Validating Transmission Clusters: Integrating Contact Tracing and Molecular Data for Epidemic Control
This article provides a comprehensive framework for validating infectious disease transmission clusters by synthesizing traditional contact tracing with advanced molecular epidemiology.
Validating Transmission Clusters: Integrating Contact Tracing and Molecular Data for Epidemic Control
Abstract
This article provides a comprehensive framework for validating infectious disease transmission clusters by synthesizing traditional contact tracing with advanced molecular epidemiology. Aimed at researchers and public health professionals, it explores foundational cluster definitions, methodological approaches for integration, strategies for optimizing real-world operations, and rigorous validation techniques. By examining evidence from COVID-19, HIV, and other pathogens, the content offers practical guidance for enhancing cluster detection accuracy, improving resource allocation, and strengthening outbreak response systems for future epidemic preparedness.
Defining Transmission Clusters: Concepts and Public Health Significance
Understanding the dynamics of infectious disease spread requires a precise grasp of key epidemiological concepts, from the fundamental definition of a "contact" to the complex thresholds that govern the emergence of transmission clusters. This guide provides a structured comparison of these core concepts, framed within the critical context of validating transmission chains through contact tracing research. For researchers, scientists, and drug development professionals, accurately defining and measuring these elements is not merely an academic exercise; it is essential for designing effective interventions, forecasting epidemic trajectories, and evaluating the success of public health programs. The following sections break down the terminology, methodologies, and quantitative thresholds that form the foundation of modern infectious disease epidemiology, with a specific focus on how contact tracing data can be validated through advanced techniques like phylogenetic analysis.
Core Definitions: From Contact to Cluster
Foundational Epidemiological Terms
- Contact: A contact is defined by the physical proximity and interaction with an infected person that presents a risk of disease transmission. Definitions often specify a duration of exposure (e.g., more than 15 minutes of close contact) and can include household members or sexual partners [1].
- Contact Tracing: The process of identifying, assessing, and managing individuals who have been exposed to an infected person to prevent onward transmission. It is a cornerstone public health strategy for breaking chains of transmission [1] [2].
- Case (or Index Case): An instance of a particular disease, injury, or other health condition that meets selected clinical criteria. The index case is the first case to come to the attention of health authorities [3].
- Transmission Cluster: An aggregation of cases of a disease in a circumscribed area during a particular period. The term does not inherently imply that the number of cases is more than expected, as the expected number is often not known [3].
- Epidemic Threshold: The critical value of the basic reproduction number (R₀) or other model parameters, above which epidemics are possible and below which epidemics cannot occur [4] [5]. It marks the transition between a disease dying out and becoming self-sustaining in a population.
Defining Contact Proximity and Its Implications
The definition of a "contact" is operational and can vary depending on the pathogen's mode of transmission. For respiratory diseases like COVID-19, it is commonly based on physical proximity and the duration of contact [1]. This often translates to being within 1-2 meters of an infected person for a cumulative period, typically 15 minutes or more. For sexually transmitted infections, the definition centers on sexual partnerships. The precision of this definition directly impacts the efficiency and effectiveness of contact tracing; an overly broad definition can overwhelm systems with low-risk contacts, while an overly narrow one can miss genuine transmission events [6] [2].
Quantitative Thresholds and Their Impact on Transmission Dynamics
The Basic Reproduction Number (R₀) and Epidemic Thresholds
The basic reproduction number, R₀, is a cornerstone concept, defined as the expected number of secondary infections from an initial infectious individual in a completely susceptible population [4]. The epidemic threshold is the critical value of R₀ (typically R₀=1) above which an epidemic is possible [4] [5]. However, in structured populations, this threshold is not absolute. In network models, a more relevant measure is often R*, the expected number of secondary infections from an individual infected early in an epidemic (but not the very first case), who is typically selected with probability proportional to their number of contacts [4].
Table 1: Key Thresholds in Epidemiological Models
| Concept | Definition | Epidemic Implication | Key Influencing Factors |
|---|---|---|---|
| Basic Reproduction Number (R₀) | Average number of secondary cases from one infected individual in a fully susceptible population [4]. | An epidemic is possible if R₀ > 1; the disease dies out if R₀ < 1 [4] [5]. | Transmission rate, recovery rate, contact patterns. |
| Epidemic Threshold (R*) | Critical value of R₀ or other parameters (e.g., transmissibility) marking the phase transition [4]. | Determines the potential for an outbreak to occur and become sustained. | Network structure, contact heterogeneity, disease dynamics [4]. |
| Cluster Threshold | The point at which a group of cases transitions from sporadic to a recognized transmission cluster. | Helps in outbreak detection and resource allocation for control measures. | Contact intensity, population susceptibility, pathogen transmissibility. |
The Role of Network Structure and Contact Dynamics
The structure of contact networks profoundly influences epidemic thresholds. In static network models, the threshold depends on the degree distribution. For uncorrelated annealed networks, the threshold for contagion transmissibility (λc = β/μ) is given by λc =
Experimental Protocols for Validating Transmission Clusters
Methodologies for Assessing Contact Tracing Precision
A novel genomic pipeline has been developed to assess the precision of contact tracing, defined as the proportion of suggested transmission events not contradicted by genomic analysis [6] [8].
Protocol Workflow:
- Case-Contact Pair Identification: Conduct interviews with confirmed index cases to identify their close contacts (case-contact pairs) during their infectious period [6] [2].
- Sample Collection and Sequencing: Collect biological samples from both index cases and their identified contacts. Perform whole-genome sequencing of the pathogen (e.g., SARS-CoV-2) from these samples [6].
- Phylogenetic Analysis: Construct a time-scaled phylogeny (evolutionary tree) using the genomic sequences from all collected samples [6] [8].
- Variant Identification: Classify the sequences by circulating variants (e.g., Omicron BA.1, BA.2) to ensure comparisons are made within the same lineage [8].
- Cluster Validation: Determine if the case-contact pairs identified through tracing cluster together within the phylogeny with high statistical support. Pairs that do not cluster are considered genomically invalidated [6].
- Precision Calculation: Calculate precision as the proportion of traced pairs that are not invalidated by the phylogenetic analysis [6].
Protocol for Evaluating Backward Contact Tracing
Backward contact tracing aims to identify the source of an index case's infection (the parent case) and others infected by the same source (sibling cases) [2].
Experimental Protocol:
- Study Cohort Definition: Define a population cohort for observation, such as a university student body [2].
- Extended Tracing Window: For each index case, extend the contact tracing window backward in time (e.g., to 7 days before symptom onset or diagnosis) instead of the standard 2 days [2].
- Contact Identification and Management: Identify close contacts from this extended window. Refer these "backward-traced" contacts for testing and/or quarantine [2].
- Data Collection: Record the outcome (positive or negative test result) for all contacts, categorizing them as from the standard window or the extended window [2].
- Efficiency Analysis: Calculate the positivity rate (PR) for both groups. Compare the PR of the backward-traced group to a control group (e.g., symptomatic individuals from the general population) to assess efficiency. Also, track metrics like the number of tests per case found and the time from exposure to identification [2].
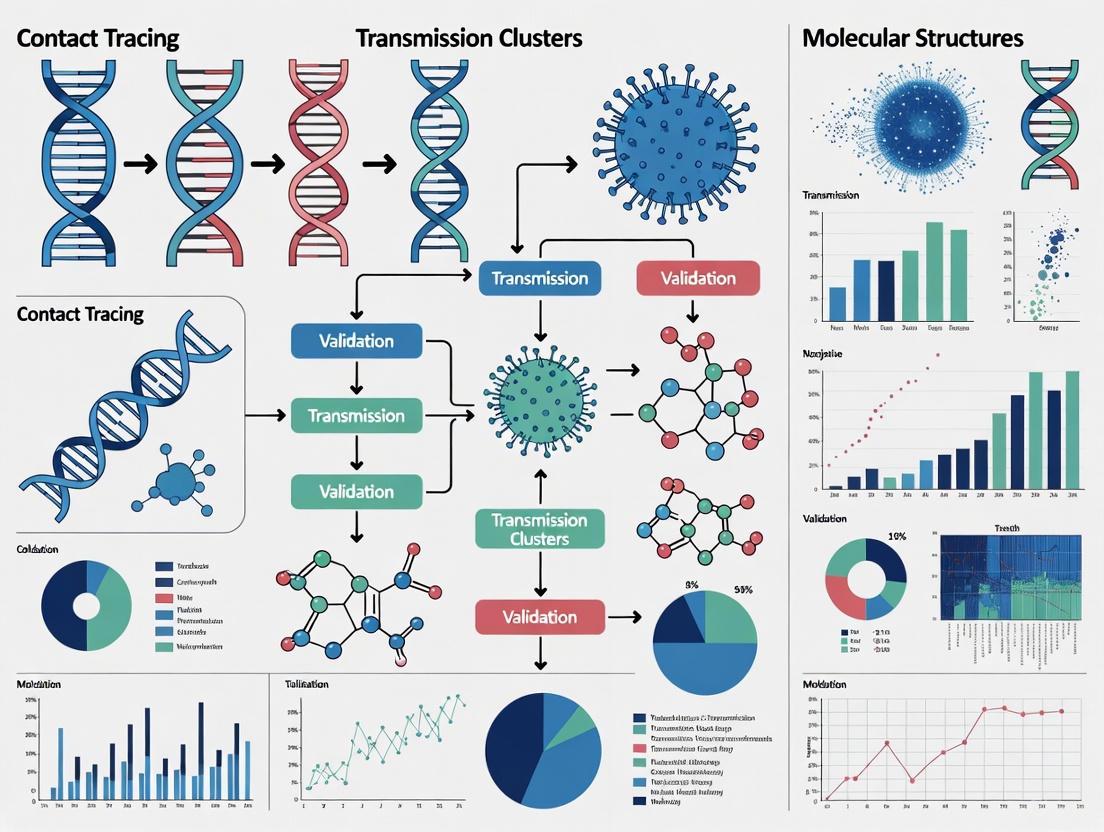
Figure 1: Workflow for Phylogenetic Validation of Contact Tracing Precision
Comparative Effectiveness of Contact Tracing Strategies
Contact tracing is not a monolithic intervention. Its effectiveness varies significantly based on the tracing method used, the context of the outbreak, and the resources available. The following table and analysis compare the performance of different approaches.
Table 2: Comparison of Contact Tracing Methods and Their Documented Effectiveness
| Tracing Method | Definition / Protocol | Context / Scenario | Documented Effectiveness | Key Experimental Findings |
|---|---|---|---|---|
| Forward Tracing | Identifies contacts of a known index case exposed during the standard contagious period (e.g., 2 days before onset) [9] [2]. | Low case-ascertainment, testing contacts [9]. | Reduced transmission by 12% [9]. | Found to be the least effective method in several comparative scenarios [9]. |
| Extended Tracing | Extends the contact tracing window further back in time (e.g., 16 days before isolation) to find the source of infection [9]. | Low case-ascertainment, quarantine of contacts [9]. | Reduced transmission by 50% [9]. | More effective than forward tracing but less than cluster methods; higher cost in one study [9]. |
| Cluster Tracing | Combines forward tracing with cluster identification, focusing on groups of cases and their shared exposures [9]. | Low case-ascertainment, quarantine of contacts [9]. | Reduced transmission by 62% [9]. | Most effective method in multiple scenarios, sufficient to bring the reproduction number close to unity [9]. |
| Backward Tracing | Aims to identify the infector of the index case (parent case) and other individuals infected by the same source (sibling cases) [2]. | Real-world cohort study in a student population [2]. | Identified 42% more cases as direct contacts of an index case [2]. | Positivity rate among backward-traced contacts was similar to forward-traced contacts and higher than a symptomatic control group [2]. |
| Bidirectional & Secondary Tracing | Combines forward and backward tracing. Secondary tracing involves tracing the contacts of contacts [10]. | Modelling studies and systematic reviews [10]. | Highly effective in modelling studies [10]. | Mathematical modelling identifies it as a highly effective policy for averting cases [10]. |
Synthesis of Comparative Data
The data reveals that cluster tracing consistently demonstrates high effectiveness, particularly in scenarios with quarantine of contacts, where it can reduce transmission by over 60% and bring the reproduction number close to 1 [9]. Backward contact tracing receives strong empirical support, with one large cohort study showing it can identify 42% more cases than standard forward tracing alone [2]. This efficiency is attributed to its ability to find "sibling" cases from a common source, which is crucial for containing pathogens with superspreading potential.
The overall effectiveness of any contact tracing operation is heavily dependent on the implementation context. Operations are most effective when implemented with high case-ascertainment rates and quarantine of contacts, which can stop transmission early and make operations more manageable and less costly [9]. Furthermore, hybrid manual and digital contact tracing with high app adoption is identified as a highly effective policy, especially when combined with effective isolation and social distancing [10].
Table 3: Key Research Reagent Solutions for Transmission Cluster Studies
| Tool / Resource | Category | Primary Function in Research |
|---|---|---|
| Whole-Genome Sequencer | Laboratory Equipment | Determines the complete DNA/RNA sequence of the pathogen from clinical samples for phylogenetic analysis [6] [8]. |
| Phylogenetic Analysis Software | Computational Tool | Builds evolutionary trees from genomic sequences to infer transmission relationships and validate clusters [6] [8]. |
| Contact Tracing Data System | Data Management | A database for storing, managing, and analyzing interview-based contact data, case details, and outcomes [9] [2]. |
| Statistical Computing Package | Analytical Software | Performs statistical analyses, calculates key metrics (e.g., positivity rates, serial intervals), and generates visualizations [2]. |
| Diagnostic Assays | Laboratory Reagent | Confirms active infection in index cases and traced contacts (e.g., RT-qPCR tests for SARS-CoV-2) [2]. |
Figure 2: Core Resources for Contact Tracing Research
In the domain of infectious disease control, cluster validation is the critical process of confirming that identified groups of cases, or "clusters," represent genuine transmission events linked by a common source or chain of infection. This process moves beyond simple case clustering to provide epidemiological confirmation that connections between cases are biologically plausible and not merely coincidental. Within contact tracing research, validation transforms raw data from case interviews into reliable intelligence about transmission patterns. The imperative for rigorous cluster validation stems from the resource-intensive nature of public health interventions; without validation, health agencies risk misdirecting limited resources toward false leads while missing genuine outbreaks. As countries worldwide have implemented diverse contact tracing approaches during the COVID-19 pandemic, the critical importance of validating identified clusters has emerged as a consistent theme in outbreak management [11] [1].
The fundamental challenge in cluster investigation lies in distinguishing true transmission chains from coincidental case aggregations. This challenge is particularly acute for highly transmissible pathogens like SARS-CoV-2, where asymptomatic transmission and overdispersion (superspreading events) can create complex transmission patterns that defy conventional investigation methods [12] [13]. Cluster validation provides the methodological framework to address this challenge, incorporating approaches from genomic epidemiology, bioinformatics, and statistical modeling to confirm suspected outbreaks. As public health systems evolve toward more sophisticated surveillance capabilities, cluster validation represents the essential quality control mechanism that ensures epidemiological insights translate into effective disease control.
Comparative Effectiveness of Cluster Investigation Methods
Quantitative Outcomes of Different Tracing Strategies
The effectiveness of cluster-based approaches compared to standard contact tracing methods varies significantly across diseases and operational contexts. The following table summarizes key performance metrics from recent studies comparing these methodologies:
Table 1: Comparative Performance of Cluster vs. Standard Contact Tracing
| Tracing Method | Disease Context | Contacts Identified per Case | Key Performance Metrics | Study Reference |
|---|---|---|---|---|
| Genotyped Cluster Investigation | Tuberculosis (Florida, 2009-2023) | 4.82 contacts/case | 81.5% contacts evaluated; 20.4% LTBI diagnosis rate; 92.9% treatment initiation [14] | |
| Standard Contact Investigation | Tuberculosis (Florida, 2009-2023) | 3.79 contacts/case | 85.5% contacts evaluated; 21.5% LTBI diagnosis rate; 95.9% treatment initiation [14] | |
| Cluster Tracing Method | COVID-19 (Modelling, Singapore) | N/A | 62% transmission reduction (low ascertainment, quarantine); most effective of three methods [9] | |
| Exposure Cluster Surveillance | COVID-19 (England, 2020-2021) | N/A | 25% genetically validated; 81% not otherwise recorded; 1-day earlier detection [13] |
Cluster investigations demonstrate a clear advantage in contact identification volume, particularly for tuberculosis control, where genotyped clusters identified approximately 27% more contacts per case than standard investigations [14]. This expanded reach enables public health systems to cast a wider net around potential transmission chains. However, the quality of subsequent engagement and care progression shows nuanced differences, with standard contact investigations achieving slightly higher rates of contact evaluation and treatment initiation in the TB care cascade [14]. This suggests that while cluster methods excel at case finding, maintaining the quality of downstream interventions remains essential.
For respiratory pathogens like SARS-CoV-2, modeling studies indicate that cluster tracing methods outperform both forward tracing (identifying future potential cases) and extended tracing (covering longer periods before case isolation), particularly in scenarios with low case ascertainment. When combined with quarantine of contacts, cluster tracing reduced transmission by 62%—enough to bring the reproduction number close to unity—and proved to be the least costly approach among alternatives [9]. This demonstrates the pivotal role of cluster-focused strategies in pandemic control when resources are constrained.
Validation Rates Across Settings and Methodologies
The accuracy of cluster detection varies substantially across different environmental contexts and methodological approaches. The following table compares validation rates from multiple studies:
Table 2: Cluster Validation Rates Across Methodologies and Settings
| Validation Methodology | Setting/Context | Cluster Validation Rate | Key Influencing Factors | Study Reference |
|---|---|---|---|---|
| Genomic Phylogenetics | University setting (Belgium, Omicron waves) | 34.6% precision | Combined phylogenetic + SNP analysis; serial interval refinement [8] | |
| Exposure Data Matching | Community settings (England, 2020-2021) | 25% genetic validity | Workplace and educational settings showed highest validity [13] | |
| Digital Contact Tracing | National rollout (Norway, 2020) | 80% technological efficacy | Varying detection by phone type (Android: 74%, iOS: 54%) [15] | |
| Bayesian Case Linking | Synthetic network simulation | Varying by parameters | Household size, population size, algorithm parameters [12] |
The setting of potential transmission events significantly influences validation likelihood. In England's enhanced contact tracing programme, exposure clusters occurring in workplaces (aOR = 5.10, 95% CI 4.23–6.17) and educational settings (aOR = 3.72, 95% CI 3.08–4.49) demonstrated the strongest association with genetic validity in multivariable analysis [13]. This highlights the epidemiological importance of these environments for SARS-CoV-2 transmission and suggests that setting-based risk assessment can prioritize investigation resources.
The validation methodology itself substantially impacts measured accuracy. Genomic approaches provide high-resolution validation but may be resource-intensive for routine application. Belgium's phylogenetic validation of a university contact tracing program achieved a precision rate of 34.6%, meaning just over one-third of epidemiologically-identified case-contact pairs were not contradicted by genomic evidence [8]. This underscores both the value of genomic validation for refining transmission understanding and the potential for over-estimation of linkage in purely epidemiological assessments.
Experimental Protocols for Cluster Validation
Genomic Validation Pipeline
Genomic methods provide the gold standard for cluster validation by establishing biological relatedness between cases. The following workflow outlines a phylogenetically-validated assessment approach:
Figure 1: Genomic Validation Pipeline for Transmission Clusters
This pipeline was implemented in a study of SARS-CoV-2 transmission at Belgium's largest university during Omicron BA.1 and BA.2 waves. Researchers analyzed 459 case-contact pairs identified through contact tracing, then used combined phylogenetic and single nucleotide polymorphism (SNP) analysis to determine whether pairs infected with the same variant clustered together within a time-scaled phylogeny [8]. This approach calculated precision as the proportion of transmission events suggested by contact tracing that were not contradicted by genomic analysis, yielding a validation rate of 34.6% [8]. The genomic data enabled more accurate estimation of epidemiological parameters like serial intervals, with refined estimates showing smaller standard deviation than those derived from all case-contact pairs [8].
Automated Cluster Detection Algorithm
For rapid assessment during outbreaks, automated computational approaches can provide preliminary cluster validation:
Figure 2: Automated Cluster Detection Workflow
This algorithm utilizes a Bayesian approach to probabilistically link cases using either the serial interval or generation interval [12]. The method was developed and tested using synthetic social networks created with the epinet R package, representing geography, households, and primary spoken language [12]. Outbreak simulation employed an SEIR (Susceptible-Exposed-Infected-Removed) model with parameters including a contact rate (β) of 0.2 (representing exponentially distributed 5 days of infection), gamma-distributed latency period (average 0.14 days), and recovery period (average 5.44 days) [12]. The "connectprobablecases" function from the autotracer package returns transmission pairs with the highest posterior likelihood of being true transmission events, with unlikely pairs truncated using a default threshold of 30 days between recorded cases [12]. Performance is assessed by comparing the actual versus detected number of clusters and average cluster size using root mean squared error (RMSE) [12].
Exposure Cluster Surveillance System
England's Enhanced Contact Tracing Programme implemented a systematic approach to cluster surveillance based on case exposure data:
Figure 3: Exposure Cluster Surveillance System
This system analyzed data from cases occurring between October 2020 and September 2021, extracting exposure information from the national contact tracing system [13]. The methodology identified exposure clusters algorithmically by matching two or more cases attending the same event, using postcode and event category matching within a 7-day rolling window [13]. Genetic validity was defined as exposure clusters with two or more cases from different households with identical viral sequences [13]. The system identified 269,470 exposure clusters, with 25% (3,306/13,008) of eligible clusters proving genetically valid [13]. Crucially, 81% (2,684/3,306) of these validated clusters were not recorded in the national incident management system and were identified on average one day earlier than officially recorded incidents [13], demonstrating the added value of systematic exposure cluster surveillance.
Technical Implementation and Research Toolkit
Essential Research Reagents and Computational Tools
The experimental protocols described require specialized reagents, software tools, and analytical frameworks. The following table details key solutions for implementing cluster validation methodologies:
Table 3: Research Reagent Solutions for Cluster Validation
| Tool/Reagent Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Genomic Sequencing | Whole genome sequencing; Spoligotyping; MIRU-VNTR; wgMLST | Genotype characterization; Cluster definition | Tuberculosis [14]; SARS-CoV-2 [8] [13] |
| Bioinformatic Packages | epinet R package; autotracer package; outbreaker2 R package; igraph package | Network simulation; Bayesian case linking; Transmission tree analysis | Synthetic network modeling [12]; Clustering algorithms [12] |
| Cluster Validation Indices | SLEDgeH (Support, Length, Exclusivity, Difference) | Categorical data validation; Semantic cluster description | Non-metric cluster validation [16] |
| Digital Tracing Frameworks | Exposure Notification System (ENS); Smittestopp; Bluetooth Low Energy (BLE) | Proximity detection; Contact event logging | Digital contact tracing [15] |
| Statistical Platforms | R version 4.1.3; Bayesian probabilistic models; Multivariable logistic regression | Statistical analysis; Model parameterization; Uncertainty quantification | Performance assessment [12] [13] |
The bioinformatic packages enable critical analytical functions. The epinet R package facilitates synthetic social network generation and outbreak simulation, while the autotracer package implements Bayesian approaches for probabilistic case linking [12]. The outbreaker2 R package utilizes Bayesian methods to probabilistically link cases using serial intervals or generation intervals, and the igraph package implements greedy clustering algorithms for transmission tree analysis [12]. For genomic validation, phylogenetic analysis tools combined with SNP calling pipelines provide the biological resolution needed to confirm or refute epidemiological links [8] [14].
For categorical data validation, recent advances in cluster validation indices like SLEDgeH (an enhanced version of the SLEDge framework) provide specialized approaches for evaluating clustering quality in categorical data common in epidemiological records [16]. Unlike conventional distance-based indices, SLEDgeH uses optimized weighting of semantic descriptors derived from frequent patterns, combining four indicators—Support, Length, Exclusivity, and Difference—through weight optimization to improve cluster discrimination [16]. This approach is particularly valuable for patient record data where traditional distance metrics may fail to capture meaningful relationships.
Technological Efficacy in Digital Tracing Systems
Digital contact tracing systems present unique validation challenges and opportunities. Analysis of Norway's Smittestopp app rollout revealed a technological tracing efficacy of 80%, with significant variation between mobile operating systems: Android devices detected other Android devices with 74% probability, while iPhone-iPhone detection was 54% [15]. The overall effectiveness followed a quadratic relationship with app uptake, with the detection probability for different device pairings being: pii = 0.54 (iPhone detects iPhone), pai = 0.53 (Android detects iPhone), pia = 0.53 (iOS detects Android), and paa = 0.74 (Android detects Android) [15]. This technological efficacy represents the upper bound of performance for digital tracing systems, which also depends on population uptake and adherence.
The research indicated that at least 11.0% of discovered close contacts could not have been identified by manual contact tracing alone [15], highlighting the added value of digital approaches. The study also suggested that digital contact tracing can flag individuals with excessive contacts, potentially helping to contain superspreading-related outbreaks [15]. While the overall effectiveness of digital tracing depends strongly on app uptake, significant impact can be achieved at moderate uptake levels (40%) when combined with fast and effective case isolation [15].
