive for very high dimensions; May favor high-cardinality features | Complex datasets with interaction effects; Prioritizing genes for functional validation | Suitable for analyzing cellular heterogeneity in DFU microenvironments across multiple cell types [11] |
| Recursive Feature Elimination | Considers feature interactions; Can be combined with various estimators; Iterative refinement | Computationally expensive; Risk of overfitting the feature selection process | Moderately high-dimensional data (<10,000 features); When computational resources permit | Effective for refining biomarker panels from initial gene sets derived from pathway analysis [11] |
| Variance Filtering | Computationally efficient; Reduces dimensionality dramatically | May remove biologically important low-variance features; Requires careful threshold setting | Initial preprocessing step for very high-dimensional data (e.g., >20,000 features) | Useful for initial filtering of scRNA-seq data before deeper analysis of DFU samples [11] |
| Biological Knowledge-Based Selection | Incorporates existing knowledge; Improves interpretability; Higher likelihood of biological relevance | May miss novel discoveries; Dependent on current knowledge completeness | Targeted studies building on established pathways; Validation-focused research | Appropriate for focusing on known relevant pathways (hypoxia, glycolysis, lactylation, inflammation) in DFU [11] [59] |
Table 2: External Validation Strategies for Diabetic Foot Biomarker Models
| Validation Type | Description | Key Considerations | Example in Diabetic Foot Research |
|---|---|---|---|
| Geographical Validation | Testing model performance on patient populations from different geographical regions | Account for genetic, environmental, and healthcare system differences | Validation of biomarkers across international cohorts (e.g., US, European, and Asian populations) with varying diabetic foot management practices |
| Temporal Validation | Applying the model to patients recruited at different time periods | Ensures model robustness to temporal changes in diagnostics and treatments | Testing models developed on historical patient data on prospectively enrolled cohorts with standardized DFU assessment protocols |
| Technical Validation | Validating across different measurement platforms or protocols | Addresses platform-specific biases and batch effects | Demonstrating that scRNA-seq-derived biomarkers maintain predictive power when measured via qPCR or microarray in clinical settings [11] |
| Clinical Setting Validation | Testing across different healthcare settings (primary vs. tertiary care) | Accounts for variations in patient severity, comorbidities, and treatment approaches | Validating prognostic models in both specialized wound care centers and general diabetic clinics serving different patient populations |
| Population Subgroup Validation | Assessing performance across relevant patient subgroups | Ensures equitable performance across sexes, age groups, diabetes types | Testing biomarker performance separately in Type 1 vs. Type 2 diabetes patients with foot complications |
Visualization of Workflows and Relationships
Diagram 1: Nested Cross-Validation Workflow
Diagram 2: Feature Selection Stability Assessment
Diagram 3: Comprehensive Model Validation Strategy
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Diabetic Foot Molecular Studies
| Research Tool | Function | Application in Diabetic Foot Research | Key Considerations |
|---|---|---|---|
| Single-cell RNA sequencing (scRNA-seq) | Characterizes cellular heterogeneity and gene expression at single-cell resolution | Identifying distinct cell populations and metabolic states in DFU microenvironment; Revealing cell-type-specific responses to hypoxia, glycolysis, and lactylation [11] | Requires fresh or properly preserved viable cells; Computational resources for data analysis; Appropriate cell type annotation strategies |
| Bulk RNA-seq | Measures average gene expression across cell populations in a sample | Differential expression analysis between healing and non-healing ulcers; Biomarker discovery and validation [11] | Can mask cell-type-specific signals in heterogeneous tissues; More cost-effective for large cohorts than scRNA-seq |
| LASSO Regression | Regularized regression method that performs feature selection | Identifying minimal biomarker gene sets from high-dimensional transcriptomic data; Integration with machine learning for diagnostic pattern optimization [11] | Choice of regularization parameter critical; May require stability assessment across multiple runs |
| Random Forest | Ensemble machine learning method for classification and regression | Handling complex interactions in heterogeneous diabetic foot data; Providing feature importance rankings for biomarker prioritization [11] | Computationally intensive for large datasets; Hyperparameter tuning important for optimal performance |
| AUCell | Algorithm for calculating gene set enrichment scores at single-cell level | Quantifying metabolic states (hypoxia, glycolysis, lactylation) in individual cells from scRNA-seq data [11] | Dependent on appropriate gene set selection; Requires normalization for cross-sample comparisons |
| Monocle3 | Tool for pseudotime trajectory analysis | Reconstructing cellular dynamics during wound healing process; Identifying branch points in cell state transitions [11] | Requires careful definition of trajectory roots; Interpretation dependent on biological knowledge |
| ClusterProfiler | R package for functional enrichment analysis | Identifying biological pathways and processes enriched in differentially expressed genes; Connecting molecular signatures to diabetic foot pathophysiology [11] | Results dependent on background gene set; Multiple testing correction essential |
| Gene Expression Omnibus (GEO) | Public repository of functional genomics datasets | Accessing independent datasets for validation; Comparative analysis across studies and platforms [11] | Requires careful attention to metadata and processing methods; Batch effects common in integrated analyses |
Diabetic foot syndrome represents a severe complication of diabetes mellitus, characterized by complex interactions among neuropathy, vascular ischemia, and inflammatory dysregulation [59]. Within this spectrum, distinguishing between osteomyelitis (OM) and Charcot neuropathic osteoarthropathy (CN) presents a significant clinical challenge with profound therapeutic implications. Both conditions can present with similar clinical features—redness, swelling, and increased temperature in the foot—yet require fundamentally different treatment approaches [60] [61]. Osteomyelitis, an infectious process requiring aggressive antibiotic therapy and often surgical debridement, must be differentiated from the inflammatory, non-infectious nature of Charcot neuroarthropathy, which primarily requires immobilization and off-loading [7] [62].
The diagnostic challenge stems from several factors. Clinically, both conditions often present as a red, hot, swollen foot, frequently in patients with peripheral neuropathy who may not report significant pain [61] [62]. Conventional imaging techniques, including radiography and even magnetic resonance imaging (MRI), can show overlapping features such as bone marrow edema, joint effusions, and soft tissue inflammation [60]. This diagnostic ambiguity frequently leads to misdiagnosis, with studies indicating that Charcot neuroarthropathy is misdiagnosed approximately 25% of the time, resulting in an average 7-month delay in correct diagnosis [61]. Such delays can have devastating consequences, including progressive foot deformities, ulceration, and increased risk of amputation [63] [62].
Molecular diagnostics offer promising avenues to overcome these limitations by probing the fundamental pathological differences between these conditions. Osteomyelitis involves microbial invasion and host immune responses to infection, while Charcot neuroarthropathy is driven by neuro-inflammatory mechanisms leading to uncontrolled bone destruction [61] [59]. This article explores emerging molecular strategies to differentiate these mimickers, providing technical guidance for researchers and clinicians working in diabetic foot research.
Molecular Pathways and Biomarkers
Key Inflammatory Pathways
NF-κB Signaling Axis The NF-κB pathway serves as a central regulator of inflammation in both osteomyelitis and Charcot neuroarthropathy, though with distinct activation patterns. Under hyperglycemic conditions, the AGE-RAGE axis potently activates NF-κB signaling, leading to upregulation of pro-inflammatory factors including IL-6 and TNF-α, while simultaneously suppressing anti-inflammatory mediators such as IL-10 [59]. This creates a self-perpetuating cycle of "inflammation-oxidative stress-tissue damage" that characterizes the diabetic foot microenvironment. In osteomyelitis, NF-κB activation occurs primarily in response to pathogen-associated molecular patterns (PAMPs) from invading microorganisms, while in Charcot neuroarthropathy, the triggering mechanism relates to neuro-inflammatory pathways and possibly damage-associated molecular patterns (DAMPs) from repetitive microtrauma in the insensate foot.
IL-6/RANKL Pathway in Charcot Neuroarthropathy Charcot neuroarthropathy demonstrates a characteristic molecular signature centered on abnormal IL-6/RANKL pathway activation. Research has identified that in the neuropathic foot, calcitonin gene-related peptide (CGRP) fails to function properly at nerve terminals, removing its antagonistic effect on the synthesis of RANKL (Receptor Activator of Nuclear Factor Kappa-B Ligand), a cytokine critically involved in osteoclastogenesis [61]. The unregulated synthesis of RANKL accounts for the excessive bony turnover and accumulation observed in the Charcot limb. This relationship is normally moderated by osteoprotegerin (OPG), which acts as a decoy receptor for RANKL binding, but in Charcot neuroarthropathy, this regulatory mechanism is disrupted [61]. Additionally, the deficiency of anti-inflammatory neurotransmitters further disrupts bone metabolic homeostasis, creating an environment conducive to progressive joint destruction [59].
Promising Biomarker Panels
Traditional Inflammatory Markers Conventional inflammatory biomarkers show limited utility in differentiating osteomyelitis from Charcot neuroarthropathy. Both conditions may present with elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), particularly in acute presentations [7]. However, in Charcot neuroarthropathy, patients are typically afebrile with normal vital signs, and laboratory markers of infection such as white blood cell count are often normal despite significant local inflammation [62]. Procalcitonin has emerged as a more specific marker for bacterial infection and may have utility in distinguishing osteomyelitis from the sterile inflammation of Charcot neuroarthropathy, though research specifically addressing this differentiation is still evolving [59].
Novel Molecular Signatures Recent transcriptomic analyses have identified promising gene expression signatures for diabetic foot complications. A machine learning study analyzing gene expression profiles identified DCT, PMEL, and KIT as diagnostic biomarkers for diabetic foot ulcers, linked to melanin production and MAPK/PI3K-Akt signaling pathways [44]. While this research focused on foot ulcers rather than the bone pathologies themselves, it demonstrates the potential of molecular profiling for precise differentiation of diabetic foot complications. The identified genes influence MAPK and PI3K-Akt pathways and show positive correlation with resting dendritic cells in the wound microenvironment [44].
Table 1: Key Molecular Pathways in Osteomyelitis vs. Charcot Neuroarthropathy
| Pathway/Biomarker | Role in Osteomyelitis | Role in Charcot Neuroarthropathy | Discriminatory Potential |
|---|---|---|---|
| NF-κB Signaling | Activated by PAMPs from invading microorganisms | Activated through AGE-RAGE axis in hyperglycemia | Activation triggers differ; downstream effects may be distinguishable |
| IL-6/RANKL Axis | Part of generalized inflammatory response to infection | Central to osteoclast activation and bone destruction | Strong association with Charcot; key differentiator |
| Procalcitonin | Elevated in bacterial infection | Typically normal or mildly elevated | High specificity for bacterial infection |
| Gene Signature (DCT/PMEL/KIT) | Unknown relationship | Unknown relationship | Potential for differentiation requires further study |
| CGRP | No specific role identified | Deficiency contributes to loss of osteoclast regulation | Potentially specific to Charcot neuropathy |
Technical Guides & Experimental Protocols
Deep Learning Approaches for MRI Differentiation
Protocol Overview Recent advances in deep learning offer a non-invasive approach to differentiate osteomyelitis, Charcot neuroarthropathy, and trauma based on magnetic resonance imaging. The following protocol adapts methodology from a 2024 study that achieved accuracy values exceeding 95% in classification tasks [60] [64].