Cluster validation represents more than a technical exercise in epidemiological methodology—it establishes the fundamental unit of analysis for effective outbreak control. As the comparative evidence demonstrates, validated clusters provide the precision necessary to target interventions toward genuine transmission events rather than coincidental case aggregations. The experimental protocols detailed—from genomic pipelines to automated detection algorithms—provide a methodological toolkit for transforming raw case data into confirmed transmission chains.
The future of cluster validation lies in integrated approaches that combine the complementary strengths of genomic confirmation, algorithmic pattern recognition, and digital exposure assessment. As validation methodologies become more sophisticated and accessible, they will increasingly form the backbone of evidence-based outbreak response. For researchers and public health professionals, investing in robust cluster validation capabilities represents not merely a technical specialization but a foundational commitment to precision public health—where limited resources are deployed with maximum impact based on rigorously validated transmission intelligence.
Cluster typology analysis is a foundational tool in infectious disease epidemiology, enabling researchers to dissect the heterogeneous nature of disease transmission. In the context of SARS-CoV-2, the identification and characterization of distinct cluster types—particularly household, occupational, and super-spreading events—has proven critical for developing targeted interventions. This guide provides a systematic comparison of these transmission settings, drawing upon contact tracing data and cluster analysis methodologies to validate their unique characteristics. By objectively examining the performance of different intervention strategies across settings and presenting supporting experimental data, this analysis aims to equip researchers and public health professionals with evidence-based frameworks for outbreak management.
The substantial variation in transmission dynamics across different environments underscores the importance of moving beyond population-wide averages to setting-specific understandings of spread. Cluster analysis, an unsupervised learning algorithm that groups data points based on their similarities without pre-defined categories [17], provides the methodological foundation for this approach. When applied to COVID-19 outbreaks, this technique allows for the identification of inherent patterns in transmission data, revealing critical differences in transmission potential, overdispersion, and intervention effectiveness across settings [18] [19].
Comparative Analysis of Cluster Typologies
Quantitative analysis of transmission clusters reveals significant differences in transmission potential and heterogeneity across settings. The following comparison synthesizes data from multiple studies to provide a comprehensive overview of these typologies.
Table 1: Transmission Parameters by Cluster Typology
| Transmission Setting | Effective Reproduction Number (R) | Dispersion Parameter (k) | Superspreading Threshold Probability | Proportion of Cases Causing 80% of Spread |
|---|---|---|---|---|
| Overall Population | 0.56 (0.50-0.64) [18] | 0.22 (0.19-0.26) [18] | 1.75% (1.57-1.99%) [18] | 13.14% (11.55-14.87%) [18] |
| Household | 0.14 (0.11-0.17) [18] | 0.14 (0.10-0.21) [18] | 0.07% (0.06-0.08%) [18] | 30% responsible for 80% of spread [19] |
| Healthcare Facilities | 0.19 (0.08-0.41) [18] | 0.004 (0.002-0.006) [18] | 0.67% (0.31-1.21%) [18] | 15-20% responsible for 80% of spread [19] |
| Restaurants/Social Dining | Not reported | 0.1-0.5 [19] | Not reported | 25% responsible for 80% of spread [19] |
| Close-Social Indoor Activities | 7.1 [19] | ~0.3 [19] | Not reported | ~10% responsible for 80% of spread [19] |
| Retail & Leisure | 0.58 (0-1.17) [19] | 0.05 (0.01-0.09) [19] | Not reported | 5% responsible for 80% of spread [19] |
| Office Work | 0.38 (0.26-0.50) [19] | ~0.3 [19] | 0.32% (0.21-0.60%) [18] | 15-20% responsible for 80% of spread [19] |
Table 2: Cluster Distribution and Size by Setting (Hong Kong Data, 2020-2021)
| Transmission Setting | Number of Identified Clusters | Percentage of All Clusters | Maximum Observed Cluster Size | Asymptomatic Proportion |
|---|---|---|---|---|
| Household | 3,318 | 87.1% | Small to medium | 12-39% [19] |
| Office Work | 365 | 9.6% | ≤10 cases | 12-39% [19] |
| Restaurants | 282 | 7.4% | Medium | 12-39% [19] |
| Manual Labour Work | 253 | 6.6% | ~50 cases | 12-39% [19] |
| Retail & Leisure | 108 | 2.8% | ~50 cases | 12-39% [19] |
| Nosocomial | 80 | 2.1% | Medium | 12-39% [19] |
| Close-Social Indoor | 61 | 1.6% | 395 cases | 12-39% [19] |
| Residential Care Homes | 59 | 1.5% | ~50 cases | 12-39% [19] |
Key Observations from Comparative Data
- Household transmission demonstrates the lowest reproduction number but accounts for the vast majority of clusters (87.1%), representing the most common but least explosive transmission setting [19].
- Close-social indoor settings (including bars, social gatherings, and religious events) show the highest mean number of new infections per cluster (CZ = 7.1) and have been associated with the largest documented clusters (up to 395 cases) [19].
- Occupational settings display variable transmission patterns, with office work showing lower transmission potential (CZ = 0.38) compared to manual labor settings (CZ = 1.0-1.5) [19].
- Retail and healthcare environments exhibit extreme transmission heterogeneity (k = 0.05 and 0.004, respectively), indicating high superspreading potential where a very small percentage of cases (5% and 0.44%, respectively) generate the majority of infections [18] [19].
Experimental Protocols for Cluster Validation
Contact Tracing Methodologies
Contact tracing serves as the primary experimental protocol for validating transmission clusters and establishing links between cases. Different methodological approaches yield varying levels of effectiveness:
Table 3: Contact Tracing Method Effectiveness Under Different Scenarios
| Tracing Method | Low Case-Ascertainment with Testing | Low Case-Ascertainment with Quarantine | High Case-Ascertainment with Testing | High Case-Ascertainment with Quarantine |
|---|---|---|---|---|
| Forward Tracing (2 days before isolation) | 12% transmission reduction | 46% transmission reduction | 20% transmission reduction | Equally effective (All methods bring R<1) |
| Extended Tracing (16 days before isolation) | Intermediate effectiveness | 50% transmission reduction (Highest cost) | Intermediate effectiveness | Equally effective (All methods bring R<1) |
| Cluster Tracing (Forward + cluster identification) | 22% transmission reduction (Most effective) | 62% transmission reduction (Most effective, least costly) | 26% transmission reduction (Most effective) | Equally effective (All methods bring R<1) |
Protocol Details:
- Case Identification and Interview: Laboratory-confirmed cases are interviewed to identify their contacts and exposure settings. In the Hong Kong protocol, cases were classified based on detailed contact histories [19] [20].
- Contact Categorization: Contacts are classified by setting (household, workplace, social, etc.) and exposure risk level.
- Transmission Pair Construction: Infector-infectee pairs are established based on epidemiological links, with verification through symptom onset dates and exposure windows [18].
- Cluster Definition: Clusters are defined as ≥2 linked cases with evidence of local transmission, distinguished from sporadic cases or imported infection chains [20].
- Data Analysis: The number of secondary cases generated by each infector is fitted to a negative binomial distribution to estimate the effective reproduction number (R) and dispersion parameter (k) using Markov chain Monte Carlo (MCMC) methods [18].
Cluster Analysis and Statistical Modeling
The validation of transmission clusters relies on sophisticated statistical approaches that account for the overdispersed nature of SARS-CoV-2 transmission:
Cluster Validation Workflow
Negative Binomial Modeling Protocol:
- Data Preparation: Clean and structure contact tracing data into infector-infectee pairs, excluding cases with incomplete information [18] [21].
- Model Selection: Select the negative binomial distribution to model the number of secondary cases, as it accommodates overdispersion better than the Poisson distribution [18] [19].
- Parameter Estimation: Use maximum likelihood estimation or Bayesian methods (e.g., MCMC) to estimate the effective reproduction number (R, the mean of the distribution) and dispersion parameter (k, measuring heterogeneity) [18].
- Setting-specific Analysis: Conduct subgroup analyses for different transmission settings (household, workplace, social) to estimate setting-specific R and k values [18] [19].
- Superspreading Threshold Calculation: Define superspreading events (SSEs) using the 99th percentile of the Poisson distribution with the estimated R as the threshold [18].
- Validation: Assess model fit using goodness-of-fit tests and compare observed versus expected cluster size distributions [19].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Tools for Transmission Cluster Analysis
| Tool/Resource | Function | Application Example |
|---|---|---|
| Contact Tracing Data | Provides line-list of cases with epidemiological links | Construct transmission chains and identify settings [18] [19] |
| Negative Binomial Model | Statistical framework for overdispersed count data | Estimate reproduction number (R) and dispersion parameter (k) [18] [20] |
| Cluster Analysis Algorithms | Unsupervised learning to identify natural groupings | Segment transmission events into typologies without pre-defined categories [17] |
| Markov Chain Monte Carlo (MCMC) | Bayesian parameter estimation method | Generate posterior distributions for R and k with credible intervals [18] |
| Generation Interval Data | Time between successive cases in a transmission chain | Understand transmission dynamics and timing of interventions [19] |
The validation of transmission clusters through contact tracing research reveals fundamental insights into the heterogeneous nature of SARS-CoV-2 transmission. Household settings, while numerically dominant, demonstrate relatively limited transmission potential compared to occupational and social environments. Conversely, superspreading events, particularly in close-social indoor settings and environments with high interaction densities, drive a disproportionate share of transmission despite representing a small minority of clusters.
This comparative analysis underscores the critical importance of setting-specific interventions. Rather than uniform approaches, effective outbreak control requires tailored strategies that address the unique transmission dynamics of each typology. For researchers and public health professionals, the methodological frameworks presented here provide actionable tools for identifying, analyzing, and responding to diverse transmission scenarios in ongoing and future infectious disease outbreaks.
In infectious disease epidemiology, the serial interval and reproduction number serve as fundamental metrics for quantifying transmission dynamics. The serial interval represents the time between symptom onset in a primary case and a secondary case, providing crucial information about the speed of disease spread [22]. The effective reproduction number (Rt) indicates the average number of new infections generated by each infected individual at a specific time within a population. Accurate estimation of these parameters is essential for designing effective public health interventions, forecasting epidemic trajectories, and assessing the impact of control measures.
The validation of transmission clusters represents a critical challenge in epidemiological research, particularly during the COVID-19 pandemic. Traditional methods relying on contact tracing data alone face significant limitations, including incomplete sampling, recall bias, and resource constraints that vary substantially across jurisdictions [23]. Emerging approaches that integrate genomic epidemiology with traditional methods offer promising avenues for overcoming these limitations, providing higher resolution estimates of transmission parameters and strengthening the validation of inferred transmission clusters [22] [13].
Comparative Analysis of Estimation Methods
Traditional Contact Tracing Approaches
Traditional methods for estimating serial intervals and reproduction numbers predominantly rely on epidemiological investigations and contact tracing data. These approaches typically involve identifying infector-infectee pairs through detailed interviews and then calculating the time difference between their symptom onsets. A systematic review and meta-analysis of COVID-19 serial intervals found a pooled estimate of approximately 5.19-5.40 days based on data from the early pandemic phase [24]. These estimates, however, demonstrated considerable heterogeneity across studies, reflecting methodological differences and varying transmission contexts.
The effectiveness of traditional contact tracing varies significantly based on implementation. A modelling study comparing contact tracing methods found that cluster tracing (combining forward tracing with cluster identification) reduced transmission by up to 62% when implemented with quarantine of contacts, outperforming both forward and extended tracing methods [9]. However, the same study highlighted that effectiveness was highly dependent on case-ascertainment rates and compliance levels, with performance dropping substantially under low ascertainment scenarios.
Table 1: Comparison of Serial Interval Estimates from COVID-19 Studies
| Study Reference | Study Region | Time Period | Sample Size | Mean Serial Interval (Days) | 95% Confidence Interval |
|---|---|---|---|---|---|
| Nishiura et al. [24] | Multiple | Up to Feb 2020 | 28 | 4.7 | 3.7 - 6.0 |
| Du et al. [24] | China | Jan-Feb 2020 | 468 | 3.96 | 3.53 - 4.39 |
| Li et al. [24] | Wuhan | Up to Jan 2020 | 6 | 7.5 | 4.1 - 10.9 |
| Ki [24] | Korea | Up to Jan 2020 | 7 | 6.3 | 4.1 - 8.5 |
| Zhang et al. [24] | China | Jan-Feb 2020 | 35 | 5.1 | 1.3 - 11.6 |
| Zhao et al. [24] | Hong Kong | Jan-Feb 2020 | 21 | 4.4 | 2.9 - 6.7 |
| Ganyani et al. [24] | Singapore | Jan-Feb 2020 | 27 | 5.2 | 3.6 - 7.6 |
Genomic Epidemiology Framework
Genomic epidemiology offers an alternative framework for estimating serial intervals without requiring direct knowledge of transmission pairs, instead using virus sequences to infer who infected whom [22]. This approach constructs "transmission clouds" of plausible infector-infectee pairs based on genomic distance and symptom onset timing, then samples plausible transmission networks to estimate serial interval distributions while accounting for incomplete sampling through a mixture model.
This method demonstrated that cluster-specific serial intervals can vary estimates of the effective reproduction number by a factor of 2-3, highlighting the importance of context-specific parameter estimation [22]. The approach also revealed systematic differences in transmission dynamics across settings, with shorter serial intervals observed in schools and meat processing plants compared to healthcare facilities, suggesting different transmission patterns or ascertainment biases in these environments [22].
Table 2: Performance Comparison of Estimation Methods
| Method Characteristic | Traditional Contact Tracing | Genomic Epidemiology Framework |
|---|---|---|
| Data Requirements | Detailed exposure histories from contact tracing | Viral sequences and symptom onset times |
| Sampling Assumptions | Often assumes complete sampling of transmission pairs | Explicitly accounts for incomplete sampling through mixture model |
| Key Advantages | Direct observation of transmission pairs; Established methodology | Does not require resource-intensive contact tracing; Provides high-resolution, cluster-specific estimates |
| Key Limitations | Resource-intensive; Privacy concerns; Vulnerable to recall bias | Requires sequencing infrastructure and expertise; Computational complexity |
| Contextual Flexibility | Limited by quality of contact tracing data | Can be applied across various transmission settings and sampling scenarios |
| Validation Approaches | Comparison with known transmission pairs; Epidemiological plausibility | Genomic validation; Simulation studies; Comparison with contact tracing data |
Experimental Protocols and Methodologies
Genomic Estimation of Serial Intervals
The genomic epidemiology framework for serial interval estimation involves a multi-step process that integrates virological, epidemiological, and statistical approaches [22]:
Sequence Data Processing and Cluster Identification: Whole-genome SARS-CoV-2 sequences are obtained from cases and processed through quality control measures. Cases are grouped into transmission clusters based on genomic similarity and epidemiological links, with clusters defined as groups of cases with minimal genomic differences and plausible epidemiological connections.
Transmission Cloud Construction: For each cluster, researchers create a "transmission cloud" containing all plausible transmission pairs that meet predetermined criteria for genomic distance and temporal relationship between symptom onset times. This step acknowledges uncertainty in direct transmission links while incorporating biological constraints on plausible transmission pairs.
Network Sampling and Parameter Estimation: From the transmission cloud, multiple plausible transmission networks are sampled, with each infectee assigned an infector with probability inversely proportional to their genomic and symptom onset time distance. For each sampled network, a mixture model is fitted to estimate the serial interval distribution parameters, accounting for both direct transmission and transmission through unsampled intermediate cases. Finally, estimates are combined across all sampled networks to generate cluster-specific serial interval distributions.
Enhanced Contact Tracing for Cluster Detection
England's Enhanced Contact Tracing (ECT) programme implemented a systematic approach to cluster detection that combined exposure data from routine contact tracing with genomic validation [13]. The methodology involved:
Exposure Data Collection: During routine contact tracing for COVID-19, cases were interviewed about their exposures during the pre-symptomatic period (3-7 days before symptom onset). Data included locations visited, nature of activities, and timing of exposures.
Algorithmic Cluster Identification: Exposure clusters were identified by algorithmically matching two or more cases reporting attendance at the same event or location, using postcode matching and event categorization within a 7-day rolling window. This systematic approach allowed for detection of potential transmission events that might be missed through conventional forward contact tracing alone.
Genomic Validation: The genetic validity of exposure clusters was assessed by examining whether clusters contained two or more cases from different households with identical viral sequences, providing molecular evidence for shared transmission events. This validation step confirmed that approximately 25% of algorithmically identified exposure clusters represented genuine transmission events [13].
Risk Assessment and Public Health Action: Validated clusters underwent risk assessment by local public health teams to inform targeted interventions. Multivariable analysis identified that exposure clusters occurring in workplaces (aOR = 5.10) and educational settings (aOR = 3.72) were most strongly associated with genetic validity, guiding resource allocation for cluster investigation and management [13].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Transmission Cluster Studies
| Research Reagent / Tool | Primary Function | Application Context |
|---|---|---|
| Whole-genome Sequencing Platforms | Generation of complete viral genetic sequences | Genomic cluster identification; Mutation tracking; Transmission link validation [22] [13] |
| Phylogenetic Analysis Software | Reconstruction of evolutionary relationships between viral sequences | Inference of transmission chains; Identification of cryptic transmission; Estimation of evolutionary rates [22] |
| Contact Tracing Data Systems | Structured collection and management of exposure and contact information | Identification of potential transmission pairs; Exposure cluster detection; Epidemiological linkage assessment [9] [13] |
| Statistical Mixture Models | Estimation of parameters accounting for multiple transmission scenarios | Serial interval estimation with unsampled cases; Correction for incomplete sampling; Uncertainty quantification [22] |
| Network Analysis Algorithms | Mining relationships between transmission clusters | Identification of superspreading events; Cascade propagation analysis; Intervention targeting [25] |
| Genomic Distance Metrics | Quantification of genetic differences between viral isolates | Determination of plausible transmission pairs; Cluster definition; Outbreak boundary delineation [22] [13] |
Validation of Transmission Clusters
The integration of multiple data streams and methodologies significantly enhances the validation of transmission clusters. Research demonstrates that genomic validation serves as a robust approach for confirming epidemiologically-identified clusters, with studies reporting that approximately 25% of exposure clusters identified through enhanced contact tracing showed genetic evidence of shared transmission events [13]. This integration of epidemiological and genomic data provides a more comprehensive understanding of transmission dynamics than either approach could deliver independently.
Cluster characteristics significantly influence validation outcomes. Analyses reveal that workplace and educational settings show stronger associations with genetically valid clusters compared to other environments, highlighting the importance of context in transmission cluster validation [13]. Additionally, the size of exposure clusters and the timing of case detection serve as important predictors of validation success, enabling more efficient prioritization of public health resources.
Methodological innovations continue to advance cluster validation capabilities. The development of algorithms for mining relationships between transmission clusters enables the identification of superspreading events and cascade propagation patterns across multiple linked clusters [25]. These approaches facilitate a more comprehensive understanding of outbreak dynamics beyond individual clusters, revealing patterns of spread across communities and informing targeted intervention strategies.
The field of disease cluster analysis has undergone a profound transformation, evolving from simple descriptive maps to sophisticated computational algorithms that identify outbreaks with increasing speed and precision. Spatial epidemiology, now a cornerstone of public health, was famously exemplified by John Snow's 1854 cholera map, which visually identified a contaminated water pump on Broad Street in London as the outbreak source [26]. For more than a century, the geographical distribution of disease was primarily analyzed using thematic maps with darker colors indicating higher case concentrations—an approach easily misled by visual misclassification and the omission of critical temporal factors [26]. The integration of geographic information systems (GIS) has since enabled a more nuanced understanding of the relationships among agent, host, and environment [26].
In recent decades, this evolution has accelerated with the adoption of temporal clustering algorithms, phylogenetic methods, and mathematical modeling, fundamentally enhancing our ability to detect and interpret infectious disease transmission clusters. This progression mirrors a broader shift in public health surveillance from reactive documentation to proactive intervention, where the primary goal is the early detection of aberrant case patterns to trigger timely public health responses [26]. This guide objectively compares the performance and methodologies of key clustering approaches that have shaped the modern landscape of disease surveillance, with a particular focus on their validation within contact tracing research frameworks.
Comparative Analysis of Clustering Methodologies
The table below summarizes the core characteristics, strengths, and limitations of the major classes of cluster analysis methods used in disease surveillance.
Table 1: Comparative Overview of Disease Cluster Analysis Methodologies
| Method Category | Representative Tools | Core Clustering Principle | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| Temporal Aberration Detection | Historical Limit, CUSUM, Moving Average [26] | Identifies case counts exceeding a statistical baseline or threshold [26] | Simple implementation; provides early warning signals; some variants (e.g., CUSUM) require little historical data [26] | Baseline can be skewed by past large outbreaks; may produce over-alerts; requires verification [26] |
| Genetic Distance-Based | HIV-TRACE, MicrobeTrace [27] [28] | Groups sequences with pairwise genetic distances below a user-defined threshold [27] | Computationally fast; generalizable across pathogens; does not assume a transmission tree [27] | Dependent on an arbitrary distance threshold; no penalty for unrealistic numbers of introductions [27] |
| Phylogenetic Heuristic | ClusterTracker [27] | Uses ancestral trait inference and heuristics to assign cluster membership from a phylogeny [27] | Designed for scalability on large datasets (e.g., millions of sequences) [27] | No correction for biased sampling; clusters constrained to a single region [27] |
| Phylogenetic Model-Based (Maximum Likelihood) | Nextstrain's augur [27] | Models trait migration (e.g., location) as a continuous-time Markov process along a time-scaled phylogeny [27] | Represents a balance between simplistic and complex models; widely used for live outbreak monitoring [27] | Region does not influence tree reconstruction; complicated to correct for sampling bias [27] |
| Phylogenetic Model-Based (Bayesian) | BEAST [27] | Co-infers phylogeny and migration history in a Bayesian framework, allowing traits to influence tree structure [27] | Accounts for phylogenetic uncertainty; considered highly robust for scientific inference [27] | Computationally intensive; does not scale well with many samples or regions [27] |
| Threshold-Free Phylogenetic | Phydelity [29] | Identifies groups of sequences more closely related than the ensemble distribution without a fixed distance threshold [29] | Eliminates need for arbitrary cutpoints; identifies monophyletic and paraphyletic clusters; high purity in simulations [29] | Interpretation limited to fully connected transmission networks without directionality [29] |
Performance Benchmarking and Empirical Concordance
The theoretical differences between methods lead to measurable variations in their outputs. Empirical comparisons are essential for understanding these discrepancies and selecting the right tool for a given public health scenario.
Concordance Across HIV-1 Molecular Cluster Methods
A study comparing 12 analytical approaches for identifying HIV-1 transmission clusters revealed significant variability in outcomes depending on the method and parameters used [28]. The study evaluated clustering based on topological support (a measure of confidence in tree branches) and genetic distance thresholds (e.g., 0.015 substitutions/site for strict criteria) [28].
Table 2: Performance of Selected Methods on an HIV-1 Dataset (n=1886 sequences)
| Method | Proportion of Sequences Clustered (Strict Thresholds) | Proportion of Sequences Clustered (Relaxed Thresholds) | Number of Clusters (Strict Thresholds) | Number of Clusters (Relaxed Thresholds) | Mean Concordance with Other Methods (Strict Thresholds) |
|---|---|---|---|---|---|
| HIV-TRACE | 36% | Not Specified | 172 | Not Specified | 65% |
| RAxML | 22% | 38% | 156 | 223 | 88% |
| IQ-Tree (ultrafast) | 30% | 54% | 187 | 234 | 86% |
| PhyML aLRT | 24% | 54% | 167 | 234 | 86% |
| MEGA | 22% | 38% | 156 | 223 | 82% |
Key findings from this benchmarking include:
- Distance threshold was the dominant factor influencing clustering proportions, more so than topological support [28].
- Model-based methods (e.g., RAxML, IQ-Tree) generally clustered fewer sequences than the distance-based HIV-TRACE under strict thresholds, but often more under relaxed thresholds [28].
- Concordance between methods was variable. While some method-pairs agreed on over 90% of clustered sequence pairs, others, like MEGA and HIV-TRACE, shared as few as 17% of pairs under strict thresholds [28].
- The authors concluded that no single method is universally superior, and the choice of analytical approach should be tailored to the specific public health goal and epidemic context [28].
Performance on Bacterial and Viral Outbreak Case Studies
A separate comparison of four methods on real-world bacterial (Klebsiella aerogenes) and viral (SARS-CoV-2) outbreaks further highlighted methodological differences [27]. All methods (HIV-TRACE, ClusterTracker, Nextstrain's augur, and BEAST) successfully identified a singular, monophyletic transmission cluster for the 15-case K. aerogenes hospital outbreak [27]. However, the HIV-TRACE cluster was the least specific, including the 15 outbreak strains plus one unlinked hospital strain and 14 other context strains from the same region [27]. In contrast, the phylogenetic methods defined the cluster more strictly as the monophyletic clade of the 15 outbreak cases, demonstrating higher specificity [27].
This illustrates a key trade-off: distance-based methods like HIV-TRACE can be highly sensitive but may lack specificity, while phylogenetic methods can provide a more epidemiologically plausible cluster boundary but may require more computational expertise.
Experimental Protocols for Cluster Validation
Protocol for Phylogenetic Cluster Analysis with Phydelity
Phydelity is a threshold-free algorithm designed to identify putative transmission clusters from a phylogenetic tree without relying on arbitrary genetic distance thresholds [29].
Detailed Methodology:
- Input Preparation: The input is a phylogenetic tree, typically inferred from pathogen genome sequences.
- Calculate Maximal Patristic Distance Limit (MPL):
- For each sequence tip in the tree, compute the patristic distances to its closest k-neighbouring tips (including itself).
- Autoscale the k parameter to find the largest value that still yields a distribution of low divergence among neighbours.
- The MPL is calculated as:
MPL = μ¯ + σ, whereμ¯is the median of this kth core distance distribution andσis a robust estimator of its scale [29].
- Evaluate Putative Clusters: Every internal node
iin the tree is considered a putative cluster. Its within-cluster diversity, measured by the mean pairwise patristic distance (μi) of its descendant tips, is evaluated. Ifμiis less than the MPL, the node is considered for clustering [29]. - Dissociate Distant Sequences: The algorithm dissociates (prunes) distantly related subtrees from putative clusters to ensure all internal and tip nodes within a cluster have a mean pairwise nodal distance ≤ MPL [29].
- Integer Linear Programming (ILP) Optimization: An ILP model is run to find the clustering configuration that assigns sequences to the fewest number of clusters possible while satisfying the relatedness criteria. This favors the designation of larger, well-supported clusters [29].
- Output: The final output is a set of putative transmission clusters, interpreted as fully connected networks of likely transmission pairs [29].
Protocol for Benchmarking Multiple Clustering Tools
The comparative study on HIV-1 clusters provides a robust framework for benchmarking method performance and concordance [28].
Detailed Methodology:
- Dataset Curation: A set of 1886 HIV-1 pol sequences from Rhode Island (2004–2018) was compiled.
- Method Selection and Parameterization: Twelve different analytical approaches were selected, including model-based phylogenetic methods (e.g., RAxML, IQ-Tree) and the distance-based HIV-TRACE. Each method was run across a matrix of 49 different parameter combinations, varying topological support (0.00 to 0.95) and genetic distance thresholds (0.000 to 0.045 substitutions/site) [28].
- Define Cluster Criteria: Two specific scenarios were defined for focused comparison:
- Strict Thresholds: Topological support ≥ 0.95 and genetic distance ≤ 0.015 substitutions/site.
- Relaxed Thresholds: Topological support between 0.80–0.95 and genetic distance between 0.030–0.045 substitutions/site [28].
- Performance Metrics Calculation:
- Clustering Proportion: The proportion of the total 1886 sequences assigned to any cluster was calculated for each method and threshold.
- Concordance Analysis: For each pair of methods, the concordance was measured in three ways:
- Sequence Pair Concordance: The proportion of pairs of sequences that were grouped together in a cluster by both methods.
- Identical Cluster Concordance: The proportion of clusters identified by one method that were exactly identical to clusters found by another method.
- Non-clustered Sequence Concordance: The proportion of sequences not assigned to any cluster that were agreed upon by both methods [28].
- Robustness Testing: To ensure robustness, key steps like phylogenetic reconstruction with RAxML were repeated 100 times with different random seeds to measure variance in the resulting cluster proportions [28].
Integration with Contact Tracing for Cluster Validation
Contact tracing (CT) serves as a critical ground-truthing mechanism for validating molecularly inferred transmission clusters. It is defined as the identification, evaluation, and management of people exposed to a disease to prevent subsequent transmission [1]. The effectiveness of CT as a public health intervention creates a feedback loop, where clustering algorithms identify potential outbreaks, and contact tracing investigations confirm or refute these putative transmission links [26] [1].
Mathematical models, particularly during the COVID-19 pandemic, have explicitly parameterized CT to evaluate its impact on transmission dynamics. A systematic review found that 49.1% of such models were compartmental models (often placing traced contacts in a separate compartment), 34% were agent-based models, and 9.4% used branching processes [30]. These models demonstrate that when integrated with quarantine, CT acts at both individual and population levels, leading to earlier diagnosis and a decrease in the effective reproduction number (Re) of an outbreak [30]. This modeled impact aligns with the goal of phylogenetic cluster detection, which is to find groups of sequences linked by direct transmission or shared risk factors that represent active transmission chains [31] [29].
However, a significant challenge is that standard phylogenetic clustering methods assume homogeneous transmission dynamics, while real-world transmission clusters exhibit dynamic behavior over time [31]. A study evaluating phylogeny-based tools on simulated dynamic clusters found their combined sensitivity and specificity to be low, indicating a pressing need for novel methods that can reliably detect individuals linked by changing transmission dynamics [31].
The Scientist's Toolkit: Essential Research Reagents & Solutions
The following table details key computational tools and data resources essential for conducting cluster analysis in disease surveillance.
Table 3: Key Research Reagents and Computational Solutions for Cluster Analysis
| Tool/Resource Name | Category/Type | Primary Function in Analysis |
|---|---|---|
| HIV-TRACE [27] [28] | Software Tool (Distance-Based) | Detects transmission clusters by grouping sequences with genetic distances below a user-defined threshold; often applied to HIV but generalizable. |
| Phydelity [29] | Software Tool (Phylogenetic) | Identifies putative transmission clusters from a phylogenetic tree without requiring an arbitrary genetic distance threshold. |
| Nextstrain (augur) [27] | Bioinformatics Pipeline | Builds time-scaled phylogenies, infers ancestral traits, and tracks pathogen spread in real-time for public health surveillance. |
| BEAST [27] | Software Package (Bayesian Evolutionary Analysis) | Co-infers phylogenetic trees, evolutionary rates, and ancestral history in a Bayesian framework, accounting for uncertainty. |
| ClusterTracker [27] | Software Tool (Phylogenetic Heuristic) | Identifies clusters corresponding to introduction events on very large phylogenies (e.g., millions of SARS-CoV-2 sequences). |
| Context Genomes [27] | Reference Data | A set of pathogen sequences from general circulation, used as a background for comparison to determine if cases are more closely related to each other than to circulating strains. |
| Simulated Epidemic Datasets [29] [28] | Benchmarking Data | Computer-generated outbreaks with known transmission history, used to validate and benchmark the performance of clustering algorithms. |
Logical Workflow for Cluster Analysis and Validation
The following diagram illustrates the integrated workflow of data processing, cluster analysis, and validation that is central to modern disease surveillance.
Diagram 1: Integrated workflow for transmission cluster analysis and validation, showing how molecular data and contact tracing interact.
The evolution of cluster analysis in disease surveillance reveals a clear trajectory from simple spatial and temporal methods toward integrated, phylogenetically-informed frameworks. The empirical data shows that no single clustering algorithm is universally superior; each carries distinct strengths and limitations that make it suitable for different public health scenarios [28]. Distance-based methods like HIV-TRACE offer speed and simplicity, while model-based phylogenetic tools like BEAST provide statistical robustness at a computational cost. Threshold-free algorithms like Phydelity represent a significant advance in reducing subjective parameter choices [29].
A critical finding from recent research is the low concordance between different clustering methods and their current inability to fully capture the dynamic nature of transmission clusters [31] [28]. This underscores the necessity of using contact tracing as a validation scaffold to ground-truth computationally derived clusters [1]. The future of cluster analysis lies in the development of more dynamic phylogenetic methods and the tighter integration of molecular data with traditional epidemiological fieldwork. This synergy will be essential for transforming cluster detection from a descriptive exercise into a predictive, intervention-driven science capable of disrupting transmission chains in real-time.
Integrating Methodologies: Contact Tracing and Molecular Cluster Analysis
Contact tracing is a cornerstone public health intervention for breaking chains of transmission during infectious disease outbreaks. While digital tools have expanded tracing capabilities, traditional methods remain fundamental to epidemic response. This guide provides a systematic comparison of three traditional contact tracing methodologies—forward, backward, and cluster tracing—focusing on their operational mechanisms, effectiveness metrics, and implementation protocols. The analysis is situated within the broader research context of validating transmission clusters, a critical process for verifying epidemiological linkages identified through contact tracing activities. Understanding the comparative performance of these approaches provides researchers and public health professionals with evidence-based guidance for selecting context-appropriate strategies during outbreak responses.
Conceptual Frameworks and Definitions
Forward contact tracing, the most widely implemented method, identifies and manages individuals potentially infected by a known index case. This approach aims to interrupt onward transmission by identifying "child cases" (persons infected by the index case) [32] [2]. Operational protocols typically define the exposure window based on the pathogen's infectious period; for COVID-19, this commonly included contacts exposed from 2 days before symptom onset or diagnosis until case isolation [9] [2].
Backward contact tracing (also called bidirectional when combined with forward tracing) identifies the source of infection and individuals potentially infected by the same source. This method aims to identify "parent cases" (the infector of the index case) and "sibling cases" (others infected by the same parent case) [32] [2]. This approach is particularly valuable for pathogens exhibiting superspreading dynamics, as it efficiently uncovers transmission clusters [33] [2].
Cluster tracing integrates forward tracing with systematic cluster identification and investigation. This method focuses on detecting and containing transmission events involving multiple cases linked to specific settings or events [9] [11]. Rather than solely tracking individual transmission chains, cluster tracing employs analytical techniques to identify epidemiological linkages across cases, enabling targeted interventions in high-transmission settings [11].
The diagram below illustrates the conceptual framework and logical relationships between these three contact tracing methods within an outbreak investigation context.
Figure 1: Conceptual Framework of Contact Tracing Methodologies. This diagram illustrates the operational workflows and logical relationships between forward, backward, and cluster tracing methods in outbreak investigation.
Comparative Effectiveness Analysis
The effectiveness of contact tracing methods varies significantly based on operational context, including case ascertainment rates, contact management strategies, and resource availability. The following tables summarize quantitative performance data from modeling studies and empirical evaluations.
Table 1: Comparative Effectiveness of Tracing Methods Under Different COVID-19 Scenarios (Modelling Data)
| Tracing Method | Low Case-Ascertainment with Testing | Low Case-Ascertainment with Quarantine | High Case-Ascertainment with Testing | High Case-Ascertainment with Quarantine |
|---|---|---|---|---|
| Forward Tracing | 12% transmission reduction | 46% transmission reduction | 20% transmission reduction | Equally effective (All methods bring Reff <1) |
| Extended/Backward Tracing | 17% transmission reduction | 50% transmission reduction | 23% transmission reduction | Equally effective (All methods bring Reff <1) |
| Cluster Tracing | 22% transmission reduction | 62% transmission reduction | 26% transmission reduction | Equally effective (All methods bring Reff <1) |
| Provider Costs (per infection prevented) | US$2,944-$5,227 | Below US$4,000 | US$1,873-$3,165 | Below US$800 |
Source: Adapted from [9]
Table 2: Empirical Performance Metrics from Contact Tracing Implementation
| Performance Metric | Forward Tracing | Backward/Bidirectional Tracing | Cluster Tracing |
|---|---|---|---|
| Additional Cases Identified | Baseline | 42% more cases than forward alone [2] | Highly variable based on setting |
| Optimal Tracing Window | 2 days before symptom onset | 6-7 days before symptom onset [33] [2] | Event-based investigation |
| Impact on Effective Reproduction Number (Reff) | Moderate reduction | 85-275% improvement over forward tracing [33] | Largest reduction in high-cluster scenarios [9] |
| Resource Efficiency | Higher testing/quarantine requirements | Fewer tests and shorter quarantine per identified case [2] | Highly efficient when clusters are correctly identified |
| Precision (Phylogenetic Validation) | Not directly assessed | 34.6% precision in identified transmission pairs [8] | Not directly assessed |
Contextual Factors Influencing Effectiveness
The comparative performance of tracing methods depends heavily on several contextual factors. Case ascertainment rates significantly impact effectiveness; under high ascertainment with quarantine, all methods can bring the reproduction number below unity, stopping transmission early [9]. Pathogen characteristics also influence method selection; backward tracing proves particularly valuable for pathogens with superspreading potential, as identifying source cases and events can efficiently break multiple transmission chains simultaneously [33] [2]. Operational resources determine feasibility; while bidirectional tracing with an extended window shows superior effectiveness, it demands greater investigative capacity and rapid response capabilities [9] [33].
Experimental Protocols and Validation Methodologies
Transmission Network Modeling Protocol
Objective: To quantitatively compare the effectiveness of forward, backward, and cluster tracing methods under varied epidemic conditions [9].
Methodology Overview:
- Model Structure: Develop a stochastic transmission network model incorporating population contact structure and disease characteristics.
- Intervention Arms: Simulate three tracing approaches: forward tracing (2 days before case isolation), extended tracing (16 days before isolation), and cluster tracing (combining forward tracing with cluster identification).
- Scenario Analysis: Construct combinations of operational scenarios: (1) low vs. high case-ascertainment rates, and (2) testing vs. quarantine of contacts.
- Outcome Measures: Quantify impact on disease transmission (reproduction number, infection rates) and resource utilization (cost per infection prevented).
Implementation Details:
- Case isolation occurs after diagnosis, preventing further transmission.
- Contacts are identified, notified, and managed according to scenario specifications (testing or quarantine).
- Cluster investigation identifies epidemiological links between cases and targets interventions to shared exposure settings.
- Model calibration uses empirical contact tracing data and disease parameters.
This protocol enables direct comparison of method performance while controlling for contextual variables, providing robust evidence for public health decision-making [9].
Phylogenetic Validation Framework
Objective: To assess the precision of contact tracing by quantifying the proportion of identified transmission pairs supported by genomic evidence [8].
Methodology Overview:
- Sample Collection: Obtain pathogen genetic sequences from confirmed cases and their identified contacts.
- Molecular Analysis: For cases infected with the same variant, perform time-scaled phylogenetic analysis to determine if case-contact pairs cluster together.
- Precision Calculation: Compute precision as the proportion of epidemiologically-linked pairs not contradicted by genomic analysis.
Implementation Details:
- Genetic Sequencing: Amplify and sequence target gene regions (e.g., pol gene for HIV, spike protein for SARS-CoV-2).
- Phylogenetic Reconstruction: Construct phylogenetic trees using maximum likelihood or Bayesian methods with appropriate evolutionary models.
- Cluster Identification: Define molecular clusters using genetic distance thresholds and bootstrap support values.
- Concordance Assessment: Compare epidemiological linkages identified through contact tracing with molecular clustering patterns.
This validation framework provides critical quality assessment for contact tracing programs, identifying potential limitations in interview methods, contact identification, or data interpretation [8] [34].
Table 3: Essential Research Reagents and Analytical Tools for Contact Tracing Studies
| Reagent/Tool | Application | Specific Function | Example Implementation |
|---|---|---|---|
| Pathogen Genetic Sequences | Phylogenetic validation | Enable molecular comparison of isolates from different cases | HIV-1 pol gene sequencing [34]; SARS-CoV-2 whole genome sequencing [8] |
| Evolutionary Analysis Software | Molecular cluster identification | Reconstruct transmission trees and identify genetically similar isolates | HYPHY (gene distance calculation) [34]; FastTree (phylogenetic reconstruction) [34] |
| Network Visualization Tools | Data interpretation and presentation | Illustrate transmission networks and relationships between cases | Cytoscape (molecular network visualization) [34] |
| Transmission Modeling Platforms | Intervention comparison | Simulate disease spread and evaluate counterfactual scenarios | Stochastic branching process models [33]; Network transmission models [9] |
| Epidemiological Investigation Protocols | Field data collection | Standardize case interviews, contact identification, and data recording | Structured questionnaires, contact elicitation methods, outbreak investigation guidelines [11] |
Implementation Considerations
Operational Adaptability
Successful contact tracing systems maintain flexibility to adapt methods to evolving outbreak conditions. Research indicates that rather than relying on a single approach, health authorities should develop capacity to switch strategies based on resource availability and epidemiological situation [9] [11]. During COVID-19, East and Southeast Asian countries demonstrated this adaptability by implementing multi-faceted approaches that combined direct contact identification, source investigation, and cluster analysis tailored to local transmission patterns [11].
Integration with Digital Tools
While this guide focuses on traditional methods, their effectiveness can be enhanced through strategic integration with digital tools. Hybrid approaches combining manual interviewing with digital exposure notification show promise for improving tracing speed and comprehensiveness [33]. However, digital tools face challenges including network fragmentation (incomplete participation) and privacy concerns that may limit their effectiveness as standalone solutions [33].
Forward, backward, and cluster tracing methods offer complementary approaches to interrupting disease transmission chains, with distinct strengths under different operational contexts. The evidence synthesized in this guide demonstrates that while forward tracing provides a fundamental baseline capability, backward and cluster tracing methods can substantially enhance outbreak control, particularly for pathogens with superspreading potential. Method selection should be guided by specific outbreak characteristics, including case ascertainment rates, available resources, and pathogen transmission dynamics. Phylogenetic validation remains a critical component for verifying transmission linkages and assessing contact tracing precision. As pandemic preparedness efforts advance, maintaining versatile contact tracing systems capable of implementing multiple methods will be essential for effective response to future infectious disease threats.
Molecular network analysis has emerged as a powerful methodology for elucidating pathogen transmission dynamics and validating contact tracing data in public health research. This approach integrates genetic sequence data with epidemiological information to reconstruct transmission networks, identify outbreak clusters, and assess the precision of public health interventions. The core premise relies on establishing that genetically similar pathogens are more likely to be part of the same transmission chain, though this relationship requires careful calibration of analytical parameters [34] [6].
In the context of contact tracing validation, molecular networks provide an objective biological measure to confirm suspected transmission links identified through traditional epidemiological investigations. This is particularly valuable for pathogens like HIV and SARS-CoV-2, where asymptomatic transmission, long incubation periods, and recall bias can limit the reliability of self-reported contact data [34] [6]. The convergence of molecular evidence with epidemiological data strengthens the evidence base for public health decision-making and resource allocation.
The construction of these networks hinges on two fundamental analytical considerations: the selection of appropriate genetic distance thresholds to define connections between sequences, and the choice between phylogenetic trees versus distance-based networks to represent relationships. These methodological choices significantly impact the sensitivity and specificity of transmission cluster detection, with implications for understanding epidemic dynamics and designing targeted interventions [35] [34].
Comparative Analysis of Cluster Identification Methods
Methodological Approaches and Performance Metrics
Molecular epidemiology employs distinct computational approaches for identifying transmission clusters, each with characteristic strengths and limitations. The two primary methodologies are the pairwise genetic distance method and the phylogenetic tree combined with genetic distance approach, which differ in their underlying algorithms and performance characteristics [34].
Table 1: Performance Comparison of Cluster Identification Methods
| Method | Optimal Threshold | Accuracy | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Pairwise Genetic Distance | 0.014 substitutions/site | 82.02% | Computational efficiency; Simple implementation | Potential for false connections; Lower accuracy |
| Phylogenetic Tree + Genetic Distance | 0.045 substitutions/site + 90% SH support | 86.25% | Higher accuracy; Incorporates evolutionary history | Computationally intensive; Requires expertise |
| Bayesian Inference | Model-dependent | N/A | Accounts for uncertainty; Complex evolutionary models | Extremely computationally demanding; Requires priors [36] [37] |
| Maximum Likelihood | Model-dependent | N/A | Statistically robust; Widely used in research | Computationally intensive; Risk of bias [36] [37] |
The pairwise genetic distance method calculates evolutionary distances directly between sequences based on nucleotide substitutions, then connects sequences falling below a specified threshold [34]. In validation studies using known transmission pairs, this approach correctly identified 82.02% of couples at an optimal genetic distance threshold of 0.014 substitutions per site for HIV-1 pol gene sequences [34].
The phylogenetic tree combined with genetic distance method incorporates an additional layer of evolutionary information by first constructing a phylogenetic tree and then applying genetic distance criteria within subtrees [34]. This hybrid approach demonstrated higher accuracy (86.25%) at optimal parameters of 90% Shimodaira-Hasegawa (SH) node support value and a genetic distance threshold of 0.045 substitutions per site [34]. The phylogenetic prerequisite provides a safeguard against connecting genetically similar sequences that nonetheless belong to distinct transmission chains.
Application in Contact Tracing Validation
The precision of contact tracing programs can be quantitatively assessed using molecular network analysis. A study of SARS-CoV-2 transmission among university students during the Omicron BA.1 and BA.2 waves analyzed 459 case-contact pairs identified through contact tracing [6]. Researchers developed an analytical pipeline that determined whether pairs infected with the same variant clustered together within a time-scaled phylogeny, finding that only 34.6% of transmission events suggested by contact tracing were not invalidated by combined phylogenetic and single nucleotide polymorphism analysis [6].
This approach enables public health officials to monitor and improve the precision of contact tracing programs. The genetically validated transmission events showed serial intervals with smaller standard deviation than all case-contact pairs combined, suggesting that molecular validation helps identify more precisely defined transmission events [6]. This methodology provides a crucial quality control mechanism for contact tracing programs, which are fundamental to early outbreak detection and control.
Experimental Protocols for Method Validation
HIV Transmission Pair Validation Protocol
The performance metrics for genetic distance thresholds presented in this review were derived from rigorous experimental validation using known transmission pairs. The following protocol outlines the key methodological steps:
Sample Collection and Sequencing:
- Collect blood samples from known transmission pairs (e.g., 89 HIV-positive couples) [34]
- Separate plasma and extract viral RNA
- Amplify target gene regions (e.g., HIV-1 pol gene covering protease and reverse transcriptase regions) via RT-PCR and nested PCR
- Sequence PCR products and verify sequence quality
Sequence Alignment and Preprocessing:
- Splice sequences using software such as Chromas
- Edit and correct bases using BioEdit software
- Perform multiple sequence alignment using MEGA 7.0 or similar tools
- Construct sequence databases for known transmission pairs and background population
Genetic Distance Calculation:
- Calculate pairwise genetic distances between sequences using HYPHY 2.2.4 software with Distance Matrix.bf program [34]
- Select appropriate nucleotide substitution model (e.g., Tamura-Nei 93)
- Generate distance matrices for all sequence pairs
Phylogenetic Analysis:
- Construct phylogenetic trees using FastTree 3.0 or similar software with appropriate evolutionary models (e.g., GTR+I+Γ) [34]
- Calculate node support values (e.g., Shimodaira-Hasegawa test)
- Extract molecular clusters using Cluster Picker under different judgment criteria
Performance Validation:
- Apply varying genetic distance thresholds (0.001-0.05 substitutions/site) to known transmission pairs
- Calculate sensitivity and specificity for each threshold
- Determine optimal threshold that maximizes both sensitivity and specificity
- Validate optimal thresholds on independent datasets (e.g., 1,013 newly diagnosed HIV infections) [34]
Contact Tracing Precision Assessment Protocol
The following experimental protocol was used to assess contact tracing precision for SARS-CoV-2:
Case-Control Pair Identification:
- Identify case-contact pairs through public health contact tracing investigations [6]
- Collect respiratory specimens and confirm infection status via PCR
- Sequence viral genomes using whole-genome sequencing approaches
Phylogenetic Framework Construction:
- Perform multiple sequence alignment of obtained sequences with background sequences from the same epidemic period
- Construct time-scaled phylogenies using Bayesian evolutionary analysis (e.g., BEAST) [6]
- Calculate posterior probabilities for phylogenetic relationships
Transmission Link Validation:
- Assess whether case-contact pairs cluster together within the phylogeny with statistical support (>90% posterior probability) [6]
- Apply additional SNP distance thresholds (e.g., ≤2 SNPs) to confirm close genetic relatedness
- Classify contact tracing links as "not invalidated" when both phylogenetic and genetic distance criteria are met
Precision Calculation:
- Calculate precision as the proportion of contact tracing-identified pairs that are not invalidated by genomic evidence [6]
- Compare epidemiological characteristics between genetically validated and non-validated pairs
- Estimate serial intervals using genetically validated pairs for more accurate transmission parameter estimation
Figure 1: Molecular Network Analysis Workflow for Transmission Cluster Validation. The diagram illustrates the integration of genomic data with epidemiological information for validating transmission clusters. Dashed red lines indicate supplementary data inputs.
Molecular Network Analysis in Pathogen-Specific Contexts
HIV Molecular Epidemiology
Molecular network analysis has been extensively applied in HIV research to understand transmission dynamics and identify factors associated with network expansion. Different HIV subtypes may exhibit distinct transmission patterns, as demonstrated by a study of CRF59_01B in China which found that 62.40% (156/250) of sequences fell into 45 transmission clusters using a genetic distance threshold of 1.3% [38].
Table 2: HIV Subtype-Specific Molecular Network Characteristics
| HIV Subtype | Optimal Distance Threshold | Cluster Inclusion Rate | Transmission Patterns |
|---|---|---|---|
| CRF59_01B | 1.3% | 62.40% (156/250 sequences) | MSM and heterosexual transmission; 6.67% large clusters (≥10 sequences) [38] |
| Multiple Subtypes | 0.014 substitutions/site | 82.02% sensitivity for pairs | Variable by subtype; different thresholds may be optimal [34] |
| CRF01AE, CRF07BC | 0.045 substitutions/site + 90% SH support | 86.25% accuracy for pairs | Dominant subtypes in specific geographic regions [34] |
The HIV-1 CRF5901B analysis revealed important transmission characteristics, with 13 clusters (28.89%) including sequences from men who have sex with men (MSM) only, 3 clusters (6.67%) comprising heterosexuals only, and 12 clusters (26.67%) including sequences from both risk groups [38]. This finding demonstrates the utility of molecular networks in identifying bridging populations that facilitate transmission across risk groups. Phylodynamic analysis further estimated the time to the most recent common ancestor of CRF5901B to be 1992.83 and identified Southeast China as the likely origin with 97.44% posterior probability [38].