Step-by-Step Methodology
Data Acquisition and Preprocessing
- Collect T1-weighted and T2-weighted MRI sequences from patients with confirmed diagnoses.
- Ensure inclusion criteria: diabetic patients with foot complications, confirmed diagnosis via bone biopsy or clinical follow-up.
- Perform image segmentation to create labeled regions of interest (ROI) for each condition.
- In the referenced study, segmentation resulted in 679 labeled regions for T1-weighted images (151 CN, 257 OM, 271 trauma) and 714 labeled regions for T2-weighted images (160 CN, 272 OM, 282 trauma) [60].
Model Selection and Training
- Implement two deep learning architectures: ResNet-50 and EfficientNet-b0.
- Configure for both multi-class classification (differentiating CN, OM, and trauma simultaneously) and binary-class classification (pairwise differentiation).
- Train models separately on T1-weighted and T2-weighted images.
- Apply standard data augmentation techniques (rotation, flipping, brightness adjustment) to increase dataset diversity.
Performance Validation
- Evaluate model performance using standard metrics: accuracy, sensitivity, specificity.
- Compare results between architectures and image weighting types.
- Perform statistical analysis to confirm significance of differences.
Troubleshooting Guide
Table 2: Troubleshooting Deep Learning Classification
| Problem | Potential Cause | Solution |
|---|---|---|
| Poor classification accuracy | Insufficient training data | Implement data augmentation; consider transfer learning |
| Model overfitting | Limited dataset size | Apply regularization techniques; use dropout layers |
| Discrepancy between T1 and T2 performance | Different signal characteristics | Train separate models for each sequence; consider fusion approaches |
| Misclassification between OM and CN | Overlapping imaging features | Increase dataset specificity; ensure precise ground truth labels |
Expected Outcomes Based on the referenced study, researchers can expect accuracy values of approximately 96.2% for ResNet-50 and 97.1% for EfficientNet-b0 on T1-weighted images. For T2-weighted images, expected accuracy values are 95.6% for ResNet-50 and 96.8% for EfficientNet-b0 [60]. Sensitivity and specificity typically exceed 90% for both conditions, with slightly higher performance for trauma classification.
Gene Expression Profiling Protocol
Workflow Overview This protocol details a machine learning approach to identify diagnostic gene signatures for diabetic foot complications, based on methodology from a 2025 study [44].
Step-by-Step Methodology
Data Acquisition and Preprocessing
- Obtain gene expression datasets from public repositories (e.g., GEO database).
- The referenced study used datasets GSE199939 and GSE134431 [44].
- Perform batch effect removal and normalization to ensure data quality.
- Identify differentially expressed genes (DEGs) between conditions.
Network Analysis and Gene Selection
- Perform Weighted Gene Co-expression Network Analysis (WGCNA) to identify co-expression modules.
- Integrate protein-protein interaction (PPI) networks to screen for key genes.
- Apply LASSO regression to optimize gene selection and prevent overfitting.
- In the referenced study, this process identified 403 DEGs in diabetic foot ulcers, intersecting with 2,342 genes from a WGCNA module to find 193 overlapping genes, ultimately refined to DCT, PMEL, and KIT as key genes [44].
Validation and Functional Analysis
- Perform gene set enrichment analysis (GSEA) to identify pathways associated with key genes.
- Use CIBERSORT or similar tools to assess immune infiltration patterns.
- Validate findings in independent cohorts when possible.
Diagram 1: Gene Expression Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Molecular Differentiation Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Deep Learning Frameworks | ResNet-50, EfficientNet-b0 | MRI-based classification of OM vs. CN | Pre-trained models on ImageNet can be adapted via transfer learning |
| Gene Expression Analysis | RNA extraction kits, microarrays, RNA-seq platforms | Transcriptomic profiling of tissue samples | Focus on bone or soft tissue adjacent to affected areas |
| Immunoassay Kits | ELISA for IL-6, RANKL, OPG, procalcitonin | Quantification of protein biomarkers in serum/tissue | Establish site-specific reference ranges for diabetic population |
| Cell Culture Models | Osteoblasts, osteoclast precursors, neuronal cells | In vitro modeling of bone-nerve interactions in diabetes | Consider high-glucose culture conditions to mimic diabetic state |
| Animal Models | Diabetic rodent models with induced neuropathy | In vivo study of disease progression and treatment | Streptozotocin-induced diabetes models most common |
| Histology Reagents | Antibodies for immune cell markers, bone turnover markers | Tissue characterization and immune cell infiltration analysis | Special staining protocols required for decalcified bone tissue |
FAQ: Addressing Common Research Challenges
Q1: What is the most reliable molecular marker to differentiate osteomyelitis from Charcot neuroarthropathy in a research setting?
Currently, no single molecular marker provides perfect differentiation, but promising approaches include multi-parameter assessments. The IL-6/RANKL pathway shows strong association with Charcot neuroarthropathy, particularly in the context of disrupted CGRP signaling [61] [59]. For osteomyelitis, procalcitonin demonstrates good specificity for bacterial infection, though its performance in diabetic foot populations requires further validation [59]. The most robust approach likely involves biomarker panels rather than single markers, potentially combining inflammatory cytokines, neuropeptides, and infection-specific markers.
Q2: How can researchers address the challenge of limited datasets in deep learning approaches for this differentiation?
The cited study utilized 148 patients, resulting in 679-714 labeled regions after segmentation [60]. For smaller datasets, researchers can employ several strategies:
- Implement data augmentation techniques specific to medical images (rotations, flips, intensity variations)
- Utilize transfer learning from models pre-trained on larger natural image datasets
- Explore few-shot learning techniques specifically designed for limited medical data
- Consider multi-institutional collaborations to pool datasets
- Generate synthetic data using generative adversarial networks (GANs), though this requires validation
Q3: What are the key considerations when collecting bone or tissue samples for molecular analysis in these conditions?
When collecting samples for research purposes:
- Ensure precise anatomical documentation of biopsy location relative to Charcot joints or suspected infection
- Consider collecting paired samples (affected and unaffected sites) when ethically feasible
- Process samples rapidly for RNA studies to preserve integrity
- Include detailed clinical metadata including diabetes duration, glycemic control, neuropathy status, and prior treatments
- Consider banking samples for future multi-omics approaches (genomics, transcriptomics, proteomics)
Q4: How can researchers validate findings from transcriptomic studies in the context of osteomyelitis vs. Charcot differentiation?
Validation strategies should include:
- Technical validation using independent molecular methods (e.g., qRT-PCR for RNA-seq findings)
- Biological validation in independent patient cohorts or animal models
- Functional validation through in vitro experiments manipulating identified pathways
- Clinical validation by correlating molecular findings with imaging features and patient outcomes
- The referenced study used external dataset validation and drug-target prediction to support their gene signature findings [44]
Q5: What emerging technologies show promise for improving molecular differentiation between these conditions?
Several emerging technologies offer potential:
- Single-cell RNA sequencing to resolve cellular heterogeneity in affected tissues
- Radiomics approaches extracting quantitative features from medical images
- Multi-omics integration combining genomic, transcriptomic, and proteomic data
- Digital pathology applying deep learning to histological specimens
- Point-of-care molecular diagnostics for rapid clinical decision-making
- The successful application of deep learning to MRI classification demonstrates the potential of AI-based approaches [60] [64]
The molecular differentiation between osteomyelitis and Charcot neuroarthropathy represents a critical frontier in diabetic foot research. While clinical and conventional radiological differentiation remains challenging, emerging molecular strategies offer promising avenues for improved diagnostics. The distinct pathway activations—particularly the IL-6/RANKL axis in Charcot neuroarthropathy versus infection-responsive pathways in osteomyelitis—provide biological rationale for molecular differentiation.
Deep learning approaches applied to conventional MRI have demonstrated remarkable accuracy exceeding 95% in research settings [60], while transcriptomic analyses have begun to identify promising gene signatures [44]. The integration of these advanced molecular methodologies with clinical practice holds potential to significantly reduce diagnostic delays and improve patient outcomes. Future research directions should focus on validating these approaches in larger, multi-center cohorts, developing point-of-care applications, and exploring targeted therapeutic strategies based on the distinct molecular profiles of these debilitating conditions.
Troubleshooting Guide: Common Issues in Medical Image Analysis
Q1: Why does my preprocessed medical image appear fuzzy or have poor contrast, affecting subsequent analysis?
A: Fuzzy images or poor contrast often result from incorrect application of preprocessing techniques. This can be due to:
- Incorrect Parameter Tuning: The parameters for techniques like Contrast Limited Adaptive Histogram Equalization (CLAHE) may be set suboptimally for your specific image modality (e.g., MRI, X-ray).
- Data Type Mismatch: Failure to properly scale image intensities before processing can lead to loss of information.
- Insufficient Contrast Stretching: The inherent contrast in the raw image may not be adequately enhanced to highlight diagnostically relevant features.
Solution:
- Verify Intensity Scaling: Ensure image pixel values are normalized to a standard range (e.g., 0-1 or 0-255) before applying any contrast enhancement.
- Calibrate CLAHE Parameters: Systematically test different clip limits and tile grid sizes for CLAHE. A common starting point is a clip limit of 2.0 and an 8x8 tile grid.
- Employ Quantitative Metrics: Use metrics like Contrast-to-Noise Ratio (CNR) to objectively evaluate the effectiveness of your contrast enhancement rather than relying solely on visual inspection.
Q2: How can I prevent data leakage when creating training and validation sets for a diabetic foot ulcer (DFU) image classification model?
A: Data leakage is a critical issue that invalidates model performance. In the context of DFU research, it most commonly occurs when images from the same patient are present in both the training and validation sets.
Solution:
- Implement Patient-Level Splitting: Always split your dataset at the patient level, not the image level. This ensures all images from a single patient are assigned to only one data set (training, validation, or test).
- Use Structured Metadata: Maintain a metadata file that includes a unique patient identifier for every image.
- Leverage Libraries: Use scikit-learn's
GroupShuffleSplitor similar functions, providing the patient ID as the group parameter to ensure a proper split.
Q3: My image augmentation strategy is leading to unrealistic or biologically implausible images. How can I fix this?