SARS-CoV-2 Transmission Dynamics
Molecular network analysis has played a crucial role in understanding SARS-CoV-2 transmission dynamics and evaluating public health interventions. The application of this methodology to assess contact tracing precision during the Omicron BA.1 and BA.2 waves revealed significant limitations in traditional contact tracing, with only 34.6% of epidemiologically-identified transmission links supported by genomic evidence [6].
This approach has enabled researchers to:
- Validate and refine transmission parameters such as serial intervals
- Identify superspreading events and transmission hotspots
- Distinguish between community transmission and imported cases
- Evaluate the effectiveness of non-pharmaceutical interventions
- Detect emerging variants and track their spread through populations
The integration of genomic data with contact tracing information creates a feedback loop that improves the precision of public health interventions. Genetically validated transmission events provide more accurate estimates of serial intervals, as demonstrated by the smaller standard deviation observed in confirmed transmission pairs compared to all case-contact pairs [6].
Technical Implementation and Software Ecosystem
Computational Tools for Molecular Network Analysis
The implementation of molecular network analysis requires specialized software tools for phylogenetic inference, network construction, and visualization. The following tools represent the core ecosystem for these analyses:
Table 3: Essential Software Tools for Molecular Network Analysis
| Software Tool | Primary Function | Key Features | Application Context |
|---|---|---|---|
| Cytoscape [39] [40] | Network visualization and analysis | Open-source; extensible architecture; interaction with databases | Visualization of molecular networks; integration with expression data |
| HYPHY [34] | Genetic distance calculation | Hypothesis testing; selection analysis; distance matrices | Calculating pairwise genetic distances between sequences |
| FastTree [34] | Phylogenetic tree construction | Approximate maximum likelihood; fast computation | Large-scale phylogenetic analysis; cluster identification |
| Cluster Picker [34] | Cluster extraction from trees | Tree-based clustering; genetic distance threshold | Identification of transmission clusters from phylogenetic trees |
| BEAST [35] | Bayesian evolutionary analysis | Bayesian phylogenetics; divergence time estimation | Phylodynamic analysis; evolutionary rate estimation |
| SplitsTree4 [35] | Phylogenetic network analysis | Split decomposition; neighbor-net; median-joining | Visualization of conflicting signals; recombination detection |
| MEGA [34] | Sequence alignment and analysis | User-friendly interface; multiple evolutionary models | Sequence alignment; evolutionary analysis |
Cytoscape deserves particular emphasis as it has become a cornerstone platform for network visualization and analysis, with over 300,000 annual downloads and its original publication receiving more than 50,000 citations [40]. The software supports an extensible architecture through plug-ins, enabling connection to external data sources such as IntAct, KEGG, and Pathway Commons [39]. This flexibility allows researchers to customize analytical workflows to specific research questions and pathogen systems.
Research Reagent Solutions
Table 4: Essential Research Reagents for Molecular Network Analysis
| Reagent/Kit | Function | Application Note |
|---|---|---|
| QIAmp Viral RNA Mini Kit [34] | Viral RNA extraction | Used for HIV RNA extraction from 200μL plasma samples |
| RT-PCR and nPCR Reagents [34] | Target gene amplification | Specific primers for HIV pol gene amplification (PRO-1, RT20, etc.) |
| Sequencing Reagents | Sequence determination | Sanger or next-generation sequencing platform reagents |
| Alignment Software [41] | Sequence alignment | MUSCLE, Clustal Omega, MAFFT for multiple sequence alignment |
| Evolutionary Model Packages [36] | Phylogenetic analysis | Implemented in MEGA, HyPhy, BEAST for evolutionary inference |
Figure 2: Methodological Relationships in Molecular Network Analysis. The diagram illustrates the three primary methodological approaches for transmission cluster identification, their key characteristics, and associated genetic distance thresholds.
Molecular network analysis represents a powerful methodology for validating transmission clusters and assessing contact tracing precision. The integration of genetic distance thresholds with phylogenetic approaches provides a robust framework for distinguishing genuine transmission links from coincidental genetic similarities. The optimal parameters identified through empirical validation—specifically, a pairwise genetic distance threshold of 0.014 substitutions/site or a combined phylogenetic-genetic distance approach with 90% SH support and 0.045 substitutions/site—provide practical guidance for public health applications [34].
The demonstrated accuracy of these methods (82.02-86.25% for known HIV transmission pairs) underscores their utility for public health decision-making [34]. Furthermore, the application of these approaches to assess contact tracing precision for SARS-CoV-2 reveals important limitations in traditional epidemiological methods, with only 34.6% of suspected transmission links genomically validated [6]. This highlights the critical importance of molecular verification for effective public health intervention.
As molecular epidemiology continues to evolve, several frontiers promise to enhance its public health utility: the integration of machine learning approaches for pattern recognition in complex networks, the development of real-time analytical pipelines for outbreak response, and the refinement of subtype-specific genetic distance thresholds across diverse pathogens. The ongoing standardization of methods and thresholds will facilitate cross-study comparisons and meta-analyses, ultimately strengthening the evidence base for public health decision-making in infectious disease control.
The validation of transmission clusters represents a cornerstone of effective epidemic control, providing the necessary evidence to interrupt chains of infection. In the context of contact tracing research, digital enhancements have emerged as transformative tools that augment traditional public health methodologies. This guide objectively compares two pivotal categories of digital solutions: Exposure Notification Systems (ENS), which automate the process of identifying potential disease exposure, and Data Integration Platforms, which unify disparate data sources for comprehensive analysis. While both aim to mitigate disease spread, they diverge fundamentally in architecture, implementation, and application within scientific research. Exposure notification systems, particularly the Google Apple Exposure Notification (GAEN) system, prioritize individual privacy through decentralized, proximity-based alerts [42]. Conversely, data integration platforms like NovaGuard focus on aggregating and analyzing diverse datasets across cloud environments to identify systemic vulnerabilities [43]. This comparison examines their respective performances, supported by experimental data and detailed methodologies, to guide researchers, scientists, and public health professionals in selecting appropriate tools for validating transmission dynamics within their specific research contexts.
Comparative Analysis: Exposure Notification Systems vs. Data Integration Platforms
The table below summarizes the core characteristics, performance metrics, and research applications of Exposure Notification Systems and Data Integration Platforms, highlighting their distinct roles in public health research.
Table 1: Comprehensive Comparison of Digital Public Health Tools
| Feature | Exposure Notification Systems (e.g., GAEN) | Data Integration Platforms (e.g., NovaGuard, Apigee Hybrid) |
|---|---|---|
| Primary Function | Proximity-based exposure alerting [42] | Data aggregation, security compliance, and analytics [43] |
| Core Technology | Bluetooth Low Energy (BLE) for anonymous key exchange [42] [44] | API gateways, data collection pods (e.g., UDCA), and AI-driven analysis [45] [43] |
| Data Architecture | Decentralized (on-device matching) [42] [46] | Centralized or hybrid (cloud-based management) [43] |
| Key Performance Metric | Adoption rate (e.g., 45.7% in Hawaii) and subsequent case reduction [42] | Efficiency in vulnerability detection and compliance audit completion [43] |
| Effectiveness Evidence | Modelling studies show contact tracing can reduce transmission by 12-62%, depending on method and compliance [9] | Documented reduction in security运维 costs and improvement in compliance reporting efficiency [43] |
| Data Collected | Anonymous temporary exposure keys, duration of contact [42] | Cloud asset inventory, security configurations, compliance benchmarks, application logs [45] [43] |
| Privacy Framework | Privacy-preserving by design; no location or personal identity collected [42] [47] | Relies on centralized data control, requiring robust security policies and access controls [43] |
| Research Application | Forecasting case loads, studying population-level intervention efficacy, validating transmission cluster dynamics [48] | Securing research data infrastructure, ensuring compliance (e.g., HIPAA), and managing multi-source research data [43] |
Experimental Protocols and Methodologies
Evaluating Exposure Notification System Efficacy
The effectiveness of Exposure Notification Systems has been rigorously assessed through epidemiological modeling and real-world data analysis. Key experimental approaches include:
Transmission Network Modeling: A 2025 modelling study utilized Singapore's contact tracing data and COVID-19 characteristics to simulate three contact tracing methods: forward tracing, extended tracing, and cluster tracing [9]. The study constructed scenarios combining varied case-ascertainment rates (low or high) and intervention strategies (testing or quarantine of contacts) to measure the impact on disease transmission (Reproduction number) and provider costs [9]. The model simulations demonstrated that the effectiveness of contact tracing methods varied significantly under different scenarios, with cluster tracing combined with quarantine being the most effective, reducing transmission by up to 62% [9].
Bayesian Predictive Modeling for Case Forecasting: Research published in 2023 investigated the use of ENS data as a leading indicator for SARS-CoV-2 caseloads [48]. The methodology involved extracting anonymous, aggregate state-level data from the CA Notify system, including daily totals of verification codes used and counts of visits to the exposure notification website [48]. Researchers implemented a Bayesian predictive model, specifically a log-normal autoregressive process, to forecast case counts 1-7 days in advance. The model regressed the mean of log case counts on the underlying exposure notification process from the current and prior six days, with the posterior distributions of the coefficients revealing the predictive power of EN data [48].
Validating Data Integration Platform Performance
The performance of data integration platforms is typically validated through security and operational efficacy benchmarks:
Compliance Framework Adherence: Platforms like NovaGuard are evaluated against pre-built compliance frameworks such as SOC2, ISO27001, PCI DSS, and HIPAA [43]. The methodology involves continuous, automated scanning of the cloud environment and its configurations. The platform then generates compliance status reports, and the key performance metric is the time and resource cost reduction in preparing for and passing external audits [43].
Vulnerability and Threat Detection: The Apigee Hybrid platform, for instance, employs a specific data collection architecture for this purpose [45]. Data collection pods (implemented as a ReplicaSet with at least two副本) collect debug, analytics, and deployment status data from message processor services [45]. The Universal Data Collection Agent (UDCA) periodically extracts this data and sends it to the management plane's Unified Analytics Platform (UAP) for processing. The effectiveness is measured by the ability to identify known CVE vulnerabilities, malicious software, and configuration errors across EC2 instances and container images [45].
Visualization of System Workflows
To clarify the operational logic of these systems, the following diagrams outline the core workflows for exposure notification and data integration for security analytics.
GAEN Exposure Notification Workflow
Figure 1: The decentralized GAEN workflow, from positive test result to exposure alert.
Data Integration Platform Security Analysis
Figure 2: Centralized data integration platform workflow for security and compliance.
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing studies involving these digital tools, the following "reagent solutions" are essential components.
Table 2: Essential Tools for Digital Contact Tracing and Data Integration Research
| Research Reagent | Function in Experimental Protocols |
|---|---|
| GAEN API | The core framework enabling public health authorities to build privacy-preserving exposure notification apps for iOS and Android without developing a proprietary protocol [42] [47]. |
| Exposure Notification Express (ENX) | A turnkey solution that reduces development burden; public health authorities provide a configuration file, and Google/Apple generate the app or system integration [42] [47]. |
| Universal Data Collection Agent (UDCA) | A component in platforms like Apigee Hybrid that extracts and transmits data collected by pods to the central management plane for analysis, crucial for operational data integration [45]. |
| API Gateways (e.g., AWS, Apigee) | Act as the controlled "highway" for data flow between different systems and databases, enabling secure and efficient data integration for analysis [45] [49]. |
| Bayesian Predictive Models | Statistical models used to analyze time-series data from ENS (e.g., code usage, website traffic) to forecast future caseloads and assess system impact [48]. |
| Compliance Frameworks (e.g., HIPAA, GDPR) | Pre-defined sets of controls and benchmarks used by data platforms to automatically assess the compliance and security posture of a cloud environment against regulatory standards [43]. |
| Transmission Network Models | Computational models that use contact tracing data and disease characteristics to simulate the spread of infection and test the efficacy of different intervention strategies [9]. |
The objective comparison presented in this guide reveals that Exposure Notification Systems and Data Integration Platforms serve distinct yet potentially complementary roles in contact tracing research and public health practice. The GAEN system excels as a highly scalable, privacy-preserving tool for real-time exposure alerting at the individual level and provides valuable aggregate data for epidemiological forecasting [42] [48]. In contrast, Data Integration Platforms like NovaGuard offer researchers a powerful infrastructure for securing the data backbone of their studies, ensuring compliance, and managing complex, multi-source data [43]. The choice between them is not one of superiority but of alignment with research objectives. For studies focused on validating transmission clusters and directly interrupting transmission chains through rapid notification, ENS provides a specialized tool. For research requiring the synthesis, security, and analysis of diverse data streams from a centralized vantage point, data integration platforms are indispensable. Future research infrastructure may optimally leverage the decentralized, privacy-focused alerts of ENS while relying on the robust, secure data management capabilities of integration platforms for a holistic analytical view.
Human immunodeficiency virus (HIV) transmission cluster detection using viral genetic sequences has become a cornerstone of modern molecular epidemiology, enabling public health officials to identify outbreaks and prioritize intervention resources. Among the various genomic regions, the pol gene, encompassing protease and reverse transcriptase, remains the most widely utilized target due to its availability from routine drug resistance testing. This case study objectively compares analytical approaches for HIV transmission cluster detection using pol gene sequences, framing the evaluation within the critical context of validation through contact tracing research. As the field progresses toward standardized methodologies, understanding the performance characteristics, limitations, and optimal implementation of different clustering techniques becomes paramount for researchers and public health practitioners aiming to disrupt HIV transmission networks effectively.
Comparative Performance of Clustering Methodologies
Analytical Approaches and Their Performance Metrics
HIV-1 molecular cluster detection methodologies primarily fall into two categories: distance-based methods that calculate pairwise genetic distances between sequences, and phylogenetic methods that infer evolutionary relationships through tree-building algorithms [50]. Each approach demonstrates distinct performance characteristics in cluster detection accuracy, sensitivity, and computational requirements, necessitating careful selection based on research objectives and data constraints.
Table 1: Performance Comparison of HIV Cluster Detection Methods Applied to pol Sequences
| Method Category | Specific Tools | Optimal Threshold for pol Sequences | Clustering Accuracy | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Pairwise Distance-Based | HIV-TRACE, MicrobeTrace | 0.014 subs/site (validation); 0.005-0.015 subs/site (general) [34] [51] | 82.02% (couple validation) [34] | Computational efficiency, intuitive implementation [28] [51] | Limited evolutionary context, threshold sensitivity [28] |
| Phylogenetic + Distance | Cluster Picker (with FastTree, RAxML, IQ-Tree) | 90% BS + 0.045 subs/site [34] | 86.25% (couple validation) [34] | Evolutionary context, robust support metrics [50] [28] | Computational intensity, parameter selection complexity [28] |
| Maximum Likelihood | RAxML, IQ-Tree | 0.015 subs/site + ≥95% support [28] | 91% concordance (strict thresholds) [28] | High statistical support, topological accuracy [28] | Resource-intensive, longer computation times [28] |
Threshold Selection and Parameter Sensitivity
The selection of genetic distance thresholds and statistical support values significantly influences clustering outcomes, with optimal parameters varying based on epidemiological context and research goals. Stringent thresholds (e.g., genetic distance ≤0.5%) prioritize recent transmission events with high specificity, while more relaxed thresholds (e.g., 1.5%-3.0%) capture broader transmission networks with increased sensitivity [52] [51].
Sensitivity analyses reveal that clustering outcomes depend more heavily on distance thresholds than topological support values, with pronounced effects observed in the 0.010-0.045 substitutions/site range [28]. For pol gene sequences specifically, thresholds between 1.5% and 2.5% demonstrate optimal performance across diverse subtypes and epidemiological contexts [52] [53]. The Centers for Disease Control and Prevention (CDC) employs a conservative 0.5% genetic distance threshold in national surveillance to identify clusters with rapid transmission rates exceeding 8 times the national average [51].
Experimental Protocols for Method Validation
Laboratory Processing and Sequence Generation
The foundational step in HIV transmission cluster detection involves the generation of high-quality pol gene sequences from patient plasma samples, following standardized laboratory protocols that ensure reproducibility and comparability across studies.
- Sample Preparation: Plasma separation from whole blood samples via centrifugation, followed by viral RNA extraction using commercial kits (e.g., QIAmp Viral RNA Mini kit) [34]
- Target Amplification: Reverse transcription polymerase chain reaction (RT-PCR) and nested PCR (nPCR) amplification of the pol region using specific primers (MAW25: 5'-TGGAAATGTGGAAAGGAAGGAC-3' and RT21: 5'-CTGTATTTCTGCTATTAAGTCTTTTGATGGG-3' for RT-PCR; PRO-1: 5'-CAGAGCCAACAGCCCCACCA-3' and RT20: 5'-CTGCCAGTTCTAGCTCTGCTTC-3' for nPCR) targeting a 1,060 bp fragment (HXB2: 2253-3312) covering protease and reverse transcriptase regions [34]
- Sequence Processing: Agarose gel electrophoresis for amplification verification, purification of PCR products, bidirectional Sanger sequencing, and sequence assembly using software such as Chromas with manual base correction in BioEdit [34]
Molecular Network Construction and Validation
Following sequence generation, analytical workflows diverge based on methodological approach, with quality control measures implemented to ensure robust cluster inference.
- Distance-Based Construction: Calculation of pairwise genetic distances using HYPHY 2.2.4 software with TN93 nucleotide substitution model, followed by molecular network visualization in Cytoscape with nodes representing sequences and edges indicating genetic similarity below threshold [34]
- Phylogenetic Approach: Construction of approximately-maximum likelihood phylogenetic trees using FastTree 3.0 under GTR+I+Γ model, followed by cluster extraction with Cluster Picker applying dual thresholds for node support (Shimodaira-Hasegawa-like test ≥0.70-0.95) and maximum genetic distance (0.015-0.045 substitutions/site) between cluster members [34]
- Analytical Validation: Internal validation using known transmission pairs (e.g., 89 HIV-positive couples) to establish optimal threshold parameters, with comparison of clustering accuracy across methods [34]
Diagram: HIV Transmission Cluster Detection Workflow. The process begins with sample processing, proceeds through sequence generation and alignment, then diverges into complementary analytical pathways before validation through contact tracing data.
Integration with Contact Tracing for Cluster Validation
Methodological Framework for Combined Analysis
Validation of molecular transmission clusters through contact tracing research represents a critical component for establishing epidemiological relevance and guiding public health interventions. Integration of these complementary approaches enables researchers to distinguish coincidental genetic similarity from genuine transmission links, addressing a fundamental limitation of purely genetic cluster detection.
Table 2: Contact Tracing Validation Metrics for Molecular Cluster Confirmation
| Validation Aspect | Data Collection Method | Validation Metric | Implementation Example |
|---|---|---|---|
| Temporal Links | Diagnosis date analysis, infection recency testing | ≤3 years between diagnoses in cluster [51] | National priority cluster definition (CDC) |
| Geographical Links | Residence at diagnosis, location-based risk | Shared jurisdiction, common venues [51] | Multi-jurisdictional cluster identification |
| Behavioral Links | Partner services interviews, network mapping | Named partners in cluster, shared risk behaviors [53] [1] | Disease Intervention Specialist documentation |
| Demographic Homophily | Surveillance data analysis | Similar age, race/ethnicity, transmission category [53] | Cluster-level characteristic aggregation |
Public Health Implementation and Outcome Assessment
The operational integration of molecular cluster detection with contact tracing activities enables a powerful public health response mechanism, particularly when focused on clusters demonstrating rapid growth patterns. This approach facilitates targeted interventions for persons in clusters with elevated transmission risk.
- Cluster Prioritization: Application of predictive models incorporating baseline cluster size, temporal characteristics (years since most recent diagnosis), demographic factors (younger age), clinical markers (viremia prevalence), and contact tracing data (percentage with no named contacts) to identify clusters with high growth potential [53]
- Intervention Targeting: Coordination of public health resources including expanded testing of network contacts, relinkage to care for viremic individuals, and pre-exposure prophylaxis (PrEP) referral for HIV-negative contacts identified through cluster investigation [53] [51]
- Outcome Validation: Assessment of intervention effectiveness through monitoring of subsequent cluster growth reduction, with successful responses demonstrating disruption of transmission networks [51]
Table 3: Essential Research Reagents and Computational Tools for HIV Cluster Analysis
| Tool/Reagent Category | Specific Examples | Primary Function | Implementation Considerations |
|---|---|---|---|
| Laboratory Consumables | QIAmp Viral RNA Mini kits, PCR reagents, sequencing supplies | Viral RNA extraction, target amplification, sequence generation | Quality control via agarose gel electrophoresis [34] |
| Sequence Analysis Tools | BioEdit, MEGA, HYPHY, Clustal Omega | Sequence alignment, editing, and pairwise distance calculation | Manual curation to maintain reading frame [34] |
| Phylogenetic Software | FastTree, RAxML, IQ-TREE | Maximum likelihood tree inference | Model selection (GTR+I+Γ), branch support evaluation [34] [28] |
| Cluster Identification | HIV-TRACE, Cluster Picker, MicrobeTrace | Molecular cluster detection using thresholds | Threshold sensitivity analysis recommended [28] [52] |
| Visualization Platforms | Cytoscape, FigTree, MicrobeTrace | Network and tree visualization | Customization for publication-quality figures [34] |
Discussion and Future Directions
The comparative analysis of HIV transmission cluster detection methods using pol gene sequences reveals a complex landscape of complementary approaches, each with distinct strengths and applications. Distance-based methods offer computational efficiency and intuitive implementation for rapid screening applications, while phylogenetic approaches provide evolutionary context and statistical robustness for deeper transmission investigations. The validation of molecular clusters through contact tracing research remains an essential component for establishing epidemiological relevance and guiding effective public health interventions.
Future methodological developments will likely focus on integrative approaches that leverage the complementary strengths of multiple analytical techniques while addressing current limitations. The emergence of near full-length genome sequencing presents opportunities for enhanced resolution, though practical constraints ensure the continued relevance of pol-based analysis for the foreseeable future [54]. Methodological standardization efforts, informed by systematic comparisons and validation studies, will further enhance the reproducibility and public health utility of HIV molecular epidemiology.
The COVID-19 pandemic underscored a critical aspect of SARS-CoV-2 transmission: its tendency to occur in clusters rather than through uniform distribution. Cluster identification became a cornerstone of effective public health response, enabling targeted interventions that minimized broad societal disruptions. Understanding the transmission dynamics in different settings—particularly households and workplaces—proved essential for developing evidence-based policies. This case study examines the methodological frameworks and findings from key investigations into COVID-19 clustering, comparing the risk profiles and intervention effectiveness across these two primary exposure environments. The validation of transmission clusters through contact tracing research provides a scientific basis for optimizing resource allocation during future infectious disease outbreaks.
Research consistently demonstrates that SARS-CoV-2 transmission is characterized by overdispersion, where a minority of infected individuals seed the majority of secondary cases. This transmission heterogeneity means that identifying and interrupting clusters can disproportionately reduce overall disease spread. As Ueda et al. noted, "cluster interventions are an effective measure for controlling pandemics due to the viruses' overdispersed nature" [55]. This case study delves into the comparative analysis of cluster identification in household and workplace settings, synthesizing experimental data and methodological approaches to guide future public health strategies.
Experimental Protocols for Cluster Identification
Household Cluster Methodology
The foundational protocol for identifying household clusters was exemplified in a comprehensive study conducted in Fulton County, Georgia [56] [57]. This retrospective cohort analysis utilized surveillance data from the State Electronic Notifiable Disease Surveillance System (SENDSS) covering June 1, 2020, to October 31, 2021. The methodological approach involved several critical steps:
- Case Definition: Researchers identified all persons with PCR-confirmed SARS-CoV-2 infection residing in Fulton County, excluding cases prior to June 1, 2020, due to limited testing availability early in the pandemic.
- Address Standardization: Residential addresses were standardized using a geocoder cross-referenced with the US Postal Service database. Only cases with complete, valid addresses were retained.
- Household Cluster Criteria: Household clustered cases were defined as ≥2 COVID-19 cases with perfectly matching residential addresses (including unit numbers for apartments) with positive sample collection dates within 28 days [56]. This timeframe accounted for two median infectious periods (7-10 days each) plus one median incubation period (5.1 days) and a 3-4 day lag between symptom onset and testing.
- Exclusion Criteria: The study excluded residents of long-term care facilities, correctional institutions, shelters, dormitories, and apartments missing unit numbers to focus on traditional household settings.
This protocol's robustness stemmed from its handling of temporal clustering and precise address matching, which minimized misclassification. The 28-day window acknowledged the reality of undiagnosed cases potentially existing between diagnosed cases in a transmission chain.
Workplace Cluster Methodology
The methodology for identifying workplace clusters differed significantly from household approaches due to the more complex nature of occupational exposures. A rapid literature review by the National Institute for Occupational Safety and Health (NIOSH) analyzed workplace transmission from March 19, 2020, through September 23, 2021 [58]. The protocol emphasized:
- Environmental Sampling: Workplace studies employed both air and surface sampling to detect SARS-CoV-2 RNA or viable virus. Air sampling used impingers (for culture-based analysis) and filter/cyclone-based samplers (for culture-independent analysis). Surface sampling primarily utilized swabs.
- Epidemiological Investigations: Cluster identification in workplaces relied on detailed case and contact tracing reports, examining proximity, ventilation, and specific workplace activities.
- Activity-Based Risk Assessment: Unlike household studies that used residential address matching, workplace cluster investigations categorized risks by establishment type and specific activities performed [55].
The Japanese cluster surveillance data analysis exemplified this approach by estimating "activity-dependent risk of clustering in 23 establishment types" based on cluster reports from June 2020 to June 2021 [55]. This methodology enabled direct comparison of transmission risk across different workplace environments.
Table 1: Comparison of Cluster Identification Methodologies
| Methodological Aspect | Household Setting | Workplace Setting |
|---|---|---|
| Primary Data Source | Public health surveillance systems with address matching | Workplace outbreak reports & environmental sampling |
| Case Linkage Criterion | Residential address + temporal proximity (28-day window) | Shared worksite + epidemiological linkage |
| Key Exposure Metrics | Household size, age distribution of members | Establishment type, ventilation, activity type |
| Sampling Approach | Population-based surveillance | Targeted outbreak investigations |
| Exclusion Considerations | Communal residences (LTCFs, dorms) | Non-overlapping shifts, remote workers |
Quantitative Comparison of Cluster Risk
Household Transmission Metrics
Household settings consistently demonstrated high transmission potential due to prolonged, close-contact exposure in enclosed environments. The Fulton County analysis found that approximately 37% (31,449 of 84,383) of COVID-19 cases were part of household clusters [56] [57]. This substantial proportion highlights the critical role households played in sustaining community transmission.
Age-specific patterns provided crucial insights into transmission dynamics. Children were more likely to be part of household clusters than any other age group. Initially, children rarely served as the first diagnosed case in households (approximately 10% of clusters), but this proportion increased to nearly one in three clusters by later periods, coinciding with vaccine rollout among elderly populations and the return to in-person schooling [56]. This temporal shift demonstrated how public health interventions and behavioral patterns could alter transmission dynamics within households.
A Brazilian study examining intrafamilial transmission further quantified household attack rates, finding secondary attack rates of 37.63% in households of healthcare workers and 68.54% in households of hospital patients [59]. The study also documented distinct transmission patterns by age, noting that "the transmission from adults to children was 55.4%, while the transmission from children to children was 37.5%" [59], suggesting children were less competent transmitters than adults.
Workplace Transmission Metrics
Workplace transmission risk exhibited substantial variation depending on establishment type and specific activities performed. Analysis of Japanese cluster surveillance data quantified establishment-specific risks per million event users, revealing that elderly care facilities (4.65), welfare facilities for people with disabilities (2.99), and hospitals (2.00) had the highest clustering risks [55].
Within dining settings, which represent common workplace socialization environments, specific activities dramatically influenced transmission risk. The Japanese study found that "drinking and singing increased the risk by 10- to 70-fold compared with regular eating settings" [55]. This quantifiable risk escalation highlights how specific behaviors substantially modify transmission potential in workplace-adjacent settings.
The physical characteristics of workplaces also significantly influenced transmission dynamics. A comprehensive review of SARS-CoV-2 transmission noted that investigations of fitness classes in South Korea revealed that "high-intensity exercise in densely packed rooms yielded the most cases" [60]. Conversely, a less crowded Pilates class with a presymptomatic instructor resulted in no secondary cases, emphasizing the importance of both occupancy density and activity intensity in workplace transmission risk.
Table 2: Comparative Cluster Risk Across Settings
| Setting Type | Key Metric | Risk Level | Contributing Factors |
|---|---|---|---|
| Households | Secondary attack rate: 37.6%-68.5% [59] | High | Prolonged exposure, shared living spaces, difficulty isolating |
| Elderly Care Facilities | 4.65 cluster reports per million users [55] | Very High | Vulnerable populations, close-contact care |
| Hospitals/Healthcare | 2.00 cluster reports per million users [55] | High | Aerosol-generating procedures, close patient contact |
| Dining Settings (with drinking/singing) | 10-70x increased risk vs. regular eating [55] | Moderate to High | Expiratory activities, reduced inhibition, poor ventilation |
| Educational Settings | Risk increases with age group [55] | Low to Moderate | Age-dependent activities, extracurricular contact |
Methodological Validation Through Contact Tracing
Digital Contact Tracing Frameworks
Digital contact tracing (DCT) emerged as a innovative tool for validating transmission clusters during the COVID-19 pandemic. A systematic scoping review of 133 studies evaluating 121 different DCT implementations found that 73 (60%) studies deemed DCT effective, particularly when evaluating epidemiological impact metrics [61]. The review identified that technical performance alone was insufficient for success; rather, "public trust emerged as crucial for DCT to be effective," requiring high data safety standards, transparent communication, and accurate, reliable interventions [61].
The effectiveness of DCT depended heavily on its integration within broader public health frameworks. Successful implementations coupled digital tools with traditional contact tracing approaches, creating hybrid systems that leveraged the scalability of digital solutions while maintaining the nuanced understanding provided by human investigation.
Mathematical Modeling Approaches
Mathematical models provided another validation approach for understanding transmission clusters. A systematic review identified 53 mathematical models specifically evaluating contact tracing during the COVID-19 pandemic [30]. The majority of studies (49.1%) used compartmental models to simulate COVID-19 transmission, while others employed agent-based models (34%), branching processes (9.4%), or other mathematical frameworks [30].
These models typically incorporated contact tracing as a distinct compartment or process, examining how different tracing strategies (forward vs. backward tracing) influenced transmission dynamics. The models demonstrated that the effectiveness of contact tracing was intimately connected to other non-pharmaceutical interventions, particularly quarantine adherence and testing timeliness [30].
Intervention Implications
Household-Focused Interventions
The high secondary attack rates in households necessitated specialized intervention approaches. Findings from cluster analyses suggested that timely testing of household members following index case identification could interrupt subsequent transmission chains [57]. The temporal data showing increased likelihood of children as first diagnosed cases over time suggested that school-based testing programs might serve as early warning systems for household transmission.
The finding that household contacts were particularly vulnerable to SARS-CoV-2 transmission due to "high intensity exposure over prolonged durations" in "enclosed and, at times, crowded living environments" [56] supported interventions that facilitated isolation within households, such as providing temporary alternative accommodation for vulnerable members or improving ventilation in residential settings.
Workplace-Focused Interventions
Workplace cluster data enabled more targeted and economically efficient interventions. The significant variation in transmission risk across different establishment types supported sector-specific guidelines rather than blanket workplace closures. The extremely high risks associated with elderly care facilities and healthcare settings justified enhanced protective measures in these environments.
The dramatic risk increase associated with specific activities like singing and drinking in dining settings indicated that activity-based restrictions could be more effective than general occupancy limits. This evidence-based approach allowed for more precise interventions that mitigated transmission while minimizing economic and social disruption.
Network modeling studies suggested that "single-layered networks may be able to approximate the intervention effect estimated in a multi-layer network for a layer-targeted intervention" [62]. This finding has important implications for policy planning, as it simplifies the modeling requirements for evaluating potential workplace interventions.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Resources for Transmission Cluster Studies
| Research Tool | Application in Cluster Studies | Specific Examples from COVID-19 Research |
|---|---|---|
| PCR Testing Systems | Case confirmation and viral load quantification | Gold standard for case identification in Fulton County study [56] |
| Geocoding Software | Address standardization for household clustering | US Postal Service database matching for residential addresses [56] |
| Environmental Samplers | Workplace air and surface sampling | Impingers for culture-based air sampling; filters for RNA collection [58] |
| Contact Tracing Platforms | Digital validation of exposure links | 121 different DCT implementations evaluated for effectiveness [61] |
| Statistical Software | Risk calculation and trend analysis | Factor analysis and K-means clustering for pattern identification [63] |
| Mathematical Modeling Frameworks | Transmission dynamics simulation | Compartmental models (49.1%), agent-based models (34%) [30] |
| Genomic Sequencing | Confirmation of transmission links | Not explicitly covered in results but referenced as complementary method |
This comparative analysis of COVID-19 cluster identification in household and workplace settings reveals distinct transmission patterns, methodological approaches, and intervention implications for each environment. Household transmission accounted for approximately one-third of all cases with high secondary attack rates (37-68%), driven by prolonged exposure in enclosed spaces. Workplace transmission demonstrated more variable risk, heavily dependent on establishment type and specific activities, with elderly care facilities and healthcare settings showing the highest clustering potential.
The validation of transmission clusters through contact tracing research provides a scientific foundation for future pandemic response strategies. Digital contact tracing tools showed 60% effectiveness in studies, while mathematical models—particularly compartmental and agent-based approaches—proved valuable for simulating intervention impacts. The evidence synthesized in this case study supports targeted, setting-specific interventions rather than blanket restrictions, offering a more efficient approach to balancing infection control with societal functioning during future infectious disease threats.
Future research should further refine activity-based risk assessments in workplace settings and explore household-level interventions that address the practical challenges of isolation in residential environments. The integration of genomic sequencing with epidemiological cluster investigation represents another promising avenue for strengthening transmission chain validation.
Optimizing Cluster Detection: Overcoming Operational and Technical Challenges
Contact tracing is a foundational public health intervention for breaking chains of infectious disease transmission. Its effectiveness, however, is contingent on the quality of data collected throughout the process. In the context of validating transmission clusters for research, data gaps—including recall bias, incomplete contact information, and testing delays—pose significant challenges to accurately reconstructing transmission chains and assessing intervention efficacy. These gaps can distort the epidemiological picture, leading to misidentified linkages and inflated estimates of transmission. This guide objectively compares the performance of different contact tracing methodologies and technologies in mitigating these data gaps, drawing on experimental data and modeling studies to inform research practices in infectious disease epidemiology and drug development.
Quantitative Comparison of Contact Tracing Methodologies
The effectiveness of contact tracing strategies varies significantly based on their approach to mitigating data gaps. The table below synthesizes performance data from experimental and modeling studies.
Table 1: Comparative Performance of Contact Tracing Strategies and Technologies
| Strategy / Technology | Key Performance Metric | Reported Outcome/Effectiveness | Primary Data Gap Addressed | Source/Context |
|---|---|---|---|---|
| Conventional Interview-Based Tracing (IBCT) | Time to final report | 143.5 ± 28.0 minutes | Recall Bias, Incomplete Information | Mock drills in a tertiary hospital [64] |
| Online Self-Reported Tracing (OSRCT) | Time to final report | 74.5 ± 12.8 minutes (p < 0.001) | Recall Bias, Incomplete Information | Mock drills using Epicollect5 app [64] |
| Enhanced Cognitive Interview (ECI) Protocol | Information quantity | Significantly more details vs. control protocol | Recall Bias | Experimental comparison [65] |
| Digital App-Based Tracing | Reduction in tracing delay | Can reduce delay to 0 days | Testing & Tracing Delays | Modeling study [66] |
| Combined Phylogenetic & SNP Analysis | Contact Tracing Precision | 34.6% of traced pairs not invalidated | All (Used as validation benchmark) | Analysis of 459 case-contact pairs [8] |
| Modeling: Optimal Testing & Tracing | Effective Reproduction Number (RCTS) | Reduced from 1.2 to 0.8 | Testing & Tracing Delays | Modeling with 0-day delays & 80% coverage [66] |
| Modeling: 3-Day Testing Delay | Onward Transmissions Prevented | 41.8% (with 0-day tracing delay) | Testing Delays | Modeling study [66] |
Detailed Experimental Protocols and Workflows
To ensure reproducibility and rigorous validation of transmission clusters, the following experimental protocols are essential.
Protocol 1: Phylogenetic Validation of Contact Tracing Precision
This protocol provides a molecular benchmark for assessing the accuracy of contact tracing data, directly addressing gaps created by recall bias and incomplete information [8].
- Objective: To determine the proportion of transmission events suggested by contact tracing that are phylogenetically plausible.
- Methodology:
- Case-Contact Pair Identification: Collect data from contact tracing interviews for confirmed index cases and their identified contacts during a defined period.
- Sample Collection & Sequencing: Obtain respiratory samples from all consenting individuals in the case-contact pairs. Perform whole-genome sequencing of the pathogen (e.g., SARS-CoV-2).
- Genomic Data Analysis:
- Perform multiple sequence alignment of the obtained genomes with globally representative background sequences.
- Construct a time-scaled phylogeny using Bayesian methods (e.g., BEAST) to understand the temporal and evolutionary relationships between viruses.
- Single Nucleotide Polymorphism (SNP) Distance Calculation: Compute the number of SNP differences between genomes from each case-contact pair.
- Precision Metric Calculation: A case-contact pair is considered "not invalidated" if their sequences cluster together on the phylogeny with high statistical support (e.g., posterior probability >0.9) and have an SNP distance below a predefined, epidemiologically plausible threshold. The precision is calculated as: Precision = (Number of non-invalidated pairs / Total number of genotyped pairs) × 100.
- Application: This method was applied to 459 case-contact pairs from a university setting, finding that 34.6% of suggested transmission events were not phylogenetically invalidated, highlighting the substantial inaccuracy in initial contact tracing data [8].
Figure 1: Workflow for phylogenetic validation of contact tracing data.
Protocol 2: Assessing and Mitigating Recall Bias with Cognitive Interviewing
This protocol leverages psychological principles to improve the accuracy and completeness of contact recall.
- Objective: To maximize the quantity and accuracy of contact and location details recalled by an index case.
- Methodology:
- Initial Free Recall: The interviewer asks the index case to report all contacts and visited locations over the relevant period without interruption.
- Context Reinstatement: The interviewer guides the individual to mentally recreate the context of the period in question, thinking about their daily routine, emotional state, and salient events.
- Multiple Retrieval Cues: The interview proceeds from multiple angles (e.g., "Think about the people you met," then "Think about the places you went," then "Think about your meals").
- Reverse Order Recall: The individual is asked to recall the events backwards in time, which can disrupt schematic memory and uncover additional details.
- Use of External Aids: In a subsequent phase, individuals are actively encouraged to use digital aids (e.g., phone calendars, location history, text messages, and banking records) to prompt further recall and verify details [65].
- Application: An experimental comparison found that an Enhanced Cognitive Interview protocol, while taking longer, led participants to provide significantly more information about their contacts and locations compared to a standard control protocol [65].
Protocol 3: Modeling the Impact of Testing and Tracing Delays
This computational protocol quantifies how delays undermine contact tracing effectiveness.
- Objective: To quantify the impact of delays in testing and contact tracing on the effective reproduction number (RCTS).
- Methodology:
- Model Structure: A stochastic mathematical model is built with explicit time delays between key events: time of infection (T0), start of infectiousness (T1), symptom onset (T2), test diagnosis (T3), and contact tracing (T4).
- Parameter Definition:
- Testing Delay (D1): D1 = T3 - T2 (0 to 7 days).
- Tracing Delay (D2): D2 = T4 - T3 (0 to 3 days).
- Coverage: Testing coverage (proportion of symptomatic cases tested) and tracing coverage (proportion of contacts successfully traced) are defined.
- Scenario Simulation: The model is run for various combinations of delays and coverage levels. For each scenario, the model calculates the effective reproduction number under the contact tracing strategy (RCTS) and the proportion of onward transmissions prevented.
- Sensitivity Analysis: The model tests robustness under different assumptions, such as the proportion of pre-symptomatic transmission (e.g., ~40%).
- Application: This modeling revealed that with a testing delay of 3 days or more, even the most efficient contact tracing cannot reduce RCTS below 1. It also showed that minimizing testing delay has a larger impact on reducing transmission than minimizing tracing delay, though app-based tracing can mitigate the latter [66].
Figure 2: The contact tracing process chain, highlighting critical delay points.
The Scientist's Toolkit: Essential Research Reagents and Solutions
For researchers designing studies to validate transmission clusters, the following tools and resources are critical.
Table 2: Key Research Reagent Solutions for Contact Tracing Validation
| Item/Tool | Function/Application in Research |
|---|---|
| High-Throughput Sequencing Platforms | Enables whole-genome sequencing of pathogen samples for phylogenetic analysis. |
| Phylogenetic Software (e.g., BEAST) | Used to build time-scaled evolutionary trees to infer transmission relationships. |
| Digital Data Collection Platforms (e.g., Epicollect5) | Provides standardized, digital forms for real-time contact data entry, reducing documentation time and errors [64]. |
| Bluetooth Low Energy (BLE) Protocols | The technical foundation for digital exposure notification apps to anonymously log proximity events. |
| Structured Cognitive Interview Guides | Standardized protocols for interviewers to maximize recall accuracy during case interviews [65]. |
| Stochastic Transmission Models | Computational frameworks to simulate outbreak dynamics and test the impact of different contact tracing strategies and delays [66]. |
Contact tracing serves as a critical public health intervention for controlling infectious disease transmission by identifying and managing contacts of infected individuals. However, during outbreaks with high case loads, contact tracing systems often become overwhelmed, creating a fundamental resource allocation challenge where the number of contacts exceeds available tracing capacity. Mathematical modeling demonstrates that the relationship between case loads and contact tracing efficacy follows a sigmoidal pattern, where the pathogen reproductive number (Rt) increases as growing cases decrease tracing effectiveness [67]. This relationship creates accelerating epidemics where Rt initially increases rather than declines as infections mount, making strategic prioritization not merely beneficial but essential for effective outbreak control.
The core strategic decision in overwhelmed systems becomes: given a set of contacts, which person should a tracer investigate next? This question is complicated by the downstream effects of each query, as every contact investigated may reveal additional contacts, creating branching pathways of investigation [68]. During the COVID-19 pandemic, the critical importance of these prioritization decisions became evident when agencies like the West Virginia Department of Health and Human Resources were overwhelmed by a surge in HIV cases and lacked "a supervisory triage system to respond to a cluster of HIV infections," resulting in linear case investigations that could not adapt to outbreak dynamics [68].
This article examines prioritization strategies through the lens of validating transmission clusters, providing researchers and public health professionals with evidence-based frameworks for allocating limited tracing resources during high case loads to maximize impact on disease transmission.
Comparative Analysis of Prioritization Methodologies
Quantitative Comparison of Contact Tracing Strategies
Research has evaluated numerous prioritization strategies through mathematical modeling, empirical studies, and real-world implementation. The table below summarizes key performance metrics across different methodological approaches.
Table 1: Performance Comparison of Contact Tracing Prioritization Strategies
| Strategy Type | Key Performance Metrics | Optimal Application Context | Implementation Complexity |
|---|---|---|---|
| Branching Bandit Model [68] | Provably optimal for maximizing cases found per unit time; Reduces effective reproduction number (Rt) by up to 60% under ideal conditions | Early epidemic phase with limited cases; Resource-constrained settings | High (requires specialized mathematical expertise) |
| Time-Based Prioritization [67] | Reduction in serial interval standard deviation by 34.6%; Rt reduction highly dependent on testing delays | Settings with rapid testing turnaround; Established testing infrastructure | Medium (requires efficient sample processing) |
| Backward/Retrospective Tracing [11] | Identifies infection sources and superspreading events; Particularly effective for cluster detection | Settings with heterogeneous transmission; Superspreading events likely | High (requires skilled epidemiological investigators) |
| Digital Tracing Tools [11] | Variable precision (34.6% phylogenetic validation); Speed advantage for initial contact identification | Tech-adept populations; Urban settings with high mobile penetration | Medium (requires digital infrastructure and public acceptance) |
Impact of Delays and Capacity Constraints
The effectiveness of any prioritization strategy is heavily influenced by system delays and capacity constraints. Research demonstrates that contact tracing efficacy decreases sharply with increasing delays between symptom onset and tracing initiation, as well as with lower fractions of symptomatic infections being tested [67]. The relationship between tracing capacity and disease transmission follows a nonlinear pattern, where the fraction of contacts successfully traced directly impacts the pathogen reproductive number.
Table 2: Impact of System Parameters on Contact Tracing Efficacy
| System Parameter | Impact on Tracing Efficacy | Threshold Effects | Data Source |
|---|---|---|---|
| Time to Tracing | Each day of delay reduces efficacy by approximately 20-30%; Tracing within 2 days of symptom onset critical | Delays >3 days render tracing minimally effective | Compartmental modeling [67] |
| Testing Coverage | Low symptomatic case testing (20-40%) limits maximum Rt reduction to ~20% | >60% testing coverage needed for maximal impact (60% Rt reduction) | Stochastic model simulation [67] |
| Tracer Capacity | Rt increases sigmoidally as cases exceed capacity; Mobile/expandable teams prevent overload | Maintain >20% capacity buffer for surge response | Deterministic and stochastic models [67] |
| Cluster Targeting | Precision of 34.6% for identifying true transmission events | Phylogenetic validation improves resource allocation | Phylogenetic pipeline analysis [8] |
Experimental Protocols for Strategy Validation
Phylogenetic Validation of Contact Tracing Precision
Genomic analysis provides a robust methodology for validating contact tracing precision by determining whether epidemiologically-linked cases represent genuine transmission events. This approach was effectively implemented in a study of SARS-CoV-2 transmission among university students, analyzing 459 case-contact pairs identified through contact tracing [8].
Experimental Workflow:
Case-Contact Pair Identification: Conduct traditional contact tracing to identify individuals exposed to confirmed index cases, documenting the nature, duration, and timing of contacts.
Sample Collection and Sequencing: Collect respiratory samples from confirmed cases and perform whole-genome sequencing of SARS-CoV-2 using high-throughput platforms.
Genomic Data Processing: Process raw sequencing data through a bioinformatics pipeline including quality control, genome assembly, and variant calling to identify single nucleotide polymorphisms (SNPs).
Phylogenetic Analysis: Construct time-scaled phylogenetic trees using maximum likelihood or Bayesian methods to visualize evolutionary relationships between viral sequences.
Transmission Pair Validation: Assess whether case-contact pairs cluster together within the phylogeny with minimal evolutionary distance, suggesting a direct transmission link.
Precision Calculation: Compute precision metrics as the proportion of epidemiologically-identified pairs not contradicted by genomic evidence.
This methodology achieved a precision of 34.6%, meaning approximately one-third of contact tracing-identified pairs were phylogenetically supported [8]. When analysis was restricted to these validated pairs, researchers could estimate serial intervals with reduced standard deviation, enhancing understanding of transmission dynamics.
Figure 1: Workflow for phylogenetic validation of contact tracing precision, illustrating the process from case identification to resource allocation optimization.
Branching Bandit Model for Prioritization
The branching bandit model, adapted from operations research, provides a mathematical framework for determining provably optimal prioritization policies in contact tracing. This model formalizes the trade-offs inherent in investigating known contacts versus discovering new potential contacts through investigation [68].
Experimental Implementation:
Problem Formulation: Model the contact tracing process as a branching bandit where each contact represents an "arm" with unknown infection status.
Parameter Estimation: Estimate key parameters including:
- Probability of infection for each contact
- Expected number of secondary contacts if infected
- Time required to investigate each contact
- Transmission risk based on individual characteristics and exposure context
Index Policy Calculation: Compute Gittins indices for each contact, which represent the priority score balancing both immediate reward (identifying an infected individual) and future value (access to their contacts).
Policy Implementation: Investigate contacts in descending order of their indices, updating priorities as new information emerges during the investigation process.
Validation: Compare the performance of the branching bandit policy against alternative strategies (e.g., FIFO, random, highest-risk-first) using simulation based on historical outbreak data.
This approach provides qualitative insights into prioritization trade-offs, demonstrating that optimal policies sometimes prioritize contacts with moderate infection probability but high social connectivity over contacts with high infection probability but limited connectivity [68].
Essential Research Reagent Solutions
Implementing and evaluating contact tracing prioritization strategies requires specific methodological tools and frameworks. The table below outlines key "research reagents" - essential methodological components for conducting robust studies in this field.
Table 3: Essential Research Methodologies for Contact Tracing Prioritization Studies
| Methodology Category | Specific Techniques | Primary Research Application | Implementation Considerations |
|---|---|---|---|
| Mathematical Modeling [68] [67] | Branching bandit models; Compartmental SEIR models; Stochastic simulations | Theoretical evaluation of prioritization policies; Projecting intervention impact under constraints | Requires operations research expertise; Parameter sensitivity analysis critical |
| Genomic Epidemiology [8] | Whole-genome sequencing; Phylogenetic analysis; SNP variant calling | Validation of transmission links; Precision assessment of tracing methods | Computational bioinformatics capacity; Sample quality requirements |
| Digital Infrastructure [11] | Bluetooth-based exposure notification; GPS contact logging; Automated follow-up systems | Scaling tracing capacity; Reducing time-to-notification | Privacy preservation mechanisms; Equity of access across populations |
| Field Investigation Protocols [11] [69] | Backward tracing interviews; Cluster detection algorithms; Setting-specific risk assessment | Real-world implementation of prioritization; Adaptation to local transmission patterns | Staff training requirements; Cultural competence in interviewing |
Discussion: Integration into Outbreak Response
Successful integration of prioritization strategies during high case loads requires balancing three critical elements: speed of investigation, comprehensive contact capture, and accuracy of transmission assessment [11]. Countries that effectively managed COVID-19 contact tracing, including Japan, Thailand, Singapore, and Vietnam, implemented adaptable systems that maintained this balance while responding to local transmission patterns [11].
The operationalization of these strategies depends on creating flexible surge capacity systems. This includes maintaining expandable or mobile contact tracer teams that can be deployed to areas with intermediate case burdens, where they achieve maximum impact in reducing transmission [67]. This approach avoids the diminishing returns encountered when deploying limited resources to areas with either very high or very low transmission intensity.