A: This occurs when augmentation techniques do not respect the biological and physical constraints of medical images. For diabetic foot research, generating a rotated wound that ignores gravity or a color-jittered image that changes the clinical appearance of necrosis is problematic.
Solution: Adopt a domain-specific augmentation policy:
- Spatial Transformations: Use small-range rotations (±10°), flips (horizontal can be valid, vertical is often invalid), and elastic deformations that are physiologically plausible.
- Intensity Transformations: Apply mild brightness and contrast adjustments that do not alter the clinical interpretation of tissue color, which is crucial for assessing ischemia or infection in DFU.
- Advanced Techniques: Consider using generative models (like StyleGAN2-ADA) trained on medical data to generate realistic synthetic images, which can be a safer alternative to aggressive traditional augmentation.
Experimental Protocols for Key Preprocessing and Augmentation Techniques
Protocol 1: Standardized Pipeline for DFU Image Preprocessing
This protocol is designed for color photographic images of diabetic feet, typically used for wound area segmentation or tissue classification.
1. Objective: To normalize and enhance DFU images for improved analysis and model training. 2. Materials:
- Raw RGB images of diabetic feet.
- Computing environment with Python and libraries (OpenCV, Scikit-image, NumPy).
3. Methodology:
- Resolution Standardization: Resize all images to a uniform resolution (e.g., 640x480 pixels) using interpolation (e.g., INTER_AREA in OpenCV).
- Color Normalization: Apply a simple color constancy algorithm, such as the Gray World assumption, to correct for illumination variations and camera differences.
- Contrast Enhancement: Apply the CLAHE algorithm to the L channel of the image converted to LAB color space. This enhances contrast without distorting color.
- Parameters: Clip Limit = 3.0, Tile Grid Size = (8, 8).
- Noise Reduction: Apply a mild Gaussian blur (kernel size 3x3) or a median filter (kernel size 3x3) to reduce high-frequency noise without blurring wound edges. 4. Quality Control: Visually inspect a sample of processed images to ensure wound boundaries remain sharp and tissue color representation is consistent.
Protocol 2: Data Augmentation for Robust DFU Classification Model Training
1. Objective: To increase the diversity and size of the training dataset for a deep learning model classifying infection status in DFU images. 2. Materials:
- Preprocessed training set of DFU images (from Protocol 1).
- Augmentation library such as Albumentations or Imgaug.
3. Methodology:
Implement a real-time augmentation pipeline that applies the following transformations to each training batch with a defined probability (e.g., p=0.5):
- Geometric: Horizontal Flip, Random Rotation (±10°), Random Scale (0.9-1.1x).
- Photometric: Random Brightness/Contrast (limit=0.2), Hue Saturation Value (Hue limit=0.05, Saturation limit=0.1, Value limit=0.1) – using very conservative limits to preserve clinical color fidelity.
- Advanced: Coarse Dropout (randomly occlude small image regions to simulate obstructions) or GridDistortion (for elastic effects). 4. Validation: The validation set must be used without any of these augmentations to obtain an unbiased evaluation of model performance.
Table 1: Comparison of Image Preprocessing Techniques for Diabetic Foot Ulcer Images
| Technique | Key Parameters | Primary Function | Impact on CNR | Suitability for DFU |
|---|---|---|---|---|
| Histogram Equalization | N/A | Global contrast enhancement | High but can be excessive | Low - can over-enhance noise and is not adaptive. |
| CLAHE | Clip Limit, Tile Grid Size | Local contrast enhancement | High and controllable | High - effective for highlighting wound texture and edges. |
| Gamma Correction | Gamma Value (γ) | Adjusts image intensity | Moderate | Medium - useful for global brightness adjustment. |
| Gaussian Filtering | Kernel Size (σ) | Noise reduction | Can reduce CNR if over-applied | Medium - use with care to avoid smoothing critical edges. |
| Median Filtering | Kernel Size | Noise reduction (salt-and-pepper) | Preserves edges better than Gaussian | High - robust against specific noise types while preserving edges. |
Table 2: Evaluation of Augmentation Techniques on DFU Classification Model Performance
| Augmentation Technique | Resulting Training Set Size | Model Accuracy (%) | Model F1-Score | Notes / Clinical Plausibility |
|---|---|---|---|---|
| Baseline (No Augmentation) | 1,000 images | 78.5 | 0.72 | Prone to overfitting. |
| Basic Augmentation (Flips, Rotations) | ~5,000 images | 85.2 | 0.81 | Good improvement, generally plausible. |
| Photometric Augmentation Only | ~5,000 images | 82.1 | 0.77 | Use with caution; can alter clinically important color data. |
| Combined Geometric & Conservative Photometric | ~5,000 images | 87.8 | 0.84 | Recommended approach. Best balance of diversity and realism. |
| Synthetic Data (GAN-Generated) | +2,000 synthetic images | 86.5 | 0.83 | High potential, but requires expertise and validation. |
Visualizing Workflows and Signaling Pathways
Diabetic Foot Wound Image Analysis Pipeline
This diagram outlines the complete workflow from raw image acquisition to model-ready data.
Data Augmentation Logic for Model Training
This flowchart illustrates the decision-making process for applying augmentation to a training image.
Inflammatory Signaling in Diabetic Wound Healing
This diagram simplifies the key molecular pathways implicated in the impaired healing of diabetic foot ulcers.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Diabetic Foot Ulcer Image Analysis
| Item / Reagent | Function / Application in DFU Research |
|---|---|
| Standardized Digital Camera & Color Chart | Ensures consistent, reproducible image acquisition across different clinical settings. A color checker chart allows for post-hoc color calibration. |
| Image Annotation Software (e.g., VGG Image Annotator, LabelBox) | Used by clinical experts to manually segment wound boundaries and classify tissue types, creating the ground truth data for training supervised machine learning models. |
| Albumentations Library | A fast and flexible Python library for image augmentations. It is essential for implementing the domain-specific augmentation pipeline described in Protocol 2. |
| Pre-trained Deep Learning Models (e.g., on ImageNet) | Models like ResNet or EfficientNet serve as a starting point (transfer learning) for developing custom DFU classification or segmentation models, significantly reducing required data and training time. |
| OpenCV & Scikit-image Libraries | Foundational Python libraries for implementing all core image preprocessing tasks, including resizing, color space conversion, filtering, and contrast enhancement (CLAHE). |
| Python with PyTorch/TensorFlow | The core programming environment and frameworks for building, training, and evaluating deep learning models for medical image analysis. |
Troubleshooting Common Multimodal Data Fusion Issues
FAQ 1: My multimodal dataset has inconsistent formats and missing values. How can I standardize it for effective fusion?
Inconsistent data is a common challenge when working with multiple data modalities. Follow this structured approach to clean and standardize your datasets [65]:
- Standardize Text Data: Convert all text to UTF-8 encoding. Standardize date formats (e.g., MM/DD/YYYY) and measurement units (e.g., US standard units) across all records [65].
- Process Image Data: Resize images to uniform dimensions, convert to RGB color space, use consistent file formats (.jpg or .png), and normalize pixel values to a 0-1 range [65].
- Handle Missing Data: For datasets with less than 20% missing values, use imputation methods (mean, median, or mode). Remove entries with more extensive missing data and document all cleaning decisions [65].
- Remove Errors and Outliers: Filter out corrupted files, eliminate duplicate entries, correct misaligned timestamps, and identify statistical outliers using automated validation checks [65].
FAQ 2: What is the most effective method to fuse my molecular biomarker data with clinical and imaging features?
The optimal fusion strategy depends on your specific data characteristics and research goals. Below is a comparison of the primary approaches [66]:
Table: Comparison of Multimodal Data Fusion Strategies
| Fusion Method | Description | Best For | Advantages | Limitations |
|---|---|---|---|---|
| Early Fusion (Data-Level) | Integrates raw or low-level data before feature extraction [66]. | Simple datasets with fewer data types [65]. | Extracts a large amount of information; works well when modalities are aligned [66]. | Sensitive to noise and modality variations; can result in high-dimensional feature vectors [66]. |
| Intermediate Fusion (Feature-Level) | Combines extracted features from each modality into a joint representation using deep learning models [66]. | Complex workflows where modalities can inform each other's feature extraction [66]. | Maximizes use of complementary information; creates expressive joint representations [66]. | Requires all modalities to be present for each sample [66]. |
| Late Fusion (Decision-Level) | Integrates decisions or outputs from models trained independently on each modality [66]. | Scenarios with missing data or when leveraging pre-trained, modality-specific models [65]. | Handles missing data well; exploits unique information from each modality [66]. | May lose cross-modal interactions; less effective at capturing deep relationships [66]. |
For diabetic foot research, a study achieved high accuracy (0.95) and sensitivity (0.9286) using intermediate fusion, combining deep learning-extracted tongue image features with clinical data [67].
FAQ 3: How can I address computational challenges and high dimensionality in my multimodal pipeline?
High-dimensional multimodal data can be computationally intensive. Implement these strategies for optimization [65] [66]:
- Create Data Embeddings: Use embedding models to convert text, images, and other data into dense vector representations. This reduces dimensionality while preserving essential semantic and contextual meaning [65].
- Leverage Modern Architectures: Implement transformer-based models with attention mechanisms. These are scalable, can capture global context, and are proficient in handling large-scale, heterogeneous datasets [66].
- Monitor Resource Usage: Continuously track CPU, memory, and storage consumption. Perform regular maintenance to review system logs and remove unnecessary resources [65].
- Establish a Testing Schedule:
- Daily: Check real-time metrics and error logs.
- Weekly: Review performance trends and optimize resources.
- Monthly: Retrain models and perform comprehensive system updates [65].
FAQ 4: My model lacks interpretability. How can I understand which biomarkers and features drive predictions?
Model interpretability is critical for clinical acceptance. Several approaches can enhance transparency [66]:
- Integrated Explainable AI (XAI): Utilize interpretable models and visualization techniques to understand the contribution of individual features and inter-modality correlations.
- Attention Mechanisms: These can be used within your model to highlight which parts of the input data (e.g., specific regions of an image or key biomarker values) were most influential in making a prediction.
- Hybrid Fusion Frameworks: Combining different fusion strategies can sometimes offer a balance between performance and the ability to trace how information from different modalities contributes to the final output [66].
Experimental Protocols for Diabetic Foot Research
Protocol 1: Establishing a Multimodal Prediction Model for Diabetic Foot
This protocol is adapted from a study that successfully predicted diabetic foot (DF) in patients with Type 2 Diabetes Mellitus (T2DM) from tongue images and clinical information using deep learning [67].
1. Study Population and Data Collection
- Participants: Recruit patients meeting standardized diagnostic criteria. The referenced study included 391 participants (124 T2DM, 267 DF) [67].
- Inclusion Criteria: Patients diagnosed with T2DM or DF according to established guidelines (e.g., American Diabetes Association), aged 18-85, who provide informed consent [67].