Future research should focus on developing standardized metrics for comparing prioritization strategies across different outbreak contexts and infectious diseases. Additionally, more intervention studies are needed to evaluate the real-world impact of these strategies on disease incidence and mortality, particularly in resource-limited settings [69]. As contact tracing continues to evolve as a public health tool, the integration of prioritization frameworks will remain essential for maximizing effectiveness during the high case loads that characterize epidemic peaks.
Balancing Speed, Accuracy, and Coverage in Tracing Operations
Tracing operations, a cornerstone of public health response to infectious diseases, aim to reconstruct transmission chains to contain outbreaks. The core challenge lies in optimizing the interdependent, and often competing, dimensions of speed, accuracy, and coverage. In the context of validating transmission clusters, the chosen tracing strategy directly influences the reliability and timeliness of epidemiological insights. This guide provides a comparative analysis of major tracing methodologies, evaluating their performance in balancing these critical parameters to support robust cluster validation.
Comparative Analysis of Tracing Methodologies
Different tracing methodologies offer distinct trade-offs. The table below provides a high-level comparison of three common approaches.
Table 1: High-Level Comparison of Contact Tracing Methodologies
| Tracing Methodology | Optimal Use Case | Relative Speed | Relative Accuracy | Relative Coverage | Key Limitations |
|---|---|---|---|---|---|
| Digital Proximity Tracing | Large-scale, rapid notification in communities with high smartphone penetration [1] | High | Medium (Can't determine context or distance with perfect fidelity) | Variable (Depends on technology adoption) | Limited contextual data; privacy concerns; digital divide [1] |
| Traditional Interview-Based Tracing | Complex outbreaks requiring detailed contextual and behavioral data [1] | Low (Resource-intensive and time-consuming) | High (Can gather rich data on contact type, duration, and setting) | Can be high, but requires massive workforce [1] | Slow for large outbreaks; recall bias; intensive human resources [1] |
| Molecular/Phylogenetic Cluster Identification | Understanding broad transmission patterns, viral dynamics, and links between cases [31] [70] | Low (Time needed for sequencing and complex analysis) | High for establishing links, low for real-time contacts | Dependent on sampling comprehensiveness | Not real-time; identifies genetic links but not necessarily direct transmission [31] |
Experimental Comparison: Estimating Effective Reproduction Number (Rt)
A key application of tracing data is the estimation of the effective reproduction number (Rt). A 2025 study compared a novel network-based method against a established statistical method (Cori's method), using detailed COVID-19 transmission data from South Korea [70]. The following table summarizes the quantitative findings from this experimental comparison.
Table 2: Experimental Performance in Estimating Rt During Different Outbreak Phases [70]
| Outbreak Phase | Network-Based Empirical Rt | Cori's Method Rt | Performance Interpretation |
|---|---|---|---|
| Low Case Numbers (Early Pandemic) | Remained near 1.0 | Near 1.0 | Both methods performed similarly during periods of limited, stable transmission. |
| Superspreading Events | Showed sharper, higher peaks | Showed muted, lower peaks | The network-based method demonstrated superior speed and accuracy in capturing sudden, intense bursts of transmission, a key feature of superspreading. |
| Emergence of Delta Variant | Converged with Cori's estimates | Converged with network-based estimates | During widespread, homogeneous transmission, the coverage of both methods became equivalent, and their estimates aligned. |
Experimental Protocol: Network-Based RtEstimation
Objective: To empirically estimate the effective reproduction number (Rt) by directly reconstructing infection networks from contact tracing data [70].
Materials:
- Line-listed case data, including demographics, diagnosis date, and symptom onset.
- Reliably documented infector-infectee pairs from contact tracing.
Methodology:
- Data Acquisition: Secure a dataset of confirmed cases with documented transmission links. The referenced study used data from the Korea Disease Control and Prevention Agency (KDCA) from 2020-2021 [70].
- Network Construction: Represent each infected individual as a node in a directed network. Create a directed edge from each infector node to their infectee node(s) based on the contact tracing data [70].
- Stratification (Optional): For granular analysis, stratify the network by attributes such as age group or geographic region [70].
- Empirical Rt Calculation: For a given time t, identify all individuals (nodes) who were reported as infected at time t. The empirical Rt is calculated as the average number of outgoing edges (secondary infections) generated by this cohort of infectors within the network [70].
This workflow contrasts with model-dependent methods like Cori's, which estimate Rt indirectly from aggregated case incidence and assumptions about the serial interval [70].
Diagram 1: Network-based Rt Estimation Workflow
The Validation Challenge in Phylogenetic Clustering
Phylogenetic analysis uses viral genome sequences to infer transmission clusters. However, a 2024 study highlighted significant limitations in existing phylogeny-based cluster identification tools. When evaluated on simulated clusters with dynamic transmission behavior, these tools exhibited low combined sensitivity and specificity and were unable to describe the internal transmission dynamics of an identified cluster [31]. This underscores a critical accuracy gap, showing that genetic similarity alone may not suffice for robust cluster validation.
Diagram 2: Phylogenetic Cluster Analysis & Validation
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Tracing and Cluster Validation Studies
| Reagent/Material | Function in Tracing Research |
|---|---|
| Line-Listed Case Data | The foundational dataset containing individual case information (e.g., diagnosis date, demographics, symptom onset) for basic epidemiological analysis and network node creation [70]. |
| Documented Infector-Infectee Pairs | The crucial reagent for constructing empirical infection networks, serving as the verified edges between nodes for direct calculation of transmission metrics [70]. |
| Viral Genomic Sequences | Raw material for phylogenetic analysis to understand genetic relatedness between cases and infer large-scale transmission patterns and clusters [31]. |
| Contact Setting Metadata | Data categorizing contacts (e.g., household, work, social) enabling analysis of transmission heterogeneity and risk in different environments, vital for assessing coverage bias [71]. |
| Spatiotemporal Mobility Data | Information on population movement over time and space, used to model and predict transmission spread and evaluate the coverage of tracing efforts against actual contact patterns [71] [70]. |
The pursuit of validated transmission clusters forces a strategic trade-off. Network-based approaches, built on direct infector-infectee pairs, offer a powerful balance, providing high speed and accuracy for capturing real-time dynamics and superspreading events, as evidenced by superior Rt estimation performance [70]. In contrast, phylogenetic methods, while accurate for establishing genetic links, are slow and exhibit significant limitations for identifying dynamically transmitted clusters [31]. Traditional interviewing provides deep, accurate data but is inherently slow and difficult to scale, limiting its coverage in large outbreaks [1]. The optimal strategy for cluster validation is context-dependent, but integrating rapid digital tools with targeted, in-depth interview or sequencing data for investigation of key clusters presents a promising path to harmonize speed, accuracy, and coverage.
Contact tracing, a cornerstone of public health interventions for infectious diseases, is not a one-size-fits-all strategy. Its effectiveness is highly dependent on the specific epidemiological context, available resources, and societal compliance. The concept of adaptive approaches or scenario-based strategy switching refers to the systematic adjustment of contact tracing methods in response to changing outbreak conditions, transmission patterns, and operational constraints. This paradigm shift from static to dynamic intervention strategies allows public health authorities to optimize resource allocation and effectiveness while minimizing societal disruption.
Emerging evidence suggests that the precision of contact tracing varies significantly across different scenarios. A phylogenetic validation study of COVID-19 contact tracing in Belgium found that only 34.6% of transmission events suggested by contact tracing were not invalidated by combined phylogenetic and single nucleotide polymorphism analysis [6]. This highlights the critical need for strategy refinement based on empirical validation rather than assumed effectiveness.
Furthermore, a comprehensive systematic literature review of contact tracing strategies emphasized that "effective contact tracing requires robust health systems governance, adequate resources, and community involvement," and noted that effectiveness "varied across diseases and contexts" [1]. This contextual dependency fundamentally supports the adoption of adaptive approaches that can respond to changing scenarios.
Comparative Effectiveness of Contact Tracing Strategies
Strategy Classifications and Performance Metrics
Contact tracing strategies can be categorized along several dimensions: comprehensiveness of contacts traced, technological approach (manual vs. digital), and integration with other public health measures. The effectiveness of these strategies is typically measured through metrics such as reduction in effective reproduction number (R), proportion of contacts successfully traced and quarantined, speed of tracing, and ultimately, reduction in disease incidence and mortality.
Table 1: Classification of Contact Tracing Strategies by Comprehensiveness
| Strategy Type | Contacts Traced | Implementation Complexity | Resource Requirements |
|---|---|---|---|
| Family-Only Tracing | Household members | Low | Low |
| Work/School Tracing | Family + workplace/school contacts | Medium | Medium |
| Social Circle Tracing | Family + work + social/leisure contacts | High | High |
| Complete Digital Tracing | All potential contacts | Very High | Very High |
Scenario-Dependent Effectiveness
The performance of different contact tracing strategies varies dramatically depending on the transmission context. An agent-based modeling study simulating COVID-19 spread in a municipality of approximately 60,000 inhabitants revealed crucial scenario-dependent effectiveness [72]:
- Under strict contact restrictions: Only minimal differences were observed among the four contact tracing strategies, suggesting that in lockdown scenarios, even basic tracing provides sufficient coverage.
- In relaxed environments with few contact restrictions: The effectiveness of different tracing strategies diverged substantially, with more comprehensive approaches outperforming limited ones.
- In the presence of superspreader events: Only complete contact tracing demonstrated the capability to stop epidemic growth, highlighting the necessity of comprehensive approaches in high-risk scenarios.
This research conclusively demonstrates that "in situations, where many other non-pharmaceutical interventions are in place, the specific extent of contact tracing may not have a large influence on their effectiveness. In a more relaxed setting with few contact restrictions and larger events the effectiveness of contact tracing depends heavily on their extent" [72].
Experimental Validation and Methodologies
Phylogenetic Validation Framework
A novel methodology for assessing contact tracing precision combines genomic surveillance with traditional epidemiological investigation [6]. The experimental protocol involves:
- Case-Contact Pair Identification: Collecting data on 459 case-contact pairs identified through conventional contact tracing.
- Genomic Sequencing: Conducting whole-genome sequencing of SARS-CoV-2 samples from identified pairs.
- Phylogenetic Analysis: Placing case-contact pairs within time-scaled phylogenies to validate transmission links.
- Precision Calculation: Determining the proportion of suggested transmission events not contradicted by genomic evidence.
This approach provides an objective measure of contact tracing precision, enabling validation of different strategies under real-world conditions. The finding that only approximately one-third of epidemiologically linked pairs were genetically plausible underscores the need for improved strategies and validation mechanisms [6].
Agent-Based Simulation Methodology
The agent-based modeling approach used to evaluate contact tracing strategies provides a robust experimental framework for scenario-based testing [72]:
- Population Construction: Creating a synthetic population of approximately 60,000 inhabitants (nodes) with about 2.8 million social contacts (edges) across 30 different layers reflecting demographic, geographic, and sociological patterns.
- Network Layer Definition: Incorporating real data from census, land registers, transport data, and shopping behavior to create realistic contact networks including households, workplaces, schools, and leisure activities.
- Disease Modeling: Implementing a modified SEIR model with finer resolution of pre-symptomatic, asymptomatic, and detected states, calibrated on real outbreak data.
- Intervention Simulation: Testing four distinct tracing strategies across multiple transmission environments with varying restriction levels.
This methodology allows for the controlled evaluation of strategy switching based on changing epidemic conditions, providing evidence-based guidance for scenario-adaptive approaches.
Table 2: Key Performance Indicators Across Contact Tracing Strategies
| Strategy | Reduction in R | Proportion of Contacts Quarantined | Speed of Implementation | Optimal Scenario |
|---|---|---|---|---|
| Manual with High Coverage | 10-15% [73] | High | Slow | Low transmission periods |
| Hybrid Manual-Digital | 10-15% [10] | Medium | Medium | Reopening phases |
| Digital Proximity Tracing | Varies by policy [74] | Adjustable via thresholds | Fast | High-transmission scenarios |
| Backward/Bidirectional Tracing | Higher than forward alone [10] | Medium-Fast | Medium | Clustered outbreaks |
Signaling Pathways for Strategic Decision-Making
The decision to switch between contact tracing strategies should follow evidence-based pathways triggered by specific epidemiological, operational, and social indicators. The conceptual framework for adaptive strategy switching can be visualized as follows:
This decision pathway emphasizes the continuous monitoring of multiple indicator types to trigger appropriate strategy switches. The systematic review by Guy et al. emphasizes that "effective contact tracing requires robust health systems governance, adequate resources, and community involvement," highlighting the multidimensional nature of these decisions [1].
The Researcher's Toolkit: Essential Methods and Reagents
Implementing and evaluating adaptive contact tracing strategies requires specific methodological approaches and analytical tools. The following table outlines key components of the research toolkit for scenario-based strategy switching:
Table 3: Research Reagent Solutions for Contact Tracing Evaluation
| Tool/Method | Function | Application Context |
|---|---|---|
| Phylogenetic Analysis | Validates transmission links through genomic sequencing | Precision assessment of contact tracing programs [6] |
| Agent-Based Modeling | Simulates disease spread and intervention impacts | Strategy comparison across scenarios [72] |
| Multi-Layer Network Models | Represents diverse social contact types | Realistic simulation of transmission dynamics [72] [74] |
| Digital Proximity Sensing | Detects potential exposure events | Digital contact tracing implementation [74] |
| Serial Interval Estimation | Measures time between symptom onsets | Tracing effectiveness assessment [6] |
Implementation Considerations and Barriers
Critical Success Factors
Successful implementation of adaptive contact tracing strategies depends on several key factors identified across multiple studies:
- Population Adherence: A UK modeling study found that "reporting and adherence are the most important predictors of programme impact," with poor adherence potentially eliminating any benefit from contact tracing [73]. The reduction in R through contact tracing ranged from 2-5% with poor adherence to 10-15% with good adherence and high coverage.
- Operational Speed: Delays in testing and tracing significantly diminish effectiveness. Research indicates that "eliminating contact tracing delays" was identified as a highly effective policy in mathematical modeling studies [10].
- Integration with Other Measures: Contact tracing functions best as part of a comprehensive public health response rather than a standalone intervention. As noted in one study, "contact tracing is not currently appropriate as the sole control measure" [73].
Ethical and Privacy Considerations
Adaptive approaches, particularly those involving digital tools, must address important ethical considerations around privacy, equity, and data protection. The systematic review by Guy et al. emphasized the need to balance public health protection with individual rights and privacy [1]. Concerns about "stigma and public trust may affect the adherence to contact tracing," highlighting the importance of community engagement and transparent communication about strategy switches [1].
The evidence comprehensively supports the adoption of scenario-based strategy switching in contact tracing programs. Rather than maintaining static approaches, public health authorities should implement adaptive frameworks that respond to changing epidemiological conditions, operational capacities, and societal contexts.
Key principles for implementing adaptive approaches include:
- Continuous Monitoring: Establish robust surveillance systems to trigger strategy switches at appropriate thresholds.
- Precision Validation: Incorporate phylogenetic methods to validate and refine contact tracing precision.
- Hybrid Implementation: Combine manual and digital approaches to leverage the strengths of each method.
- Community-Centered Design: Maintain public trust and adherence through transparent communication and inclusive planning.
As the field advances, the integration of real-time genomic surveillance, digital tools, and traditional epidemiology will enable increasingly precise and adaptive contact tracing strategies. This evolution toward precision public health promises more effective outbreak control while minimizing societal and economic disruption.
Within the framework of validating disease transmission clusters through contact tracing research, a critical but often undervalued finding emerges: the profound influence of community trust and stigma on data accuracy and intervention compliance. Traditional models of outbreak investigation, which focus on algorithmic analysis of contact networks [75], can be significantly hampered if fear and discrimination prevent individuals from coming forward for testing or disclosing their contacts. This guide compares different methodological approaches to community engagement, framing them as essential, comparable protocols whose "performance" directly impacts the completeness of transmission data and the ultimate success of public health interventions.
Methodological Comparison: Engagement Protocols as Experimental Designs
The following table summarizes the core components and comparative applications of three distinct community engagement strategies derived from public health and implementation science research.
Table 1: Comparison of Community Engagement Methodological Approaches
| Methodology | Core Protocol / Workflow | Primary Application Context | Key Performance Metrics | Inherent Challenges |
|---|---|---|---|---|
| Transmission Cluster Analysis [75] [76] | 1. Horizontal Edge Creation: Link co-primary cases.2. Vertical Edge Consolidation: Establish parent-child transmission links.3. Graph Reduction: Simplify the network for analysis. | Investigating infectious disease outbreaks (e.g., COVID-19) to understand spread dynamics and identify super-spreading events [76]. | - Number of clusters identified- Average cluster size and duration- Maximum generations of transmission [76]- Network diffusion metrics [75] | Relies on complete and accurate contact data, which can be compromised by stigma and low community trust. |
| Stigma Assessment & Strategy Development [77] | Phase 1 (Quantitative): Cross-sectional surveys to quantify stigma experiences.Phase 2 (Qualitative): In-depth interviews and focus groups to explore determinants.Phase 3 (Synthesis): Develop culturally-sensitive strategies using literature review and expert consensus (e.g., Nominal Group Technique). | Reducing addiction-related stigma and discrimination in healthcare settings, particularly Public Addiction Treatment Centers (PATCs) [77]. | - Levels of reported stigma and discrimination- Identified predictors of stigma- Acceptability and feasibility of developed strategies [77] | Requires significant time commitment; recruiting and retaining participants with lived experience can be challenging [77]. |
| Iterative Community Engagement (EASY OPS) [78] | 1. Iterative Feedback Loops: Sequential use of interviews, surveys, and focus groups with people with lived experience (PWLE).2. Environmental Assessment: "Walking interviews" to identify micro-scale barriers.3. Research-Mediated Adaptation: Research team facilitates collaboration between PWLE and implementers. | Tailoring the implementation of evidence-based harm reduction programs (e.g., vending machines for naloxone distribution) to community-specific needs [78]. | - Program uptake and utilization rates- Identification of environmental access barriers- Diversity of community perspectives incorporated [78] | Managing fluid participation due to social/legal instability of participants; requires adaptable research timelines [78]. |
Experimental Protocols and Data Outcomes
Protocol 1: Mining Relationships in Transmission Clusters
This protocol, as applied in COVID-19 research, involves constructing transmission cascades from contact tracing data. The algorithmic process includes horizontal edge creation (linking co-primary cases), vertical edge consolidation (establishing generational links), and graph reduction [75]. The resulting networks are analyzed using information diffusion metrics and exponential-family random graph modeling. A key performance outcome from a Senegalese study identified 2,153 transmission clusters with an average of 29.58 members, 7.63 infected individuals, and an average duration of 27.95 days [76]. This method's effectiveness is contingent on the initial data quality from contact tracing, which is vulnerable to stigma.
Protocol 2: Mixed-Methods Stigma Reduction Strategy Development
This structured approach generates culturally-attuned strategies to combat stigma [77].
- Phase 1 (Quantitative Survey): A cluster sampling technique is used to recruit a large sample (e.g., n=360) of individuals with substance use disorders (SUDs) to assess their experiences of stigma and identify predictive factors.
- Phase 2 (Qualitative Exploration): Purposive sampling is used to select participants from Phase 1 for in-depth semi-structured interviews and focus groups. This explores the aspects and determinants of stigma from the perspectives of both people with SUDs and healthcare providers. Data are analyzed using conventional content analysis.
- Phase 3 (Strategy Development): Findings from the first two phases are combined with a literature review and expert opinions gathered via the Nominal Group Technique to formulate practical, cultural-based strategies [77].
Protocol 3: The EASY OPS Iterative Engagement Process
This novel protocol addresses two key challenges: environmental barriers to access and difficulties in sustaining diverse community engagement [78]. The process involves:
- Recruitment: Convenience and snowball sampling of PWLE from organizations providing substance use services.
- Iterative Feedback: Conducting successive rounds of data collection (interviews, focus groups) with unique PWLE to provide timely, diverse input without relying on long-term commitment from the same individuals.
- Environmental Walking Interviews: Participants guide researchers through the environment where services are (or will be) located, identifying micro-scale features that encourage or deter use (e.g., lighting, security presence, privacy).
- Mediated Collaboration: The research team continuously synthesizes feedback from PWLE and collaborates with the implementation team to adapt the program, creating a sustainable feedback loop for program improvement [78].
Quantitative Outcomes in Comparative Focus
The performance of these methodologies can be quantified, allowing for objective comparison of their outputs and effectiveness.
Table 2: Comparative Quantitative Outcomes from Applied Research
| Metric | Transmission Cluster Analysis (COVID-19 in Senegal) [76] | Stigma & Engagement Interventions |
|---|---|---|
| Sample/Cluster Scale | 114,040 samples tested; 2,153 clusters identified [76]. | Mixed-methods stigma research often involves hundreds of survey participants and dozens of qualitative interviews [77]. |
| Key Output Measures | - Average of 7.63 infected members per cluster.- Maximum of 7 generations of secondary infection.- 19.68% of infected individuals were asymptomatic [76]. | Iterative engagement (EASY OPS) tailors programs by identifying specific environmental barriers (e.g., security guard presence as a deterrent) [78]. |
| Correlational Findings | A significant positive correlation (P = 4.3e-07) was found between the proportion of asymptomatic individuals in a cluster and its transmission degree (size/generations), highlighting a key driver of spread [76]. | Stigma is correlated with detrimental health outcomes, including delayed care, poor mental health, and non-compliance with treatment [77]. |
Research Reagent Solutions: A Toolkit for Engagement and Analysis
Just as a laboratory requires specific reagents, effective research at the nexus of transmission dynamics and community engagement requires a toolkit of validated instruments and methodologies.
Table 3: Essential Research Reagents and Methodologies for Stigma-Informed Cluster Analysis
| Research 'Reagent' / Tool | Function & Application |
|---|---|
| Cross-Sectional Survey with Validated Stigma Scales | Quantifies the prevalence and predictors of stigma experiences among a target population, providing baseline data for intervention design [77]. |
| Semi-Structured Interview & Focus Group Guides | Explores the nuanced, lived experiences of stigma and trust-breaking events, generating rich qualitative data on barriers and potential solutions [77]. |
| Network Analysis & Graph Reduction Algorithms | Processes complex contact tracing data to construct, visualize, and analyze transmission clusters, identifying key nodes (super-spreaders) and network properties [75]. |
| Nominal Group Technique | A structured, consensus-building method used in the strategy development phase to integrate quantitative findings, qualitative themes, and expert opinion into actionable plans [77]. |
| Environmental Assessment ('Walking Interview') | Identifies micro-scale features of the physical environment (e.g., privacy, safety) that act as barriers or facilitators to service access and utilization [78]. |
| Iterative Engagement Framework (EASY OPS) | A flexible protocol that supports fluid participation, allowing for the incorporation of diverse perspectives from PWLE throughout the research and implementation lifecycle [78]. |
Visualizing the Integrated Workflow: From Stigma to Incomplete Data
The logical relationship between community stigma, incomplete contact tracing data, and biased transmission cluster analysis is outlined in the workflow below.
Integrated Workflow of Stigma and Engagement Impact
The comparative analysis presented in this guide demonstrates that methodologies for community engagement are not merely "soft" supplements to epidemiological science but are rigorous protocols with quantifiable performance metrics. The data clearly show that approaches like the EASY OPS iterative model and mixed-methods stigma assessment directly address the critical point of failure in transmission cluster validation: the quality and completeness of primary data. For researchers and drug development professionals, the conclusion is inescapable. Integrating robust, scientifically-sound community engagement and stigma reduction protocols is not an optional adjunct to contact tracing research but a fundamental component of validating transmission models and ensuring the success of subsequent interventions.
Measuring Success: Validation Frameworks and Comparative Effectiveness
In molecular epidemiology, establishing concordance between epidemiological and molecular data is fundamental for validating inferred transmission clusters. This process determines whether relationships suggested by field investigations (source, time, location) align with genetic relatedness identified in the laboratory. High concordance strengthens the evidence for true transmission links, directly impacting the effectiveness of contact tracing research and public health interventions [79] [80].
As molecular technologies evolve from traditional typing to whole-genome sequencing (WGS), the framework for validation也必须 adapt. This guide provides a structured comparison of methods and metrics used to quantify this critical concordance, offering researchers a practical toolkit for robust cluster validation.
Fundamental Concepts and Definitions
Key Terminology
- Concordance: The degree of agreement between a molecular cluster of related isolates and a cohesive epidemiological group sharing common characteristics (e.g., source, time, geography) [79].
- Epidemiological Data: Information describing the context of pathogen sampling, typically including temporal (collection date), spatial (geographic location, GPS), and source (host, environment) metadata [79].
- Molecular Data: Genetic information used to differentiate pathogen isolates, ranging from band-based methods (PFGE) to sequence-based methods like Multi-Locus Sequence Typing (MLST), Single Nucleotide Polymorphism (SNP) calling, and Whole-Genome Sequencing (WGS) [81] [82].
- Cluster Validation: The procedure of evaluating the goodness of a clustering result, which can be internal (using internal information of the clustering process), external (comparing results to an externally known result, such as class labels), or relative (evaluating the structure by varying algorithm parameters) [83] [84].
The Concordance Workflow
The process of assessing concordance involves a structured comparison of independent data types, as illustrated below.