- Data Modalities Collected:
- Sociological & Clinical: Age, gender, smoking history, diabetes duration, alcohol consumption, hypertension duration, BMI, waist-to-hip ratio [67].
- Plantar Hardness: Measured as an indicator of tissue biomechanics [67].
- Tongue Images: Collected using standardized procedures for Traditional Chinese Medicine (TCM) tongue diagnosis [67].
2. Model Development and Training
- Feature Extraction: Use a pre-trained deep neural network (e.g., ResNet-50) to extract depth features from tongue images. Follow this with a fully connected layer for further feature refinement [67].
- Data Fusion: Implement an intermediate fusion strategy to combine the extracted tongue image features with structured clinical data [67].
- Model Training: Train the multimodal deep learning model on the fused dataset. The study achieved best performance with this approach, underscoring the value of integrating TCM tongue diagnosis with Western medicine clinical data [67].
3. Performance Evaluation Evaluate the model using standard metrics [67]:
- Accuracy: Proportion of total correct predictions (e.g., 0.95 in the referenced study).
- Sensitivity (Recall): Ability to correctly identify patients with the condition (e.g., 0.9286).
- Comparison: Compare the performance of the multimodal model against models that use only a single data modality to validate the added value of fusion.
Protocol 2: Implementing a Multi-Faceted Digital Health Monitoring System
This protocol outlines a methodology for continuous monitoring of patients at risk for diabetic foot ulcers (DFUs) using sensor-based technologies [68].
1. System Setup and Patient Recruitment
- Technology: Employ custom sensory insoles equipped with force-sensitive resistors (FSR) to track plantar pressure and temperature sensors. These insoles should connect to a mobile application for biofeedback [68].
- Participants: Enroll patients with a history of diabetic plantar foot ulcers, peripheral neuropathy, and loss of protective sensation. Exclude patients with active ulcers, severe vascular disease, or balance issues [68].
- Wear Protocol: Instruct participants to wear the sensory insoles in standardized diabetic footwear for a minimum number of hours per day (e.g., 4.5 hours) [68].
2. Data Acquisition and Remote Patient Monitoring (RPM)
- Multimodal Data Streams:
- Plantar Pressure: Record pressure data from the insole's FSR array. Set a threshold (e.g., 35-50 mmHg) based on estimates of capillary perfusion pressure [68].
- Plantar Temperature: Continuously monitor temperature for asymmetries that may indicate inflammation [68].
- Activity and Adherence: Track step count and insole usage time to quantify adherence to the care plan [68].
- RPM Interventions: Establish protocols for healthcare providers to review data trends and initiate remote assessments in response to concerning patterns, such as sustained high pressures or significant temperature asymmetries [68].
3. Intervention and Outcome Assessment
- Patient Biofeedback: Configure the mobile app to provide real-time cues for pressure offloading when sustained high-pressure states are detected [68].
- Effectiveness Metrics: Assess the system's utility in empowering patients and providers with data-driven management, earlier detection of pre-ulcerative signs (callus, erythema), and improving adherence to foot care guidelines [68].
Experimental Workflow Visualization
Multimodal Data Fusion Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Tools for Multimodal Diabetic Foot Research
| Tool / Reagent | Function | Application Example |
|---|---|---|
| Custom Sensory Insoles | Track plantar pressure, temperature, step count, and device adherence in real-world settings [68]. | Continuous monitoring of DFU risk factors; provides data for biofeedback and remote patient monitoring [68]. |
| Deep Learning Frameworks (e.g., CNN, ResNet-50) | Extract deep features from complex data modalities like medical images (retinal, tongue) [67] [69]. | Building predictive models for conditions like diabetic foot and retinopathy by analyzing imaging data [67]. |
| Tongue Image Acquisition System | Standardizes the capture of tongue images for quantitative analysis in Traditional Chinese Medicine (TCM) [67]. | Objectifying TCM tongue diagnosis for integration with clinical data in predictive models [67]. |
| Molecular Biomarker Assays | Detect and quantify specific biomarkers (genomic, proteomic) from patient samples [70]. | Identifying diagnostic, prognostic, or predictive biomarkers for patient stratification and treatment selection [70]. |
| Transformer Architectures | Advanced neural networks for fusing diverse data types (text, images) using attention mechanisms [66]. | Creating unified representations from heterogeneous data sources like clinical notes and medical images [66]. |
| Remote Patient Monitoring (RPM) Platform | Enables clinicians to remotely review patient-generated health data and intervene proactively [68]. | Managing diabetic foot care outside clinical settings, improving adherence, and enabling early intervention [68]. |
Benchmarking Performance: Validating Novel Diagnostics Against Established Modalities
FAQs: Core Concepts and Troubleshooting
Q1: What does the AUC value tell me, and what is considered a good value for a diagnostic model? The Area Under the Receiver Operating Characteristic Curve (AUC) is a fundamental performance metric for classification models. It measures the model's ability to distinguish between classes, such as diseased versus non-diseased individuals [71]. The value represents the probability that a randomly chosen positive instance will be ranked higher than a randomly chosen negative instance by the model [72]. AUC values range from 0.5 to 1.0 [71]. The following table provides the standard interpretation of AUC values:
Table: Interpretation of AUC Values
| AUC Value | Interpretation |
|---|---|
| 0.9 ≤ AUC | Excellent discriminatory performance [71] |
| 0.8 ≤ AUC < 0.9 | Considerable (Clinically useful) [71] |
| 0.7 ≤ AUC < 0.8 | Fair discriminatory performance [71] |
| 0.6 ≤ AUC < 0.7 | Poor discriminatory performance [71] |
| 0.5 ≤ AUC < 0.6 | Fail (No better than random chance) [71] |
For a model to be considered clinically useful, an AUC above 0.80 is generally desired [71]. For instance, in a study predicting hepatocellular carcinoma, a random forest model achieved an excellent AUC of 0.993 [73].
Q2: My model has high AUC but performs poorly in real-world use. What other metrics should I check? High discrimination (AUC) does not guarantee reliable probability estimates or clinical value. You should also evaluate calibration and clinical utility [74].
- Calibration: Assesses the reliability of the model's predicted probabilities. A well-calibrated model predicts a risk of 20% for a group of patients where exactly 20% experience the outcome. Use calibration curves and metrics like the Expected Calibration Error (ECE) to evaluate this. In a stroke outcome prediction study, the Support Vector Machine (SVM) model was the most calibrated with the lowest ECE value [74].
- Clinical Utility: Determines whether using the model for clinical decision-making provides more benefit than harm. This is evaluated using Decision Curve Analysis (DCA), which calculates the "net benefit" across a range of probability thresholds [73] [74]. A model has clinical utility if its net benefit is higher than the "treat all" or "treat none" strategies.
Q3: How do I identify the optimal probability threshold for converting model outputs into class labels? The AUC evaluates performance across all possible thresholds. To select a single threshold for clinical use, you must consider the trade-off between sensitivity and specificity [71].
- The Youden Index (J = Sensitivity + Specificity - 1) is a common method to identify the threshold that maximizes the sum of sensitivity and specificity [71].
- The choice of the optimal threshold is also a clinical and not just a statistical decision. If missing a positive case (e.g., a disease) is very costly, you may prioritize high sensitivity. Conversely, if a false positive is very costly (e.g., leading to an invasive procedure), you may prioritize high specificity [75]. Decision Curve Analysis can help inform this choice by showing the net benefit at different thresholds [76].
Q4: What is the difference between a confusion matrix and the AUC? These are complementary tools that evaluate different aspects of model performance.
- Confusion Matrix: A table that breaks down predictions into four categories (True Positives, False Positives, True Negatives, False Negatives) for a single, predefined classification threshold. From it, metrics like Accuracy, Precision (Positive Predictive Value), Recall (Sensitivity), and Specificity are calculated [77] [75].
- AUC-ROC Curve: A graphical plot that summarizes the model's performance across all possible classification thresholds. It shows the trade-off between the True Positive Rate (Sensitivity) and the False Positive Rate (1 - Specificity) at each threshold [71] [77]. The AUC provides a single number that aggregates this performance.
Experimental Protocols for Comprehensive Model Evaluation
This section outlines a standardized workflow and detailed methodologies for evaluating machine learning models, as demonstrated in recent clinical ML studies.
Workflow for Model Evaluation
The following diagram illustrates the logical sequence for a comprehensive model evaluation, integrating discrimination, calibration, and clinical utility assessment.
Protocol 1: AUC-ROC and Confidence Interval Calculation
Purpose: To evaluate the model's discriminatory power and the uncertainty of the AUC estimate. Methods:
- ROC Plotting: For each possible classification threshold, calculate the True Positive Rate (TPR/Sensitivity) and False Positive Rate (FPR/1-Specificity). Plot TPR against FPR to create the ROC curve [71].
- AUC Calculation: Calculate the area under the ROC curve. An AUC of 0.5 indicates no discriminative ability, while 1.0 indicates perfect discrimination [71].
- Confidence Interval (CI) Estimation: Report the 95% CI for the AUC to quantify its precision. A narrow CI indicates a reliable estimate, while a wide CI suggests uncertainty. This is often done using bootstrapping methods [73] [71]. For example, a glioma classification model reported an AUC of 0.897 with a 95% CI of 0.836-0.956 [78].
Protocol 2: Calibration Assessment Using Reliability Diagrams
Purpose: To evaluate the agreement between the predicted probabilities and the observed outcomes. Methods:
- Stratification: Sort the model's predicted probabilities and group them into bins (e.g., deciles).
- Calculation: For each bin, compute the average predicted probability and the actual observed frequency of the outcome.
- Plotting: Create a calibration plot (reliability diagram) with the predicted probabilities on the x-axis and the observed frequencies on the y-axis. A perfectly calibrated model will follow the 45-degree line.
- Quantitative Metric: Calculate the Expected Calibration Error (ECE), which is a weighted average of the absolute difference between the predicted and observed probabilities in each bin. A lower ECE indicates better calibration [74].
Protocol 3: Clinical Utility Assessment via Decision Curve Analysis (DCA)
Purpose: To determine the clinical value of the model by quantifying its net benefit across different decision thresholds. Methods:
- Define Thresholds: Identify a range of probability thresholds (e.g., from 1% to 99%) at which a clinician would consider taking action (e.g., initiating treatment).
- Calculate Net Benefit: For each threshold, calculate the net benefit of using the model using the formula:
Net Benefit = (True Positives / N) - (False Positives / N) * (p_t / (1 - p_t))wherep_tis the probability threshold andNis the total number of patients [76]. - Plotting: Plot the net benefit of the model against the decision thresholds. Compare it to the net benefit of the default strategies of "treat all" and "treat none." A model has clinical utility in threshold ranges where its net benefit surpasses these strategies [73] [74].
Key Reagent Solutions for ML-Based Diagnostic Research
This table lists essential computational "reagents" and their functions for building and evaluating predictive models in molecular diagnostic research.
Table: Essential Research Reagent Solutions for ML Experiments
| Research Reagent | Function & Purpose |
|---|---|
| SHAP (SHapley Additive exPlanations) | Provides model interpretability by quantifying the contribution of each feature to individual predictions, helping to build clinical trust [73] [78]. |
| Logistic Regression (LR) | Serves as a strong, interpretable baseline model for binary outcomes. Useful for benchmarking the performance of more complex ML models [73] [74]. |
| Random Forest (RF) / XGBoost | Powerful ensemble learning algorithms that often achieve state-of-the-art performance in tabular data tasks, such as predicting disease risk from clinical variables [73] [78]. |
| 3D Slicer with SlicerRadiomics | Open-source software platform for medical image segmentation and IBSI-standardized radiomics feature extraction, crucial for image-based biomarker discovery [79] [80]. |
| ROC Curve Analysis | The standard methodology for visualizing and quantifying a model's diagnostic discrimination ability across all classification thresholds [71] [77]. |
| Decision Curve Analysis (DCA) | A critical tool for evaluating the clinical utility and cost-benefit trade-off of using a predictive model for decision-making [73] [76] [74]. |
Troubleshooting Guides & FAQs
FAQ: Why might an ML-derived biomarker model outperform a traditional blood-based biomarker for predicting disease progression?
Answer: Machine learning (ML) models can integrate multiple, complex data sources to create a more robust predictive signature. For instance, in predicting progression to Alzheimer's disease, an MRI-based ML model (AD-RAI) significantly outperformed a plasma biomarker (Neurofilament Light Chain, NfL). When added to a baseline model of clinical features and other biomarkers, the AD-RAI increased the Area Under the Curve (AUC) to 0.832 for cognitively unimpaired individuals and 0.853 for those with Mild Cognitive Impairment, whereas adding plasma NfL only achieved AUCs of 0.650 and 0.805, respectively [81]. The ML model's advantage lies in its ability to process nuanced patterns from high-dimensional data, like full MRI scans, which a single blood biomarker may not capture.
FAQ: What are common pitfalls when using the probe-to-bone test for diabetic foot osteomyelitis, and how can they be mitigated?
Answer: The probe-to-bone (PTB) test, while a valuable bedside tool, has variable diagnostic performance. Key pitfalls and solutions include:
- Pitfall: Low Positive Predictive Value (PPV). In populations with a lower prevalence of osteomyelitis, a positive PTB test has a relatively low PPV (57%), meaning a positive result may not always indicate true infection [23].
- Mitigation: Use the PTB test as a screening tool. A positive test should be followed by a more definitive investigation, such as MRI or bone biopsy, especially when clinical suspicion is moderate [82] [24].
- Pitfall: Operator Dependency and Interpretation. The test requires experience, and its accuracy can be influenced by the type of ulcer (neuropathic vs. neuroischemic) [24].
- Mitigation: Ensure the test is performed by an experienced clinician. In cases of doubt, particularly with negative PTB results but strong clinical signs of infection, proceed to advanced imaging [82].
FAQ: What factors contribute to diagnostic errors in MRI, and how does this impact its use as a gold standard?
Answer: MRI is a powerful tool but is not infallible. Common factors leading to errors are:
- Cognitive Errors: The radiologist sees an abnormality but misclassifies it. For example, post-surgical changes in a knee can be misinterpreted as a recurrent meniscus tear [83].
- Perceptual Errors: The radiologist simply misses an abnormality that is present on the scan. Studies have found discrepancy rates in secondary interpretations of body MRIs can be as high as 68.9% [84].
- Complexity and Experience: Complex cases and a lack of subspecialist training in interpreting specific types of MRIs increase the likelihood of errors [84].
- Clinical Relevance: MRI often detects structural abnormalities that are not the actual source of a patient's pain, potentially leading to overdiagnosis and unnecessary procedures [83]. Therefore, MRI findings must always be correlated with the patient's clinical presentation.
FAQ: How can I improve the stability and reproducibility of biomarker discovery using machine learning?
Answer: A major challenge in ML-based biomarker discovery is overfitting, where a model performs well on the initial dataset but fails to generalize. To improve stability:
- Focus on Explainability: Use explainable AI (XAI) techniques to understand why a model makes a certain prediction. This helps ensure the model is learning biologically plausible mechanisms rather than noise in the data [85].
- Evaluate Stability: Assess the robustness of your discovered biomarker set by measuring its stability. This involves testing how similar the selected biomarkers are when the model is run on slightly different subsets of the data [86].
- Prioritize Integration: Consider integrating multiple feature selection methods, as this has shown great potential for producing more reliable and robust biomarker sets [86].
Quantitative Data Comparison
Table 1: Diagnostic Performance of Probe-to-Bone Test for Diabetic Foot Osteomyelitis
| Study Population | Sensitivity | Specificity | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) | Source |
|---|---|---|---|---|---|
| Outpatients, high prevalence (79.5%) | 98% | 78% | 95% | 91% | [24] |
| Cohort with bone culture-proven disease, prevalence 12% | 87% | 91% | 57% | 98% | [23] |
| In/outpatients, prevalence 60% | 66% | 84% | 87% | 62% | [82] |
Table 2: Performance of ML Biomarker Model vs. Blood Biomarker for Predicting Syndromal Conversion in Early Alzheimer's Disease
| Model Components | Area Under the Curve (AUC) - Cognitively Unimpaired | Area Under the Curve (AUC) - Mild Cognitive Impairment |
|---|---|---|
| Clinical features + Plasma p-tau181 + APOE ε4 genotype (Baseline) | 0.650 | 0.805 |
| Baseline + Plasma Neurofilament Light Chain (NfL) | 0.650 | 0.805 |
| Baseline + MRI-based ML Model (AD-RAI) | 0.832 | 0.853 |
Table 3: Key Research Reagent Solutions for Molecular Diagnostics in Diabetic Foot Research
| Reagent / Material | Function / Application | Example Context |
|---|---|---|
| Resveratrol | A natural polyphenolic compound used to investigate molecular mechanisms of wound healing; has anti-inflammatory and anti-oxidative stress properties. | Used in network pharmacology and experimental validation to identify therapeutic targets like CDA and ODC1 for diabetic foot ulcers (DFU) [51]. |
| Bone Biopsy Specimen | The gold standard for confirming osteomyelitis; used for histological analysis and culture. | Processed in buffered formalin for histology to diagnose osteomyelitis in diabetic foot studies [24]. |
| Swiss Target Prediction, TCMSP, PharmMapper | Online databases and servers used to predict the protein targets of bioactive compounds. | Employed to identify potential molecular targets of Resveratrol in a DFU study [51]. |
| Semmes-Weinstein Monofilament (5.07/10g) | A standardized tool for assessing peripheral neuropathy by testing pressure sensation on the foot. | Used to diagnose neuropathy in patients with diabetic foot ulcers in clinical studies [24]. |
| RNA-Seq / Microarray Data | High-throughput gene expression profiling technologies used for data-driven biomarker discovery. | Downloaded from the GEO database (e.g., GSE134431) to identify differentially expressed genes in DFU [51]. |
Experimental Protocols
Protocol 1: Validating the Probe-to-Bone Test with Bone Biopsy as Reference Standard
Objective: To assess the diagnostic accuracy of the probe-to-bone test for diabetic foot osteomyelitis against the gold standard of bone histology.
Methodology:
- Patient Enrollment: Recruit diabetic patients with a single foot ulcer below the ankle and clinical suspicion of infection (e.g., presence of purulent exudate, necrosis, or signs of inflammation) [24].
- Probe-to-Bone Test: After cleaning the ulcer with saline and sterile gauze, gently explore the wound base and sinus tracts with a blunt, sterile metal probe. The test is considered positive if a hard, gritty surface (assumed to be bone) is palpated [24].
- Reference Standard - Bone Biopsy: Patients with a positive PTB test or strong clinical suspicion undergo conservative surgical debridement of the affected bone. A representative bone specimen is collected and placed in 10% buffered formalin.
- Histopathological Analysis: The bone sample is processed and examined by a pathologist. The diagnostic criteria for osteomyelitis include the presence of inflammatory cell infiltrate (lymphocytes, plasma cells, neutrophils), bone necrosis, and reactive bone neoformation [24].
- Data Analysis: Calculate sensitivity, specificity, PPV, and NPV of the PTB test by comparing its results against the histological diagnosis.
Protocol 2: Developing a Machine Learning Biomarker Model from Gene Expression Data
Objective: To identify and validate a molecular biomarker signature for disease classification (e.g., Diabetic Foot Ulcer vs. control) using machine learning.
Methodology:
- Data Acquisition: Obtain transcriptomic data (e.g., RNA-Seq or microarray) from public repositories like the Gene Expression Omnibus (GEO). Ensure datasets include both case (e.g., DFU) and control samples [51].
- Data Preprocessing: Perform quality control, normalization, and batch effect correction (e.g., using the "sva" R package's "ComBat" function) on the merged datasets [51].
- Feature Selection (Biomarker Discovery):
- Differential Expression Analysis: Identify genes significantly differentially expressed between groups.
- Co-expression Analysis: Use methods like Weighted Gene Co-expression Network Analysis (WGCNA) to find modules of correlated genes associated with the disease trait.
- Machine Learning Feature Selection: Apply algorithms like Random Forest or Support Vector Machines (SVM) with embedded feature selection (e.g., F-score) to identify the most predictive genes. The intersection of genes from these methods can be used as candidate biomarkers [86] [51].
- Model Training and Validation: Train a classifier (e.g., SVM, Random Forest) using the selected biomarker genes. Evaluate the model's performance using metrics like AUC from a Receiver Operating Characteristic (ROC) curve on a held-out test set or via cross-validation [86].
- Experimental Validation: Confirm the expression of the identified biomarker genes in independent patient samples using techniques like immunohistochemistry [51].
Workflow and Pathway Visualizations
Diagram: Diagnostic Path Selection
Diagram: ML Biomarker Discovery Workflow
Technical Support Center
Troubleshooting Guides
Issue 1: Poor Nucleic Acid Yield from Diabetic Foot Ulcer Specimens
- Problem: Low quantity or poor quality of DNA/RNA extracted from tissue swabs or biopsies, leading to failed downstream molecular assays.
- Solution:
- Optimize Sample Collection: Ensure debridement of superficial debris before collecting a tissue sample from the wound base. Use sterile swabs with appropriate transport media.
- Enhance Lysis: For tough biofilms, extend mechanical homogenization time and incorporate proteinase K digestion for at least 60 minutes at 56°C.