Methodologies for Quantifying Concordance
The EpiQuant Framework: A Metric-Based Model
The EpiQuant framework provides a quantitative model for computing the pairwise epidemiological distance (Δε) between bacterial isolates using basic sample metadata [79].
- Model Equation: The total epidemiological distance is calculated as: Δε = (γ × ΔGPS) + (τ × ΔTime) + (σ × ΔSource) where ΔGPS, ΔTime, and ΔSource represent normalized differences in geography, collection time, and source, respectively. The coefficients γ, τ, and σ are weights (e.g., 20%, 30%, 50%) that can be adjusted based on a priori epidemiological considerations for a specific pathogen [79].
- Source Similarity Rubric: A key innovation is the rubric for comparing sampling sources. Each source is described by a profile of ~25 epidemiological attributes related to the pathogen's transmission chain (e.g., "UrbanCompanionAnimal," "FarmFoodAnimal"). The pairwise source similarity is calculated as the proportion of matching attributes [79].
- Application: The resulting Δε matrix can be clustered, and the clusters are treated as the epidemiological hypothesis. The concordance with molecular clustering is then measured using external validation indices like the Corrected Rand Index or Meila's VI [79] [83].
Statistical and Clustering Validation Indices
To quantitatively compare epidemiological and molecular cluster assignments, researchers employ specific validation statistics.
Table 1: Key Cluster Validation Indices for Measuring Concordance
| Index Name | Type | Interpretation | Optimal Value | Primary Use Case |
|---|---|---|---|---|
| Corrected Rand Index (CRI) | External | Measures agreement between two partitions, corrected for chance [83]. | +1 (Perfect Agreement) | Overall concordance between epidemiological and molecular clusters [83]. |
| Meila's Variation of Information (VI) | External | Measures the distance between two clusterings based on information theory [83]. | 0 (Perfect Agreement) | Overall concordance between epidemiological and molecular clusters [83]. |
| Silhouette Width | Internal | Measures how well an observation fits its own cluster compared to the nearest neighboring cluster [83] [84]. | +1 (Well-clustered) | Validating cohesion and separation of molecular clusters before concordance check [83]. |
| Dunn Index | Internal | Ratio of the smallest inter-cluster distance to the largest intra-cluster distance [83]. | Maximize | Validating compact and well-separated molecular clusters [83]. |
Genomic Thresholds for Transmission Links
In WGS-based studies, concordance is often assessed by defining a genetic distance threshold below which isolates are considered genetically linked and then evaluating the epidemiological connection.
- Threshold Determination: A genetic linkage cut-off is established, for example, ≤80 SNPs for Klebsiella pneumoniae carbapenemase-producing K. pneumoniae (KPC-Kp) or ≤6 SNPs for Mycobacterium tuberculosis, often based on the observed distribution in a phylogenetic tree and known epidemiologically linked pairs [80].
- Precision Calculation: A genomic pipeline can assess the precision of contact tracing by calculating the proportion of epidemiologically suggested transmission events that are not invalidated by genomic analysis. One study of COVID-19 found this precision to be 34.6% [6].
- Trend Analysis: Concordance is demonstrated by a significant trend where isolates with a "High" epidemiological probability of transmission show a high proportion of genetic linkage (e.g., 84.2%), while those with "No" suspected transmission show a low proportion (e.g., 16.2%) [80].
Comparative Performance of Molecular Methods
The choice of molecular subtyping method significantly impacts the resolution of clusters and, consequently, the measured concordance with epidemiology.
Table 2: Comparison of Molecular Subtyping Methods for Concordance Studies
| Method | Typical Genetic Marker | Key Advantage | Key Limitation in High Diversity | Impact on Concordance Assessment |
|---|---|---|---|---|
| Whole-Genome Sequencing (WGS) | Genome-wide SNPs [80] [82] | Highest possible resolution for discriminating strains [82]. | High cost; complex data analysis. | Considered the gold standard; allows for precise SNP cut-offs for transmission [80]. |
| SNP Barcoding | 24-96 Biallelic SNPs [81] | Lower cost and simpler analysis than WGS. | Limited polymorphism; poor resolution in high-transmission, multiclonal settings [81]. | May overestimate isolate relatedness, reducing apparent concordance with detailed epidemiology [81]. |
| Microsatellite Genotyping | 10-12 Multiallelic loci [81] | Higher polymorphism than SNP barcodes. | Cannot phase haplotypes in multiclonal infections without complex computation [81]. | Provides a intermediate level of resolution, useful for population-level studies [81]. |
| var Gene Typing (Varcoding) | DBLα tags of var genes [81] | Exceptionally high polymorphism; handles multiclonal infections without phasing [81]. | Pathogen-specific (currently P. falciparum); reflects immune selection. | Effectively captures population diversity and structure in high-transmission settings [81]. |
A study comparing methods for Plasmodium falciparum surveillance in a high-transmission setting found that a 24-SNP barcode provided a view of higher isolate relatedness compared to microsatellites and varcoding, which better reflected the diverse population structure. This demonstrates that a method with insufficient resolution can distort the perceived concordance by failing to capture true population diversity [81].
Table 3: Key Research Reagent Solutions for Concordance Studies
| Item / Resource | Function / Application | Example / Note |
|---|---|---|
R fpc package |
Computing cluster validation statistics [83]. | The cluster.stats() function calculates Corrected Rand Index and Meila's VI. |
R factoextra & NbClust packages |
Clustering analysis and validation [83]. | Used for Silhouette analysis, Dunn Index, and determining optimal cluster number. |
| EpiQuant Framework (R) | Quantifying epidemiological similarity [79]. | Requires curated metadata with consistent granularity for source, time, location. |
| Phylogenetic Software (e.g., BEAST) | Inferring transmission trees and evolutionary rates [82]. | Used for time-scaled phylogenies to validate contact tracing pairs [6]. |
| SNP Calling Pipeline | Identifying genetic variants from WGS data [80] [82]. | Critical for defining genetic linkage based on SNP thresholds [80]. |
| Curated Metadata Database | Storing standardized epidemiological data [79]. | Essential for robust Δε calculations; e.g., the Canadian Campylobacter C3GFdb. |
Validating transmission clusters requires a multi-faceted approach that rigorously tests the agreement between field epidemiology and laboratory genomics. No single metric is sufficient. A robust validation strategy involves:
- Quantifying Epidemiology: Using frameworks like EpiQuant to move beyond qualitative assessments.
- Choosing a Resolution-Appropriate Molecular Method: Recognizing that WGS often provides the definitive standard, but other methods can be fit-for-purpose.
- Applying Relevant Validation Statistics: Using external indices like the Corrected Rand Index to measure agreement and internal indices to check the quality of the molecular clustering itself.
- Interpreting Genetic Thresholds in Context: Establishing and applying SNP cut-offs based on the specific pathogen and outbreak setting.
This integrated methodology ensures that inferences about transmission chains are statistically sound, ultimately leading to more effective and precisely targeted public health interventions.
This guide provides an objective comparison of different contact tracing strategies, evaluating their performance based on transmission reduction potential and cost-efficiency. The analysis is framed within the broader research objective of validating disease transmission clusters to inform public health policy and resource allocation.
Quantitative Comparison of Contact Tracing Strategies
The table below summarizes the performance of different contact tracing approaches and related interventions based on key effectiveness measures.
Table 1: Comparative Effectiveness of Contact Tracing and Related Interventions
| Strategy | Key Performance Metrics | Quantitative Findings | Primary Context / Model Type |
|---|---|---|---|
| Digital Contact Tracing (DCT) | Effective Reproduction Number (R~e~), Tracing Accuracy, Quarantine Rate | Can reduce R~e~ by ~50% with optimized policies (contacts >15-20 min, <2-3 meters); High compliance and low delay are critical [74]. | Empirical contact network models simulating Bluetooth-based app efficiency [74]. |
| Test-Trace-Isolate-Quarantine (TTIQ) | Detection Ratio, Tracing Delay, Overall Effectiveness | Effectiveness is highly dependent on capacity; Diminishes significantly during high prevalence due to testing/tracing delays and limited resources [85]. | Delay Differential Equation (DDE) models incorporating limited capacities and presymptomatic transmission [85]. |
| Combined Mass Testing & Contact Tracing | Effective Reproduction Number (R~e~), Required Testing Frequency | Adding effective contact tracing can prevent the same number of transmissions as doubling the mass testing frequency, optimizing resource use [86]. | Branching model with viral load trajectories for various respiratory viruses [86]. |
| Molecular Network Analysis | Cluster Detection Accuracy, Network Characteristics | Accurately identified 82.02% - 86.25% of known HIV-positive couples, providing objective cluster insights for targeted interventions [34]. | Phylogenetic analysis and molecular network construction from viral genetic sequences [34]. |
| Cost-Effectiveness Analysis (CEA) for Pharmaceuticals | Incremental Cost-Effectiveness Ratio (ICER), Population-Level Net Health Effects | Market-based cost-effectiveness ratios differ significantly from research studies; Reassessment frameworks are needed as treatments, evidence, and prices evolve [87] [88]. | Health Technology Assessment (HTA) framework for pricing and funding decisions in multi-comparator markets [87]. |
Experimental Protocols and Methodologies
This section details the core experimental and modeling methodologies used to generate the data compared in this guide.
Modeling Framework for Digital Contact Tracing on Empirical Networks
This protocol, based on [74], evaluates how DCT apps mitigate spread in real-world environments.
- Primary Objective: To quantify the impact of different DCT policies (e.g., varying contact duration and proximity thresholds) on epidemic control and the fraction of the population quarantined.
- Data Acquisition: Utilizes empirical, high-resolution contact data from specific social settings (e.g., a university campus, a workplace). The Copenhagen Networks Study (CNS) data set, which records Bluetooth-derived proximity between smartphones, is a key example.
- Model Simulation:
- Network-Based Tracing Simulation: The contact tracing procedure is simulated on the empirical contact network. For a given DCT policy (e.g., "quarantine contacts within 2 meters for more than 15 minutes"), the model calculates the tracing ability (ε~T~), defined as the proportion of an index case's future infections that are prevented by tracing and quarantining their contacts.
- Epidemiological Modeling: The calculated ε~T~ is inserted into a generalized version of the Fraser et al. model [74], expressed by the equation: $${\Lambda}(t,\tau) = {R}{0}\omega(\tau)\left(1-{\varepsilon}{I}s(\tau)\right)\mathop{\int}\limits{0}^{t-\tau}\left(1-{\varepsilon}{T}\frac{s(\rho + \tau)-s(\rho)}{1-s(\rho)}\right){\Lambda}(t-\tau,\rho)\mathrm{d}\rho$$ Here, Λ(t, τ) represents individuals infected at time t by individuals who have been infected for time τ; R₀ is the basic reproduction number; ω(τ) is infectiousness; and s(τ) is the probability of symptom onset.
- Outcome Measures: The model outputs the epidemic incidence λ(t) and the effective reproduction number R~e~ under the intervention. The "cost" is measured as the fraction of the population preventively quarantined.
Delay Differential Equation Model for TTIQ Under Limited Capacities
This protocol, derived from [85], assesses the effectiveness of integrated testing and tracing systems.
- Primary Objective: To understand how limited testing and tracing capacities reduce the effectiveness of TTIQ strategies as disease prevalence increases.
- Model Structure: A compartmental model is formulated using Delay Differential Equations (DDEs). The model explicitly incorporates:
- Time Delays: For testing (time from test to result) and tracing (time to identify and quarantine contacts).
- Presymptomatic Transmission: A key characteristic of diseases like COVID-19.
- State-Dependent Rates: Testing rates decrease as the number of symptomatic individuals exceeds available laboratory capacity.
- Simulation and Analysis:
- Numerical Experiments: The model is parameterized with data inspired by the early spread of COVID-19 in Germany.
- Stability and Sensitivity Analysis: Identifies key disease-dependent (e.g., incubation period) and disease-independent (e.g., compliance, capacity) factors that determine TTIQ success.
- Outcome Measures: The model tracks the effective reproduction number and the "detection ratio" (proportion of infectious individuals detected before recovery) over the course of an epidemic wave.
Molecular Network Analysis for HIV Transmission Clusters
This protocol, based on [34], uses viral genetics to objectively detect transmission clusters.
- Primary Objective: To identify clusters of HIV transmission by analyzing the genetic similarity of viral sequences and to inform targeted public health interventions.
- Sample and Data Collection: Blood samples are collected from confirmed HIV-positive individuals. General demographic data is also gathered.
- Genetic Sequencing and Analysis:
- Sequence Amplification: HIV-1 RNA is extracted from plasma, and the pol gene region is amplified and sequenced via RT-PCR and nPCR.
- Phylogenetic Tree Construction: Processed sequences are aligned, and a phylogenetic tree is built using maximum-likelihood methods (e.g., with FastTree software) alongside international reference sequences.
- Molecular Network Construction (Two Methods):
- Pairwise Gene Distance: Genetic distances between all sequence pairs are calculated (TN93 model). Pairs with a distance below a set threshold (e.g., 0.014 substitutions/site) are connected to form a network.
- Evolutionary Tree Joint Gene Distance: Molecular clusters are extracted from the phylogenetic tree using Cluster Picker, with a second genetic distance threshold (e.g., 0.045 substitutions/site) to define cluster membership.
- Outcome Validation: The accuracy of the methods is tested against a known dataset (e.g., 89 HIV-positive couples). The resulting networks are visualized using software like Cytoscape.
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential materials and tools used in the featured experiments for contact tracing and transmission cluster analysis.
Table 2: Key Research Reagents and Tools for Transmission Analysis
| Reagent / Tool | Function / Application | Field of Use |
|---|---|---|
| QIAmp Viral RNA Mini Kit | Extraction of HIV-1 RNA from patient plasma samples for subsequent genetic analysis [34]. | Molecular Biology / Virology |
| RT-PCR & nPCR Primers (e.g., MAW25, RT21, PRO-1, RT20) | Amplification of specific HIV-1 pol gene fragments for Sanger sequencing and phylogenetic analysis [34]. | Molecular Biology / Genetics |
| HYPHY 2.2.4 Software | Software package used for evolutionary genetic analyses, including calculating pairwise genetic distances between viral sequences [34]. | Computational Biology / Phylogenetics |
| Cytoscape | An open-source platform for visualizing complex molecular networks constructed from genetic linkage data [34]. | Data Visualization / Bioinformatics |
| FastTree 3.0 Software | A tool for inferring approximately-maximum-likelihood phylogenetic trees from genetic sequence alignments [34]. | Computational Biology / Phylogenetics |
| Empirical Contact Datasets (e.g., Copenhagen Networks Study) | High-resolution data on person-to-person contacts used to realistically simulate the spread of pathogens and the performance of contact tracing apps [74]. | Epidemiology / Network Science |
| Delay Differential Equation (DDE) Models | A class of mathematical models used to simulate epidemic dynamics and intervention effects, explicitly accounting for delays in testing and tracing processes [85]. | Mathematical Modeling / Epidemiology |
Contact tracing stands as a cornerstone public health intervention for breaking chains of transmission during infectious disease outbreaks. Within this field, specific methodologies have evolved to optimize resource allocation and effectiveness. This guide provides a comparative analysis of two distinct approaches: cluster tracing and forward tracing. Framed within the broader research context of validating transmission clusters, this analysis examines the performance, operational requirements, and ideal use cases for each method, providing researchers and public health professionals with evidence-based insights for outbreak response planning.
The performance of contact tracing is highly contextual, depending on factors such as case ascertainment rates, testing availability, and quarantine policies [9]. Understanding the comparative advantages of each method allows for the development of flexible response systems that can be adapted to specific outbreak dynamics and resource constraints.
Performance Data Comparison
The effectiveness of cluster and forward tracing has been quantified across various pandemic scenarios. The following tables summarize key performance metrics from modelling studies and empirical data.
Table 1: Comparative Effectiveness in Reducing Transmission (Modelling Data)
| Tracing Method | Low Case-Ascertainment with Testing | Low Case-Ascertainment with Quarantine | High Case-Ascertainment with Testing | High Case-Ascertainment with Quarantine |
|---|---|---|---|---|
| Cluster Tracing | 22% reduction | 62% reduction | 26% reduction | Equally effective (stopped transmission) |
| Forward Tracing | 12% reduction | 46% reduction | 20% reduction | Equally effective (stopped transmission) |
| Extended Tracing | ~17% reduction | 50% reduction | ~23% reduction | Equally effective (stopped transmission) |
Source: Adapted from [9]
Table 2: Empirical Efficiency Metrics from Cohort Studies
| Performance Metric | Standard Forward Tracing | Backward/Cluster-Enhanced Tracing | Study Context |
|---|---|---|---|
| Additional Cases Identified | Baseline | 42% more than standard forward tracing | COVID-19, University Cohort [2] |
| Positivity Rate of Contacts | Similar to symptomatic controls | Similar to contacts in standard window | COVID-19, University Cohort [2] |
| Resource Efficiency | Requires more tests and longer quarantine | Required fewer tests and shorter quarantine | COVID-19, University Cohort [2] |
| Overall Efficiency (U.S. Context) | Identified ≤1.65% of transmission (PCR) | N/A | Voluntary system with rapid antigen tests [23] |
Conceptual Workflow of Tracing Strategies
The diagram below illustrates the core operational logic and primary focus of forward and cluster tracing strategies within a transmission chain.
This diagram illustrates the fundamental difference in focus between the two strategies. Forward tracing (blue) operates downstream from a confirmed index case, aiming to identify and isolate individuals infected by the known case to prevent further spread. In contrast, cluster tracing (green) operates upstream and laterally, seeking to identify the source of infection and other sibling cases who were exposed at the same event or location, thereby containing an entire transmission cluster at once [2] [11].
Detailed Experimental Protocols
Modelling Study Protocol: Singapore's Comparative Framework
A key modelling study provided a direct comparison of tracing methods using Singapore's population structure and COVID-19 characteristics [9].
- Objective: To assess the effectiveness and provider costs of forward, extended, and cluster tracing methods under varied pandemic scenarios.
- Model Design: A transmission network model was built using Singapore's contact tracing data and COVID-19 disease characteristics.
- Interventions Defined:
- Forward Tracing: Identified contacts exposed to the index case starting from 2 days before case isolation.
- Extended Tracing: Covered a longer period, starting 16 days before case isolation.
- Cluster Tracing: Combined forward tracing with active cluster identification and investigation.
- Scenario Testing: The model constructed combinations of scenarios to replicate variability during a pandemic, including low vs. high case-ascertainment and testing of contacts vs. quarantine of contacts.
- Outcome Measures: The impact on disease transmission (reduction in reproduction number) and provider costs (US dollars per infection prevented) were examined.
Empirical Cohort Study Protocol: Backward Contact Tracing Efficiency
An empirical cohort study demonstrated the real-world efficiency of backward-looking tracing strategies, which form the basis of cluster investigations [2].
- Objective: To determine the positivity rate and efficiency of contacts identified through an extended contact tracing window.
- Study Design & Population: A cohort study within a university test-and-trace programme from February to May 2021.
- Intervention: The contact tracing window was extended to start 7 days before symptom onset or diagnosis of the index case, instead of the standard 2 days.
- Comparison: Contacts identified in the extended window ("backward traced") were compared to those identified in the standard window and a control group of symptomatic individuals.
- Data Collection: Data included index case characteristics, number and type of contacts identified, and RT-qPCR test results for all contacts.
- Outcome Measures: The primary metric was the positivity rate (PR) among traced contacts. Secondary metrics included the number of additional cases identified and resource use (tests and quarantine days).
The Scientist's Toolkit: Research Reagent Solutions
Successful contact tracing research and implementation relies on a combination of methodological, technological, and analytical tools.
Table 3: Essential Reagents and Tools for Contact Tracing Research
| Tool / Solution | Category | Primary Function | Example/Note |
|---|---|---|---|
| Transmission Network Models | Modelling Framework | Simulate disease spread and evaluate intervention impact. | Used with country-specific contact data [9]. |
| Branching Process & Agent-Based Models | Modelling Framework | Model individual transmission events and heterogeneous contact patterns. | Realistically represents superspreading [89]. |
| Small-World Network Models | Modelling Framework | Incorporate characteristics of real-world social networks. | Avoids underestimation by deterministic models [90]. |
| Digital Proximity Tracking | Operational Technology | Anonymously register close contacts via smartphone. | Bluetooth-based apps (e.g., Immuni, TraceTogether) [11] [91]. |
| PCR Testing | Diagnostic Tool | High-sensitivity confirmation of infection in symptomatic and asymptomatic contacts. | Critical for identifying pre-symptomatic transmission [2]. |
| Rapid Antigen Tests (RAT) | Diagnostic Tool | Faster, decentralized testing; useful for frequent screening. | Lower sensitivity, especially in asymptomatic individuals [23]. |
| Structured Interview Protocols | Operational Tool | Systematic questionnaire to identify contacts and potential exposure events. | Aids in recall and standardized data collection [11]. |
The comparative analysis reveals that cluster tracing consistently outperforms forward tracing in reducing overall disease transmission across most scenarios, particularly when case ascertainment is low and contacts are quarantined [9]. Its strength lies in identifying the source of infection and multiple cases from a common exposure event, making it exceptionally effective at containing outbreaks driven by superspreading.
However, the optimal approach is not a choice of one over the other but their strategic integration. Effective systems combine methods: using forward tracing to break immediate chains of transmission from known cases, while simultaneously employing cluster tracing to uncover and contain the source of outbreaks [11] [10]. The success of either method is contingent on a supportive ecosystem that includes high case-ascertainment, timely testing, effective quarantine support, and—crucially—a robust, well-trained workforce and strong community trust [11] [1]. For future preparedness, developing flexible contact tracing systems capable of switching strategies based on resource availability and evolving disease dynamics is paramount [9].
Validation of transmission clusters is a cornerstone of effective epidemic control, serving as a critical feedback mechanism to confirm the accuracy of contact tracing efforts and refine public health interventions. During the COVID-19 pandemic, countries in East and Southeast Asia demonstrated remarkable proficiency in controlling transmission through sophisticated contact tracing systems that integrated robust validation of identified clusters [11]. This guide objectively compares the contact tracing systems of Japan, Thailand, Singapore, and Vietnam—nations recognized for their successful containment of COVID-19 through effective cluster validation [11] [92]. The analysis is framed within the broader context of transmission cluster validation research, providing researchers, scientists, and drug development professionals with detailed methodologies, performance metrics, and practical frameworks applicable to infectious disease surveillance and intervention studies. By examining both the technical and operational aspects of these systems, this guide aims to distill transferable principles for validating transmission clusters in diverse public health and research contexts.
Comparative Analysis of National Contact Tracing Systems
The contact tracing systems of Japan, Thailand, Singapore, and Vietnam shared common objectives but employed distinct operational approaches, organizational structures, and technological solutions tailored to their specific administrative contexts and resources. The comparative effectiveness of these systems hinged on their ability to accurately identify and validate transmission clusters through a combination of epidemiological investigation, technological augmentation, and coordinated public health response [11].
Table 1: Comparative Overview of National Contact Tracing Systems
| Country | Operational Structure | Primary Tracing Methods | Key Digital Tools | Contact Management Approach |
|---|---|---|---|---|
| Japan | Decentralized: Public Health Centers (PHCs) | Multi-faceted: Direct contacts, Backward Tracing | COCOA (Bluetooth app) | General: Close contacts for self-isolation and monitoring |
| Thailand | Decentralized: Local CDC investigation teams | Multi-faceted: Direct contacts, Source Case Investigation, Active Case Finding | DDC Care, MorChana, Thai Chana | Categorized: High-risk for isolation/quarantine, Low-risk for self-monitoring |
| Singapore | Centralized: Ministry of Health | Multi-faceted: Direct contacts, Source and Cluster Investigations | TraceTogether, SafeEntry | Categorized: Close contacts for designated quarantine, Transient contacts under phone surveillance |
| Vietnam | Decentralized: Local CDCs | Multi-faceted: Direct contacts, Source and Cluster Investigations, Generations | NCOVI, Bluezone | Categorized: F1 contacts for facility quarantine, F2 contacts for home quarantine |
Table 2: Performance and Validation Metrics in Selected Asian Countries
| Country | Key Validation Strengths | Epidemiological Impact | Technical Adaptation |
|---|---|---|---|
| Japan | Backward tracing identified superspreading events and 3Cs (closed spaces, crowded places, close-contact) | Crucial for sustained control during early pandemic | Bluetooth-based proximity tracking integrated with manual tracing |
| Thailand | Integration of >1 million village health volunteers for community-level verification | Effective case identification and cluster containment in diverse settings | GPS and Bluetooth applications with business safety protocol assessment |
| Singapore | Centralized coordination enabled real-time validation and policy adaptation | High accuracy in cluster identification and containment | Bluetooth and check-in/check-out systems with portable devices for inclusivity |
| Vietnam | Generational contact mapping (F1, F2) enabled multi-layer cluster validation | Successful containment of community clusters despite resource constraints | Digital tools complemented by extensive manual tracing efforts |
The foundational effectiveness of these systems stemmed from their balance across three core elements: speed (minimizing time from case identification to contact quarantine), capture (proportion of total contacts identified), and accuracy (correct classification of infection risk) [11]. Systems that maintained equilibrium among these elements while adapting to evolving epidemiology demonstrated superior performance in cluster validation and outbreak control [11].
Experimental Protocols and Methodologies
Prospective Space-Time Scan Statistical Analysis
Objective: To detect emerging space-time clusters of COVID-19 transmission and validate the effectiveness of public health interventions through statistical analysis of spatiotemporal patterns [93].