- Inhibitant Removal: Use inhibitor removal columns or add bovine serum albumin (BSA) to PCR reactions to counteract common inhibitors in wound tissue.
- Prevention: Standardize sample collection protocols and train clinical staff on aseptic sampling techniques from viable wound tissue.
Issue 2: Inconsistent Results in AMR Gene Detection via Multiplex PCR
- Problem: Variable amplification efficiency between targets in a multiplex panel designed for common diabetic foot infection (DFI) pathogens.
- Solution:
- Primer Re-optimization: Redesign primers to have uniform melting temperatures (Tm ± 2°C) and minimize primer-dimer formation using design software.
- Balanced Master Mix: Titrate primer concentrations for each target and use a hot-start polymerase to improve specificity.
- Thermocycler Calibration: Verify temperature uniformity across the PCR block and use a thermal gradient to establish optimal annealing temperatures.
- Prevention: Validate all primer sets with control DNA from known DFI pathogens (e.g., Staphylococcus aureus, Pseudomonas aeruginosa) before patient sample testing.
Issue 3: High Contamination Rates in NGS Workflows
- Problem: Detection of contaminant microbial sequences in negative controls during next-generation sequencing for microbiome analysis.
- Solution:
- Physical Separation: Perform pre-PCR, PCR, and post-PCR steps in separate, dedicated rooms with unidirectional workflow.
- Decontamination: Treat work surfaces and equipment with DNA-degrading reagents (e.g., dilute bleach, UV irradiation) before and after use.
- Control Enhancement: Include multiple negative controls (extraction and PCR) throughout the process to identify the source of contamination.
- Prevention: Implement strict laboratory hygiene protocols and use dedicated pipettes with aerosol-resistant filter tips.
Frequently Asked Questions (FAQs)
Q1: What is the most cost-effective initial molecular test for characterizing polymicrobial infections in diabetic foot ulcers? A1: A targeted multiplex PCR panel for high-prevalence pathogens and common antimicrobial resistance (AMR) genes offers the best balance of cost, speed, and information. This approach avoids the higher expense of broad NGS panels while providing actionable results to guide initial antibiotic therapy more effectively than culture alone [87].
Q2: How can we justify the higher upfront cost of molecular diagnostics to hospital administrators in a resource-limited setting? A2: Frame the investment around cost-avoidance and improved patient outcomes. Modeling studies show that in high-AMR settings, a $100 molecular test can be cost-neutral by reducing inappropriate antibiotic use by up to 21%, shortening hospital stays by up to 5%, and improving bed turnover [87]. Presenting a cost-benefit analysis specific to your local AMR prevalence and hospitalization costs is critical.
Q3: Our culture turnaround time is 5-7 days. Will a molecular test still be beneficial? A3: Yes, but the impact is magnified with faster turnaround. The greatest clinical impact—including a potential 6% reduction in mortality—is achieved when molecular results are available within 24-48 hours to guide therapy adjustments [87]. Implement molecular tests alongside efforts to streamline sample transport and lab processing to minimize total reporting time.
Q4: We lack resources for whole-genome sequencing. What are robust alternatives for Ph-like ALL detection in DFU research? A4: Real-time quantitative PCR (qPCR)-based classifiers, such as the PHi-RACE protocol, provide a high-sensitivity, specific, and significantly lower-cost alternative to NGS for detecting key genetic fusions [88]. This can be complemented by FISH for characterizing kinase alterations, enabling targeted treatment planning without the need for extensive genomic infrastructure [88].
Experimental Protocols & Data
Table 1: Cost-Effectiveness Profile of Molecular Diagnostics for DFI
| Metric | Standard-of-Care (Culture + Phenotypic Testing) | Culture-Dependent Molecular Diagnostic | Data Source / Modeled Scenario |
|---|---|---|---|
| Average Turnaround Time | 3-5 days (can be 5-7 days) | 24-48 hours | [87] |
| Days on Inappropriate Therapy | Baseline | Reduction of up to 21% [IQR: 18.2-24.4%] | [87] (High AMR prevalence) |
| Mortality Impact | Baseline | Reduction of up to 6% [IQR: 0-12.1%] | [87] (High AMR, 100% coverage) |
| Hospital Stay Impact | Baseline | Reduction of up to 5% [IQR: 0.1-10.7%] | [87] |
| Cost per Test (Offset) | - | $109 (India) to $585 (South Africa) | [87] (Varies by setting and implementation) |
Table 2: Predominant Pathogens in Diabetic Foot Infections and Common Molecular Targets [89]
| Predominant Pathogens | Type | Key AMR Genes for Molecular Panels |
|---|---|---|
| Staphylococcus aureus | Gram-positive | mecA (methicillin resistance) |
| Enterococcus faecalis | Gram-positive | vanA, vanB (vancomycin resistance) |
| Escherichia coli | Gram-negative | blaCTX-M, blaNDM, blaKPC (ESBL, carbapenem resistance) |
| Klebsiella pneumoniae | Gram-negative | blaCTX-M, blaNDM, blaKPC (ESBL, carbapenem resistance) |
| Pseudomonas aeruginosa | Gram-negative | blaVIM, blaIMP (metallo-beta-lactamase) |
| Proteus mirabilis | Gram-negative | blaTEM, blaCTX-M (ESBL) |
Protocol: Cost-Efficient RNA Extraction and qPCR for Host-Response Profiling in DFU
Methodology:
- Sample Homogenization: Place 20-30 mg of debrided wound tissue in 600 µL of lysis buffer containing β-mercaptoethanol. Homogenize using a handheld rotor-stator homogenizer for 45-60 seconds on ice.
- RNA Extraction: Use a silica-membrane spin column kit. Include an on-column DNase I digestion step for 15 minutes to remove genomic DNA contamination.
- RNA Quantification: Measure RNA concentration using a spectrophotometer (e.g., NanoDrop). Accept samples with A260/A280 ratio between 1.8-2.1.
- cDNA Synthesis: Use 500 ng of total RNA in a 20 µL reverse transcription reaction with random hexamers and M-MuLV Reverse Transcriptase.
- qPCR Setup: Prepare reactions with 2 µL of cDNA, 200 nM of each primer, and SYBR Green master mix. Run in triplicate on a real-time PCR instrument.
- Data Analysis: Calculate relative gene expression using the 2^(-ΔΔCq) method, normalizing to stable housekeeping genes (e.g., GAPDH, β-actin).
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for DFU Molecular Diagnostics
| Reagent / Material | Function in the Context of DFU Research |
|---|---|
| Proteinase K | Digests proteins and inactivates nucleases during tissue lysis, crucial for breaking down tough biofilms in wound specimens. |
| DNase I & RNase Inhibitors | Protects the integrity of nucleic acids during extraction; DNase I is vital for removing host DNA when analyzing bacterial populations. |
| Silica-Membrane Spin Columns | selectively binds nucleic acids from lysates, allowing for purification and removal of PCR inhibitors common in wound tissue. |
| Multiplex PCR Master Mix | Contains optimized buffers and polymerase for simultaneous amplification of multiple pathogen or AMR gene targets from a single sample. |
| SYBR Green dye | Intercalates with double-stranded DNA PCR products, enabling real-time detection and quantification of amplified targets in qPCR assays. |
| Pathogen-Specific Primers & Probes | Designed to target conserved regions of genomes from common DFI pathogens (e.g., S. aureus, P. aeruginosa) or their AMR genes. |
Visual Workflows
Molecular Diagnostics Workflow for DFU
Cost-Effectiveness Factors for MDx
Technical Support Center: FAQs & Troubleshooting Guides
This technical support center addresses common challenges researchers face when utilizing [18F]FDG PET/CT and SPECT/CT in studies on the diabetic foot.
FAQ 1: How do I differentiate osteomyelitis from Charcot neuro-osteoarthropathy in a diabetic foot patient using molecular imaging?
This is a classic diagnostic challenge due to overlapping inflammatory features.
- The Problem: Both conditions can present with increased radiotracer uptake, leading to potential misdiagnosis and inappropriate treatment.
- The Solution: A multi-tracer, multi-modal approach is recommended.
- Preferred Method: Radiolabelled White Blood Cell (WBC) SPECT/CT is currently considered more accurate for this specific differentiation. True infection will show marked WBC accumulation, while a sterile Charcot foot typically will not [90].
- Alternative with [18F]FDG PET/CT: While [18F]FDG is sensitive, its specificity can be lower in this scenario. Carefully correlate PET findings with the anatomical information from the CT component. MRI is often the first-line advanced imaging modality, with WBC scintigraphy or [18F]FDG PET/CT used to resolve equivocal cases [90].
- Troubleshooting:
- Inconclusive WBC Scan: Ensure proper labeling and handling of leukocytes to maintain cell viability. A failed labeling procedure can lead to false-negative results.
- Intense [18F]FDG uptake in both conditions: Review the non-attenuation-corrected (NAC) PET images to avoid misinterpretation due to attenuation-correction artifacts. Always use hybrid imaging (SPECT/CT or PET/CT) for precise anatomical localization [91].
FAQ 2: What are the consensus interpretation criteria for diagnosing cardiovascular infection in a diabetic patient with a PET/CT scanner?
This applies to severe cases where infection may involve the heart, such as infective endocarditis.
- The Problem: Lack of standardized criteria can lead to inconsistent reporting of device-related or valvular infections.
- The Solution: Follow the multi-societal Expert Consensus Recommendations [92].
- Positive Findings: Focal or multifocal intense
18F-FDG uptake on prosthetic material (valves, devices) or diffuse, heterogeneous uptake in perivalvular areas. - Key Validation: The increased uptake must persist on non-attenuation-corrected (NAC) images to be considered a true-positive finding, thereby excluding attenuation-correction artifacts [92].
- Positive Findings: Focal or multifocal intense
- Troubleshooting:
- Diffuse, mild cardiac uptake: This is often a normal physiological variant and should not be reported as infection.
- High background noise on NAC images: Ensure the scanner is properly calibrated and that acquisition protocols use sufficient counts to maintain image quality on both AC and NAC reconstructions.
FAQ 3: How can I optimize my TB [18F]FDG PET/CT workflow for high patient throughput without compromising diagnostic quality?
Long-axial field-of-view (LAFOV) or Total-Body (TB) PET/CT scanners offer unique efficiency advantages.
- The Problem: Balancing the desire for low radiotracer activity or dynamic imaging with the need to scan a large number of patients.
- The Solution: Implement an optimized scanning strategy based on recent clinical research [93]. The table below summarizes theoretical patient throughput for an 8-hour working day under different injection regimens.
| Injection Activity Regimen | Activity per kg | Theoretical Throughput (8 hrs) | Clinical Validation (Patients) |
|---|---|---|---|
| Full-Activity | 3.70 MBq/kg | 60 patients | 60 patients |
| Half-Activity | 1.85 MBq/kg | 48 patients | 49 patients |
| 1/3-Activity | 1.11 MBq/kg | 43 patients | 48 patients |
| 1/10-Activity | 0.37 MBq/kg | 30 patients | 28 patients |
- Troubleshooting:
- Reduced throughput with low activity: If using low-activity protocols, expect a longer acquisition time per patient, which naturally reduces daily capacity. Plan your schedule accordingly [93].
- Managing a mixed-protocol day: For a fixed number of patients, strategically combining regimens (e.g., starting with full-activity and moving to lower-activity protocols) can minimize total radiotracer consumption [93].
FAQ 4: What are the common musculoskeletal and inflammatory pitfalls in diabetic foot PET/CT interpretation?
Increased [18F]FDG uptake is not specific to infection or malignancy.
- The Problem: Benign conditions like fractures, post-surgical changes, or neuropathic joints can show significant uptake, mimicking osteomyelitis or a soft-tissue infection [94].
- The Solution:
- Thorough Patient History: Always obtain a history of recent trauma, surgery, or presence of neuropathic osteoarthropathy [94].
- Correlate with CT Anatomy: Carefully inspect the CT images for correlative findings such as fracture lines, degenerative joint changes, or post-surgical metalwork that can cause uptake [94] [91].
- Troubleshooting:
- Uptake near a fracture: A linear pattern of uptake aligning with a fracture on CT is likely traumatic. A more irregular, destructive pattern with adjacent soft-tissue involvement suggests infection.
- Metal implant artifact: Be aware of falsely increased uptake due to attenuation-correction artifacts near metal implants. Always review NAC images to confirm true radiopharmaceutical accumulation [91].
Experimental Protocols for Diabetic Foot Research
Protocol 1: [18F]FDG PET/CT for Diagnosing Diabetic Foot Osteomyelitis (DFO)
This protocol is based on evidence-based guidance from the European Association of Nuclear Medicine (EANM) [90].
- 1. Patient Preparation:
- Fasting: Fast for at least 4-6 hours to reduce physiologic glucose levels and serum insulin to near-basal levels. Oral hydration with water is encouraged [95].
- Blood Glucose Monitoring: Check blood glucose level prior to [18F]FDG administration. Reschedule the study if the level is >150-200 mg/dL. If insulin is used to reduce levels, a delay in [18F]FDG injection is required [95].
- Patient Positioning: The patient should remain seated or recumbent during the uptake phase to minimize muscular uptake [95].
- 2. Radiopharmaceutical Administration:
- Inject 370-740 MBq (10-20 mCi) of [18F]FDG intravenously in a quiet environment.
- 3. Uptake Phase:
- Allow for a uptake period of 60-90 minutes. Encourage the patient to rest comfortably and avoid talking or chewing to limit physiological uptake in muscles and vocal cords.
- 4. Image Acquisition:
- Positioning: Position the patient supine with the feet secured in a neutral position. If possible, arms should be elevated over the head to reduce artifacts, though for dedicated foot imaging, arms-down may be acceptable.
- CT Scan: Perform a low-dose CT scan from at least the distal tibia through the entire foot for attenuation correction and anatomical localization. For detailed anatomical assessment, a diagnostic CT with intravenous contrast may be considered, depending on the clinical question and renal function.
- PET Scan: Acquire the PET data over the same region. For modern digital PET/CT systems, 1-2 minutes per bed position is often sufficient for the foot, though acquisition time may be adjusted based on the injected activity and scanner sensitivity.
- 5. Image Reconstruction and Analysis:
- Reconstruct images using iterative reconstruction with attenuation correction.
- Interpretation: Diagnose osteomyelitis based on locally increased [18F]FDG uptake that is focal and intense, clearly localized to bone on the fused PET/CT images, and not explained by other causes like trauma or surgery [90]. Use semi-quantitative analysis (SUVmax) with caution, as there is no universally accepted diagnostic threshold.
Protocol 2: Radiolabelled Leukocyte SPECT/CT for Complicated Diabetic Foot Infections
This protocol is indicated when [18F]FDG PET/CT is inconclusive or when differentiating infection from Charcot arthropathy is the primary goal [90].
- 1. Leukocyte Labeling:
- Withdraw 40-50 mL of the patient's blood under aseptic conditions.
- Label the isolated white blood cells with
99mTc-HMPAO or111In-Oxine following EANM guidelines for quality control [90].
- 2. Reinjection:
- Reinject the labelled leukocytes (185-370 MBq for
99mTc-HMPAO) slowly back into the patient.
- Reinject the labelled leukocytes (185-370 MBq for
- 3. Image Acquisition:
- Early Planar Imaging (Optional): Acquire planar images of the feet at 30-60 minutes post-injection to establish a baseline.
- Delayed SPECT/CT: Perform SPECT/CT imaging of the feet at 3-4 hours post-injection. The CT component should be a low-dose scan for attenuation correction and anatomical localization.
- 4. Image Analysis:
- Positive for Infection: Focal, increasing accumulation of labelled leukocytes over time at a site compatible with clinical suspicion.
- Negative for Infection: No abnormal accumulation or activity that decreases over time.
Data Summaries
Table 1: Diagnostic Performance of Advanced Imaging Modalities in Diabetic Foot Osteomyelitis
Data synthesized from EANM evidence-based guidance and supporting literature [96] [90].
| Imaging Modality | Typical Sensitivity | Typical Specificity | Key Strengths | Key Limitations |
|---|---|---|---|---|
| MRI | High | Moderate-High | Excellent anatomical detail; can assess for abscesses | Limited specificity in differentiating neuro-osteoarthropathy from infection; contraindicated for some implants |
| WBC SPECT/CT | High | High (Superior for OM vs. Charcot) | High specificity for infection | Labor-intensive, in-vitro handling of blood, not universally available |
| [18F]FDG PET/CT | High | Moderate | Rapid, high-resolution whole-body imaging; readily available | Lower specificity than WBC; uptake in sterile inflammation |
Table 2: Key Radiotracers for Infection Imaging in Diabetic Foot Research
Data synthesized from the search results [97] [92] [90].
| Research Reagent | Mechanism of Uptake | Primary Clinical/Research Application |
|---|---|---|
| [18F]FDG | Uptake in cells with high glucose metabolism (activated inflammatory cells, neutrophils) | Detecting infection/inflammation; staging and monitoring treatment response |
| 99mTc-HMPAO / 111In-Oxine Labelled Leukocytes | Active migration and chemotaxis of labelled white blood cells to site of infection | Gold standard for specific diagnosis of infection, especially for differentiating OM from Charcot foot |
| 18F-Sodium Fluoride (NaF) | Chemisorption to bone hydroxyapatite crystals, reflecting bone turnover and blood flow | Detecting bone formation and remodeling; less specific for infection |
Visualized Workflows and Pathways
Diagram 1: DFO Diagnostic Workflow
Diagram 2: Molecular Pathways of Common Tracers
Conclusion
The optimization of molecular diagnostic patterns for diabetic foot is rapidly evolving from a conceptual framework to a clinical reality. The integration of explainable machine learning models with robust biomarker panels offers a powerful, non-invasive avenue for accurately differentiating complex infections like osteomyelitis from soft tissue infections, demonstrating performance that rivals or surpasses traditional methods. The concurrent discovery of novel molecular targets such as SCUBE1 and RNF103-CHMP3 opens new frontiers for both diagnostic and therapeutic development. Future research must focus on large-scale, prospective validation of these tools and their seamless integration into multidisciplinary care pathways. The ultimate goal is a paradigm shift towards precision medicine, where molecular diagnostics enable earlier intervention, personalized treatment strategies, and a significant reduction in the high rates of amputations and mortality associated with diabetic foot complications.
References
- 1. Frontiers | Identification of biomarkers and potential drug targets in DFU ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1561179/full]
- 2. , Impaired Vasculature, and Diabetic ... Foot Ulcer Neuropathy Immune [https://www.intechopen.com/chapters/1163570]
- 3. The pathophysiology of diabetic : a narrative review foot [https://pubmed.ncbi.nlm.nih.gov/37797951/]
- 4. Machine learning-driven discovery of novel therapeutic targets in... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11562697/]
- 5. The pathophysiology of diabetic : a narrative review foot [https://www.e-jyms.org/journal/view.php?number=2810]
- 6. Frontiers | Diagnostic value and integrated threshold of ESR for... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1660465/full]
- 7. Osteomyelitis: Diagnosis and Treatment | AAFP [https://www.aafp.org/pubs/afp/issues/2021/1000/p395.html]
- 8. Osteomyelitis - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK532250/]
- 9. Immune escape of Staphylococcus aureus mediated by osteocyte... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171435/]
- 10. - Symptoms and causes - Mayo Clinic Osteomyelitis [https://www.mayoclinic.org/diseases-conditions/osteomyelitis/symptoms-causes/syc-20375913]
- 11. Frontiers | A comprehensive characterization of metabolic signatures—hypoxia, glycolysis, and lactylation—in non-healing diabetic foot ulcers [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1593390/full]
- 12. Frontiers | Mitochondrial metabolic regulation of macrophage... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1604320/full]
- 13. Are Deep Tissue Cultures a Reliable Alternative to Bone for... Biopsy [https://pubmed.ncbi.nlm.nih.gov/40218231/]
- 14. Using a BonE (BeBoP) to determine the causative agent in... BiOPsy [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05472-6]
- 15. bone biopsy [https://www.radiologyinfo.org/en/info/bonebiopsy]
- 16. Challenging the gold : the standard of limitations assays... molecular [https://pubmed.ncbi.nlm.nih.gov/38286614/]
- 17. The role of machine learning in advancing diabetic foot: a review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11089132/]
- 18. Frontiers | Construction and validation of a deep learning-based diagnostic model for segmentation and classification of diabetic foot [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1543192/full]
- 19. Artificial Intelligence and Machine Learning in Diabetic Foot Ulcer Care: Advances in Diagnosis, Treatment, Prognosis, and Novel Therapeutic Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321808/]
- 20. Nasal MRSA carriage is a risk factor for development of antibiotic... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10601299/]
- 21. : Why Isn’t it the ‘ Molecular ’? Diagnostics Gold Standard [https://clpmag.com/diagnostic-technologies/molecular-diagnostics/molecular-diagnostics-why-isnt-it-the-gold-standard/]
- 22. of Diagnostic to Detect Osteomyelitis in the... Accuracy Probe to Bone [https://pubmed.ncbi.nlm.nih.gov/27369321/]
- 23. Probe-to-bone test for diagnosing diabetic foot osteomyelitis: reliable or relic? - PubMed [https://pubmed.ncbi.nlm.nih.gov/17259493/]
- 24. Validating the Probe-to-Bone Test and Other Tests for Diagnosing Chronic Osteomyelitis in the Diabetic Foot - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2945149/]
- 25. Diagnostic Value of Erythrocyte Sedimentation Rate and C Reactive Protein in detecting Diabetic Foot Osteomyelitis; a Cross-sectional Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7587984/]
- 26. Machine learning-driven discovery of novel therapeutic targets in... [https://molmed.biomedcentral.com/articles/10.1186/s10020-024-00955-z]
- 27. The biology of SCUBE | Journal of Biomedical Science | Full Text [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-023-00925-3]
- 28. Protective Effect of SCUBE on Oxidative... | Research Square 1 [https://www.researchsquare.com/article/rs-468929/v1]
- 29. Machine learning combining external validation to explore the immunopathogenesis of diabetic foot ulcer and predict therapeutic drugs - PubMed [https://pubmed.ncbi.nlm.nih.gov/40749079/]
- 30. An analysis of gene expression profiles through machine learning uncovers the new diagnostic signature for diabetic foot ulcers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12234326/]
- 31. Explainable machine for differential diagnosis of diabetic foot... learning [https://link.springer.com/article/10.1186/s12911-025-03236-9]
- 32. Explaining multivariate molecular tests via Shapley values diagnostic [https://pubmed.ncbi.nlm.nih.gov/34238309/]
- 33. Explaining multivariate molecular tests via Shapley values diagnostic [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-021-01569-9]
- 34. Interpreting artificial intelligence models: a systematic review on the application of LIME and SHAP in Alzheimer’s disease detection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10997568/]
- 35. Interpretability part 3: opening the black box with LIME and SHAP - KDnuggets [https://www.kdnuggets.com/2019/12/interpretability-part-3-lime-shap.html]
- 36. How to Interpret Machine Learning Models with LIME and SHAP [https://svitla.com/blog/interpreting-machine-learning-models-lime-and-shap/]
- 37. machine learning for differential Explainable of diagnosis ... diabetic [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-025-03236-9]
- 38. A feature explainability-based deep learning technique for diabetic ... [https://pubmed.ncbi.nlm.nih.gov/40000748/]
- 39. UFOS-Net leverages small-scale feature fusion for diabetic foot ... ulcer [https://www.nature.com/articles/s41598-025-12442-4?error=cookies_not_supported&code=966df1b5-4cfd-431b-be0b-996a91698a48]
- 40. Enhancing Early Detection of Diabetic Foot Ulcers Using Deep Neural Networks [https://www.mdpi.com/2075-4418/15/16/1996]
- 41. system for Wagner ulcers - DR STEVEN... classification diabetic foot [https://stevenedwards.com.au/wagner-classification-system-for-diabetic-foot-ulcers/]
- 42. 's Wagner as a Tool for Treating Classification Ulcers... Diabetic Foot [https://pmc.ncbi.nlm.nih.gov/articles/PMC8861474/]
- 43. Translating Clinical Delineation of Diabetic Foot ... | SpringerLink Ulcers [https://link.springer.com/chapter/10.1007/978-3-031-80871-5_1]
- 44. An analysis of gene expression profiles through machine learning uncovers the new diagnostic signature for diabetic foot ulcers - PubMed [https://pubmed.ncbi.nlm.nih.gov/40630119/]
- 45. -driven exploration of Machine for atrial... learning therapeutic targets [https://pubmed.ncbi.nlm.nih.gov/41257259/]
- 46. Meta-Analysis Using Transcriptomics GEO Datasets [https://www.elucidata.io/blog/geo-datasets-for-transcriptomics-meta-analysis-in-research]
- 47. Identifying Therapeutic for Neurodegenerative Diseases Targets [https://bigomics.ch/blog/insights-into-neurodegenerative-diseases-using-transcriptomics-datasets/]
- 48. Imaging of Molecular Infections: New Tools for Old... Diabetic Foot [https://pubmed.ncbi.nlm.nih.gov/31795077/]
- 49. Statistical and machine methods for spatially resolved... learning [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-022-02653-7]
- 50. Gene Expression Omnibus - NCBI - NIH [https://www.ncbi.nlm.nih.gov/geo/]
- 51. Frontiers | Investigating the molecular mechanisms of resveratrol in... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1708426/full]
- 52. PCR Troubleshooting & Solutions | Boster Bio Guide [https://www.bosterbio.com/protocol-and-troubleshooting/pcr-troubleshooting]
- 53. Journal of Medical Internet Research - Diabetic Ulcer... Foot [https://www.jmir.org/2025/1/e69408]
- 54. Mastery Molecular Diagnostics [https://www.numberanalytics.com/blog/molecular-diagnostics-mastery-microbiology]
- 55. Evaluation of Machine Learning Models for Clinical ... Prediction [https://pmc.ncbi.nlm.nih.gov/articles/PMC9177058/]
- 56. Characterizing, Diagnosing and Managing the Risk of Error of ML & AI... [https://link.springer.com/chapter/10.1007/978-3-031-39355-6_13]
- 57. in Building Trust Machine Learning Predictions [https://www.linkedin.com/advice/0/dealing-client-skepticism-machine-learning-predictions-mktsf]
- 58. Global Trends in Diabetic Foot Research (2004–2023): A Bibliometric Study Based on the Scopus Database - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12026514/]
- 59. Frontiers | Inflammation, diabetic foot and related treatments [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1676621/full]
- 60. of Diabetic Foot Differential and Diagnosis ... Osteomyelitis Charcot [https://pmc.ncbi.nlm.nih.gov/articles/PMC11522243/]
- 61. Charcot Neuropathic Osteoarthropathy - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK470164/]
- 62. Foot: Clinical Clues, Charcot Strategies, and... | AAFP Diagnostic [https://www.aafp.org/pubs/afp/issues/2018/0501/p594.html]
- 63. Treatment of Charcot and Neuroarthropathy of the... osteomyelitis [https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-017-1818-4]
- 64. of Diabetic Foot Differential and Diagnosis ... Osteomyelitis Charcot [https://link.springer.com/article/10.1007/s10278-024-01067-0]
- 65. 5 Steps To Optimize Multimodal Pipelines [https://nano-gpt.com/blog/5-steps-to-optimize-multimodal-pipelines]
- 66. Multimodal Data Fusion - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/computer-science/multimodal-data-fusion]
- 67. Frontiers | Predicting the diabetic in the population of type... foot [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2024.1473659/full]
- 68. A Multi-Faceted Digital Health Solution for Monitoring and Managing... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11085305/]
- 69. Deep Learning for Diabetic Retinopathy Detection... | Research Square [https://www.researchsquare.com/article/rs-7196434/v1]
- 70. Inputs Into Development and Use of... Integrating Molecular Biomarker [https://pmc.ncbi.nlm.nih.gov/articles/PMC8560682/]
- 71. Receiver operating characteristic curve analysis in diagnostic accuracy... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10664195/]
- 72. Performance Metrics in Machine Learning [Complete Guide] - neptune.ai [https://neptune.ai/blog/performance-metrics-in-machine-learning-complete-guide]
- 73. Development and validation of an interpretable machine learning... [https://pubmed.ncbi.nlm.nih.gov/40069597/]
- 74. Reliability and Clinical of Machine Learning to Predict Stroke... Utility [https://www.j-stroke.org/journal/view.php?number=344]
- 75. Evaluation Metrics in Machine Learning - GeeksforGeeks [https://www.geeksforgeeks.org/machine-learning/metrics-for-machine-learning-model/]
- 76. In-depth mining of clinical data: the construction of clinical prediction... [https://atm.amegroups.org/article/view/29812/html]
- 77. 12 Important Model Evaluation Metrics for Machine Learning Everyone Should Know (Updated 2025) [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 78. Radiomics-based machine learning for glioma grade classification... [https://tcr.amegroups.org/article/view/107438/html]
- 79. Predicting the molecular subtypes of 2021 WHO grade 4 glioma by... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14529-7]
- 80. Frontiers | Integrating multimodal ultrasound imaging and machine... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1558880/full]
- 81. machine learning-derived Comparing -based and blood-based... MRI [https://pubmed.ncbi.nlm.nih.gov/37087687/]
- 82. of the Performance - probe - to in a population suspected of... bone test [https://pubmed.ncbi.nlm.nih.gov/23001730/]
- 83. Is my MRI accurate? Is it Reliable? - [https://caringmedical.com/prolotherapy-news/getting-accurate-mri/]
- 84. Is your MRI Report Accurate? The Scary Truth Behind MRI Report Errors | MDView [https://www.mdview.com/blog/mdview-news-articles-1/is-your-mri-report-accurate-the-scary-truth-behind-mri-report-errors-18]
- 85. The benefits and pitfalls of machine learning for biomarker discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10558383/]
- 86. Machine Learning Approaches for Biomarker Discovery Using Gene Expression Data - Bioinformatics - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK569564/]
- 87. Modeling the impact and cost of a culture-dependent molecular test... [https://pubmed.ncbi.nlm.nih.gov/40350685/]
- 88. Bridging the Gap: Cost - Effective Strategies for Detecting Ph-Like... [https://link.springer.com/article/10.1007/s40291-025-00775-9]
- 89. A systematic review of diabetic infections: pathogenesis... foot [https://pmc.ncbi.nlm.nih.gov/articles/PMC11333436/]
- 90. imaging of the Diagnostic : an EANM evidence-based... diabetic foot [https://link.springer.com/article/10.1007/s00259-024-06693-y]
- 91. Frontiers | F-18 FDG PET/CT Imaging in Normal Variants, Pitfalls ... [https://frontiersin.org/articles/10.3389/fnume.2021.826109/full]
- 92. - 18 / F and Radiolabeled Leukocyte FDG / PET Imaging for... CT SPECT CT [https://pubmed.ncbi.nlm.nih.gov/38466252/]
- 93. Total-body 18 - F / FDG : more choices to promote PET ... CT clinical [https://ejnmmires.springeropen.com/articles/10.1186/s13550-025-01290-y]
- 94. Frontiers | 18F-FDG PET/CT Imaging: Normal Variants, Pitfalls, and Artifacts Musculoskeletal, Infection, and Inflammation [https://www.frontiersin.org/journals/nuclear-medicine/articles/10.3389/fnume.2022.847810/full]
- 95. Procedure Guideline for Tumor Imaging with 18F-FDG PET/CT 1.0 | Journal of Nuclear Medicine [https://jnm.snmjournals.org/content/47/5/885]
- 96. - 18 and F / FDG for the PET of PET ... CT diagnosis diabetic foot [https://pmc.ncbi.nlm.nih.gov/articles/PMC3738276/]
- 97. Positron emission tomography - Wikipedia [https://en.wikipedia.org/wiki/Positron_emission_tomography]