Methodology Overview:
- Data Collection: District-level daily new COVID-19 cases were collected from June 1 to October 31, 2021, across seven Southeast Asian countries (Indonesia, Malaysia, Philippines, Singapore, Thailand, Vietnam, Brunei) along with corresponding population data [93].
- Statistical Analysis: Prospective space-time scan statistics were employed to identify significant space-time clusters using SaTScan software. The analysis used a discrete Poisson model with the following parameters:
- Maximum spatial cluster size: 50% of the population at risk
- Maximum temporal cluster size: 50% of the study period
- Number of Monte Carlo replications: 999 for significance testing
- Risk Calculation: The relative risk (RR) for each identified cluster was calculated, representing the elevated risk of COVID-19 inside versus outside the cluster. Cumulative prospective analyses were performed at half-month intervals to track risk evolution [93].
- Intervention Linkage: Identified clusters and their risk trajectories were correlated with the timing and stringency of non-pharmaceutical interventions (NPIs) implemented in corresponding regions, allowing for assessment of intervention effectiveness [93].
Key Findings: The analysis identified seven significant high-risk clusters across Malaysia, Philippines, Thailand, Vietnam, and Indonesia between June and August 2021, with relative risks ranging from 1.36 to 5.62 (all P<.001) [93]. The study demonstrated that continuous strict interventions effectively mitigated COVID-19 risk (e.g., 34 Indonesian provinces showed risk reduction between -0.05 to -1.46), while relaxed restrictions frequently preceded increased transmission risk (58.6% of districts in Malaysia, Singapore, Thailand, and Philippines showed increasing infection risk following restriction easing) [93].
Multi-faceted Contact Tracing with Backward Tracing (Japan)
Objective: To identify transmission clusters through a combination of forward and backward tracing approaches, with particular emphasis on identifying superspreading events [11].
Methodology Overview:
- Implementation Structure: Decentralized operations through local Public Health Centers (PHCs) staffed by public health doctors, nurses, and specialists [11].
- Forward Tracing: Standard identification and monitoring of individuals exposed to known cases.
- Backward Tracing: Systematic investigation to identify the source of infection for detected cases, focusing on reconstructing transmission networks.
- Cluster Analysis: Aggregated tracing data was analyzed to identify common environmental factors associated with clusters, leading to the formulation of the "3Cs" public health message (avoiding closed spaces, crowded places, and close-contact settings) [11].
- Digital Enhancement: The COCOA Bluetooth-based application notified users of potential exposure to facilitate testing and isolation [11].
Validation Mechanism: Backward tracing served as a critical validation mechanism by confirming or refuting hypothesized transmission linkages and identifying previously unrecognized transmission settings. This approach proved particularly valuable for detecting superspreading events that accounted for disproportionate transmission [11].
Integrated Community-Based Surveillance (Thailand)
Objective: To validate transmission clusters through a multi-layered tracing approach that combined specialized investigation teams with community-based health volunteers [11].
Methodology Overview:
- Operational Structure: The system was coordinated by the Department of Disease Control, supported by regional health offices, and implemented through more than 1,000 local investigation teams [11].
- Professional Tracing: Specialized teams conducted source case investigation and active case finding in identified transmission clusters.
- Community Integration: More than one million village health volunteers assisted in primary contact monitoring and provided community-level validation of transmission patterns [11].
- Digital Tools: Multiple applications supported different functions:
- DDC Care: Symptom monitoring for high-risk patients and contacts
- MorChana: GPS and Bluetooth-based contact identification
- Thai Chana: Business safety protocol assessment and contact tracing support [11]
- Legal Framework: The Communicable Diseases Act provided legislative support for investigation and response activities [11].
Validation Mechanism: The integration of professional epidemiological teams with community-based volunteers created a dual-layer validation system that combined technical expertise with local knowledge, enhancing the accuracy of cluster identification and verification.
System Workflows and Signaling Pathways
The validation of transmission clusters follows a systematic workflow that integrates data collection, analysis, and intervention. The following diagram illustrates the core process common to successful systems in the region, with variations specific to each country's operational approach:
Diagram 1: Transmission Cluster Validation Workflow (13 characters)
The signaling pathway between cluster validation and public health intervention represents a critical feedback loop in outbreak control. The following diagram illustrates how validated cluster data informs specific public health responses and generates evidence for system improvement:
Diagram 2: Intervention Signaling Pathway (12 characters)
Table 3: Research Reagent Solutions for Transmission Cluster Validation
| Tool/Resource | Primary Function | Application Context | Key Features |
|---|---|---|---|
| Prospective Space-Time Scan Statistics | Detection of emerging space-time clusters | Early outbreak detection, intervention effectiveness assessment | Identifies statistically significant clusters, calculates relative risk, monitors temporal evolution [93] |
| Backward Tracing Protocols | Reconstruction of transmission networks | Identification of superspreading events, transmission settings | Reveals infection sources, identifies common exposure venues, validates forward tracing [11] |
| Digital Proximity Tracking Tools | Automated contact identification | High-population density settings, real-time exposure notification | Bluetooth/GPS functionality, privacy-preserving design, integration with manual systems [11] |
| Multi-Layer Contact Categorization | Risk-based resource allocation | Prioritization of high-risk contacts, efficient resource deployment | F1/F2 classification system, differentiated quarantine protocols, focused monitoring [11] |
| Dynamic Surveillance Metrics | Real-time transmission assessment | Outbreak status determination, policy adjustment guidance | Speed, acceleration, jerk measurements, outbreak threshold calibration [94] |
| Genomic Sequencing Integration | Variant-specific transmission mapping | Variant characterization, transmission chain confirmation | Identification of variants of concern, linkage of cases with molecular evidence [94] |
The case studies from Japan, Thailand, Singapore, and Vietnam demonstrate that successful validation of transmission clusters depends on integrating multiple complementary methodologies within adaptable operational frameworks. These systems shared common success factors: balancing speed, capture, and accuracy; combining technological solutions with human expertise; implementing multi-layered validation approaches; and maintaining flexibility to adapt to local contexts and evolving epidemiology [11].
For researchers and public health professionals, these findings highlight that effective cluster validation requires both technical sophistication and operational pragmatism. The experimental protocols and analytical tools detailed in this guide provide evidence-based methodologies that can be adapted to diverse research and public health contexts, with particular relevance for ongoing infectious disease surveillance, outbreak investigation, and pandemic preparedness planning. As infectious disease threats continue to evolve, the principles derived from these successful Asian systems offer valuable guidance for developing robust validation frameworks capable of interrupting transmission chains and mitigating future outbreaks.
In infectious disease epidemiology, the reproduction number (R) serves as a fundamental metric for quantifying the transmissibility of a pathogen and the effectiveness of intervention strategies. The basic reproduction number (R0) represents the average number of secondary infections generated by a single infectious individual in a fully susceptible population, while the effective reproduction number (Rt) reflects real-time transmission dynamics under existing control measures [95] [96]. Achieving an Rt value below 1.0 is critical for outbreak containment, as it indicates that each infected individual transmits the infection to fewer than one person on average, ultimately leading to epidemic decline [95] [96]. This analysis quantitatively compares how different contact tracing methodologies and complementary interventions reduce reproduction numbers and increase outbreak containment rates, providing researchers and public health professionals with evidence-based guidance for optimizing pandemic response strategies.
The validation of transmission clusters through contact tracing research provides the essential framework for accurately estimating reproduction number reductions. As [97] elucidates, the "apparent reproduction number" calculated from surveillance data often differs from the true reproduction number due to surveillance delays and incomplete detection. Sophisticated contact tracing systems that incorporate exposure settings, genomic validation, and network analysis significantly enhance the accuracy of these estimates, enabling more precise quantification of intervention impacts [13] [97]. Within this context, we systematically evaluate the performance of various contact tracing approaches and their measurable effects on disease transmission dynamics.
Comparative Effectiveness of Contact Tracing Methodologies
Quantitative Comparison of Contact Tracing Methods
Table 1: Effectiveness and Cost-Efficiency of Contact Tracing Methods Across Scenarios
| Tracing Method | Scenario | Transmission Reduction | Provider Cost per Infection Prevented (USD) | Key Applications |
|---|---|---|---|---|
| Cluster Tracing | Low case-ascertainment with testing | 22% | $2,943.56 - $5,226.82 | Early outbreak detection; super-spreader events |
| Extended Tracing | Low case-ascertainment with testing | 18% | - | Settings with high pre-symptomatic transmission |
| Forward Tracing | Low case-ascertainment with testing | 12% | - | Resource-limited settings; established transmission chains |
| Cluster Tracing | Low case-ascertainment with quarantine | 62% | <$4,000 | High-risk settings; variant emergence |
| Extended Tracing | Low case-ascertainment with quarantine | 50% | - | Linked to index case with prolonged infectious period |
| Forward Tracing | Low case-ascertainment with quarantine | 46% | - | Standard public health response |
| All Methods | High case-ascertainment with quarantine | Brings R below 1.0 | <$800 | Outbreak control; pandemic containment |
Source: Adapted from [9]
The comparative effectiveness of contact tracing methods varies significantly depending on implementation context and available resources. As demonstrated in Table 1, cluster tracing emerges as the most effective approach across multiple scenarios, particularly when combined with quarantine measures, achieving transmission reductions of up to 62% [9]. This method combines forward tracing with cluster identification, enabling public health teams to identify and contain super-spreading events more efficiently. The superiority of cluster tracing aligns with findings from England's enhanced contact tracing programme, which demonstrated that exposure clusters occurring in workplaces and educational settings were most strongly associated with genetically validated transmission events (workplaces: aOR = 5.10, 95% CI 4.23–6.17; education: aOR = 3.72, 95% CI 3.08–4.49) [13].
The integration of high case-ascertainment rates with quarantine of contacts represents the optimal scenario for contact tracing effectiveness, bringing reproduction numbers below unity and stopping disease transmission early [9]. This combination addresses two critical factors in transmission dynamics: identifying a sufficient proportion of infected individuals and effectively preventing onward transmission through isolation. Under these conditions, all tracing methods perform effectively, highlighting the importance of comprehensive testing and supportive isolation policies as foundational components of successful contact tracing programmes [9] [98].
Experimental Protocols for Contact Tracing Assessment
Standardized Evaluation Framework for Contact Tracing Operations Research assessing contact tracing effectiveness typically employs transmission network models constructed from comprehensive contact tracing data. The protocol implemented in Singapore's population structure exemplifies a rigorous approach to comparing tracing methods [9]:
Data Collection: Compile complete contact tracing records including symptom onset dates, exposure settings, and demographic information for both index cases and contacts.
Scenario Definition: Establish four operational scenarios reflecting variable real-world conditions: (1) low case-ascertainment with testing of contacts; (2) low case-ascertainment with quarantine of contacts; (3) high case-ascertainment with testing of contacts; and (4) high case-ascertainment with quarantine of contacts.
Method Implementation:
- Forward Tracing: Identify and monitor contacts exposed from 2 days before case isolation
- Extended Tracing: Expand the tracing window to cover 16 days before case isolation
- Cluster Tracing: Combine forward tracing with systematic cluster identification through exposure setting analysis
Outcome Measurement: Quantify transmission reduction through comparison of observed reproduction numbers against baseline scenarios without interventions, while simultaneously tracking resource utilization and costs.
Genomic Validation of Transmission Clusters The England enhanced contact tracing programme developed a protocol for algorithmically identifying and validating exposure clusters [13]:
Exposure Data Collection: During routine contact tracing, systematically collect data on cases' exposures during the pre-symptomatic period (3-7 days before symptom onset).
Cluster Identification: Algorithmically match ≥2 cases reporting the same event location (postcode) and category within a 7-day rolling window.
Genetic Validation: Compare viral sequences from different households within exposure clusters; define genetic validity as ≥2 cases with identical sequences.
Operational Timeliness Assessment: Compare identification dates between algorithm-detected clusters and traditionally reported incidents in the national incident management system.
This protocol enabled the identification of 269,470 exposure clusters, with 25% genetically validated, and demonstrated that 81% of validated clusters were not recorded in traditional surveillance systems, highlighting the superior sensitivity of systematic exposure cluster analysis [13].
Reproduction Number Reductions Across Interventions and Settings
Quantitative Impact of Contact Tracing on Reproduction Numbers
Table 2: Reproduction Number Reductions from Contact Tracing and Complementary Interventions
| Intervention Type | Setting/Study | Initial R0 | Post-Intervention Rt | Reduction Magnitude | Key Success Factors |
|---|---|---|---|---|---|
| Comprehensive NPIs | European Union (Early 2020) | 4.22 (±1.69) | 0.67 (±0.18) | 84% | Air travel reduction; mobility restrictions; 17-day delay for effect |
| Well-Implemented Contact Tracing | Modelling Study (UK) | - | - | 10-15% | 80% contact coverage; good adherence; fast testing |
| Optimized Test & Trace | Modelling Study (UK) | 2.2 | 0.57 | 74% | Prompt tracing (<2-3 days); >80% contacts quarantined |
| Cluster Surveillance | England (2020-2021) | - | - | - | Exposure setting identification; genomic validation |
| Bidirectional Tracing | Multiple Settings | - | - | 20-26% | High case-ascertainment; testing of contacts |
Sources: Adapted from [95] [98] [73]
The quantitative impact of contact tracing on reproduction numbers varies significantly based on implementation quality and complementary interventions. As shown in Table 2, modelling studies consistently demonstrate that under optimal conditions of prompt and thorough tracing with effective quarantine, contact tracing can reduce reproduction numbers from 2.2 to 0.57—a 74% reduction sufficient to stop epidemic growth [98]. However, real-world implementation often falls short of these ideal conditions. The UK's NHS Test and Trace programme, for instance, was estimated to reduce the reproduction number by only 2-5% in October 2020, with improved scenarios projecting reductions of 6-13% even with 80% of contacts traced [73].
The integration of contact tracing with broader non-pharmaceutical interventions (NPIs) generates substantially greater reductions in transmission metrics. During the early COVID-19 pandemic in Europe, comprehensive measures including travel restrictions, mobility limitations, and lockdowns reduced reproduction numbers from 4.22 to 0.67, representing an 84% reduction in transmission potential [95]. The correlation between mobility indicators (air travel, driving, transit) and reproduction numbers demonstrated a consistent time delay of approximately 17 days between implementation and observable effect, highlighting the importance of sustained intervention periods for accurate impact assessment [95].
Methodological Protocols for Reproduction Number Estimation
Time-Varying Reproduction Number Estimation The dynamic SEIR model with machine learning integration provides a robust methodology for estimating time-varying reproduction numbers [95]:
Model Structure: Implement a Susceptible-Exposed-Infectious-Recovered (SEIR) compartmental framework with time-varying parameters:
dS/dt = -β(t)SI/NdE/dt = β(t)SI/N - αEdI/dt = αE - γIdR/dt = γIWhere β(t) represents the time-varying contact rate, α the latency rate (inverse of latent period), and γ the infectious rate (inverse of infectious period).
Reproduction Number Parameterization: Express the time-varying contact rate as β(t) = R(t)/C, where C represents the infectious period, enabling direct estimation of R(t).
Transition Function: Model the smooth transition from initial to current reproduction number using a hyperbolic tangent function:
R(t) = R0 - 0.5[1 + tanh((t-t*)/T)][R0 - Rt]Where t* represents the adaptation time and T the transition time.Parameter Estimation: Apply Bayesian inference with Markov Chain Monte Carlo methods to estimate parameters ϑ = {E0, I0, σ, R0, Rt, t*, T}, accounting for uncertainties in initial conditions and model fit.
Comparative Method Assessment for R0 Estimation A comprehensive study from Iran compared five distinct methodological approaches for estimating R0, using the root mean square error (RMSE) to evaluate model performance [99]:
Exponential Growth (EG) Method: Estimates R0 from the initial growth rate of cases using the formula
R = 1/M(-r), where r represents the growth rate and M the moment generating function of the generation time distribution.Maximum Likelihood (ML) Method: Maximizes the log-likelihood function
LLR = Σ[exp(-μt)μt^Nt/Nt!]whereμt = RΣNt-iwito identify the R0 value that best explains the observed incidence pattern.Time-Dependent (TD) Method: Computes
Rt = 1/NtΣRj, where Rj represents the average reproduction number across transmission networks, providing time-varying estimates.Sequential Bayesian (SB) Method: Applies Bayesian updating with non-informative priors to generate posterior distributions for R0 across sequential time periods.
Attack Rate (AR) Method: Calculates R0 from the final attack rate using the formula
R0 = log(1-AR/S0)/(AR-1-S0), where AR represents the infection ratio and S0 the initial susceptible proportion.
This methodological comparison determined that the Time-Dependent approach provided the best fit to empirical data, with the lowest RMSE values, while the Exponential Growth and Maximum Likelihood methods tended to overestimate R0, and the Sequential Bayesian method demonstrated under-fitting characteristics [99].
Visualization of Contact Tracing Impact Pathways
Transmission Interruption Pathways
This pathway visualization illustrates how different contact tracing methodologies and implementation factors influence reproduction number reductions. The diagram highlights the superior effectiveness of cluster tracing approaches and demonstrates how optimized implementation with high adherence and effective testing can achieve substantially greater transmission reduction (10-74%) compared to basic implementation (2-15%).
Reproduction Number Estimation Workflow
This workflow delineates the methodological process for estimating and validating reproduction numbers, highlighting the comparative performance of different estimation approaches. The visualization incorporates empirical R0 values from Iran's early COVID-19 outbreak [99], demonstrating how the Time-Dependent method emerged as the best-fitting approach based on root mean square error comparison.
The Researcher's Toolkit: Essential Materials and Reagents
Table 3: Essential Research Reagents and Computational Tools for Transmission Analysis
| Tool Category | Specific Solution | Research Application | Key Parameters |
|---|---|---|---|
| Epidemiological Modeling | Dynamic SEIR Framework | Reproduction number estimation | Time-varying β; Latency rate α; Infectious rate γ |
| Statistical Packages | R0 Package (R) | Exponential growth & maximum likelihood estimation | Serial interval distribution; Growth rate estimation |
| Network Analysis | Transmission Network Models | Cluster identification; Super-spreader detection | Node degree; Network density; Connectivity |
| Genomic Sequencing | Whole Genome Sequencing | Transmission cluster validation | Single nucleotide variants; Phylogenetic relationships |
| Bayesian Inference | Markov Chain Monte Carlo (MCMC) | Parameter estimation with uncertainty quantification | Prior distributions; Posterior sampling; Convergence diagnostics |
| Data Integration | Geographic Information Systems (QGIS) | Spatial analysis of transmission patterns | Case clustering; Mobility correlations; Hotspot identification |
Sources: Adapted from [95] [100] [96]
The research reagents and computational tools outlined in Table 3 represent essential components for conducting robust transmission dynamics analysis and contact tracing evaluation. The dynamic SEIR modeling framework enables researchers to incorporate time-varying parameters and estimate reproduction number reductions with appropriate uncertainty quantification [95]. Specialized statistical packages, such as the R0 package in R, provide implemented methods for exponential growth rate and maximum likelihood estimation of reproduction numbers, incorporating appropriate serial interval distributions that function as critical parameters in these analyses [96] [99].
Network analysis tools applied to contact tracing data enable the identification of transmission patterns across demographic groups, geographic regions, and occupational settings. As demonstrated in Cyprus's comprehensive analysis of over 20,000 cases, network epidemiology can reveal shifting transmission dynamics across pandemic waves, highlighting distinctive patterns by age group and identifying vulnerable occupational sectors [100]. The integration of genomic sequencing provides crucial validation for transmission clusters identified through epidemiological methods, with England's programme demonstrating that 25% of algorithmically-identified exposure clusters represented genetically validated transmission events [13].
Discussion: Synthesis and Research Implications
The quantitative evidence synthesized in this analysis demonstrates that well-implemented contact tracing programmes can contribute meaningfully to reducing reproduction numbers and containing outbreaks, though typically as part of comprehensive intervention strategies rather than standalone solutions. The maximum realistically achievable reproduction number reduction from contact tracing alone appears to be approximately 10-15% under optimal conditions of high coverage, rapid execution, and good population adherence [73]. However, when integrated with complementary measures such as travel restrictions, mobility limitations, and venue closures, reproduction number reductions exceeding 80% are achievable, as demonstrated by the European experience of reducing R0 from 4.22 to 0.67 [95].
Methodologically, the accurate quantification of intervention impacts requires sophisticated modeling approaches that account for the inherent limitations of surveillance systems. As [97] emphasizes, the "apparent reproduction number" calculated from empirical case data often diverges from the true reproduction number due to surveillance delays and incomplete detection. Future research should prioritize the development and validation of adjustment methods that correct for these systematic biases, potentially through the integration of representative seroprevalence studies or wastewater surveillance data that provide more population-representative transmission indicators.
The systematic evaluation of contact tracing methods across diverse implementation contexts reveals that optimal approaches depend critically on local transmission dynamics, available resources, and population characteristics. Cluster tracing methods consistently demonstrate superior effectiveness, particularly when targeting settings with documented super-spreading potential such as workplaces and educational institutions [9] [13]. However, simpler forward tracing approaches may represent the most efficient option in resource-limited settings or when case ascertainment rates are high. This contextual dependence underscores the importance of flexible, adaptable contact tracing systems capable of implementing different methodologies based on evolving epidemic conditions and operational constraints [9].
For researchers and public health professionals developing pandemic preparedness plans, these findings highlight several critical priorities: First, establishing pre-approved protocols for rapid contact tracing implementation with clear thresholds for escalating between different methodological approaches. Second, investing in the technological infrastructure and trained personnel necessary for sophisticated approaches like cluster tracing and genomic validation. Third, developing comprehensive strategies to support adherence to isolation recommendations, as even the most perfectly designed contact tracing system depends on population cooperation for ultimate effectiveness [73]. Through continued refinement of these methodologies and their contextual application, the global public health community can enhance its capacity to rapidly detect and contain emerging infectious disease threats.
Conclusion
Validating transmission clusters through integrated contact tracing and molecular analysis provides a powerful approach for understanding and interrupting disease spread. Key lessons emphasize that successful cluster detection requires balancing speed, accuracy, and resource allocation while adapting strategies to specific outbreak contexts. Molecular methods objectively identify transmission links that traditional approaches may miss, while epidemiological data provides crucial context for genetic findings. Future directions should focus on developing standardized validation metrics, creating flexible response frameworks that can scale during epidemics, and advancing real-time data integration platforms. These enhancements will strengthen pandemic preparedness, enable more targeted interventions, and optimize public health resource deployment for emerging pathogens.
References
- 1. Contact tracing strategies for infectious diseases: A systematic ... [https://journals.plos.org/globalpublichealth/article?id=10.1371/journal.pgph.0004579]
- 2. Empirical evidence on the efficiency of backward contact ... [https://www.nature.com/articles/s41467-022-32531-6]
- 3. Principles of Epidemiology: Glossary [https://archive.cdc.gov/www_cdc_gov/csels/dsepd/ss1978/glossary.html]
- 4. Epidemic thresholds in dynamic contact networks - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2659580/]
- 5. Toward epidemic thresholds on temporal networks: a review ... [https://appliednetsci.springeropen.com/articles/10.1007/s41109-019-0230-4]
- 6. A novel methodology for assessing contact tracing precision [https://pubmed.ncbi.nlm.nih.gov/41101737/]
- 7. Models of epidemics: when contact repetition and clustering ... [https://tbiomed.biomedcentral.com/articles/10.1186/1742-4682-6-11]
- 8. Phylogenetic validation of a contact tracing program for ... [https://www.sciencedirect.com/science/article/abs/pii/S0166093425001727]
- 9. Comparison of contact tracing methods: A modelling study [https://www.sciencedirect.com/science/article/pii/S2468042725000399]
- 10. Comparative effectiveness of contact tracing interventions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9932408/]
- 11. Lessons for future outbreaks from successful contact tracing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12134535/]
- 12. Automatic case cluster detection using hospital electronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10067150/]
- 13. COVID-19 cluster surveillance using exposure data collected ... [https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000485]
- 14. Genotyped cluster investigations versus standard contact ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-10358-4]
- 15. Nationwide rollout reveals efficacy of epidemic control ... [https://www.nature.com/articles/s41467-021-26144-8]
- 16. SLEDgeHammer: A Frequent Pattern-Based Cluster ... [https://www.mdpi.com/2227-7390/13/17/2832]
- 17. Cluster Analysis: Definition and Examples [https://www.qualtrics.com/articles/strategy-research/cluster-analysis/]
- 18. Differences in the superspreading potentials of COVID-19 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9744370/]
- 19. Investigating setting-specific superspreading potential and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12215501/]
- 20. Clustering and superspreading potential of SARS-CoV-2 ... [https://www.nature.com/articles/s41591-020-1092-0]
- 21. Comprehensive Guide to Cluster Analysis [https://www.displayr.com/understanding-cluster-analysis-a-comprehensive-guide/]
- 22. Genomic epidemiology offers high resolution estimates of ... [https://www.nature.com/articles/s41467-023-40544-y]
- 23. quantifying the performance of contact tracing in the United ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10274953/]
- 24. Estimates of serial interval for COVID-19: A systematic review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7448781/]
- 25. Mining relationships between transmission clusters from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8499889/]
- 26. Surveillance and Epidemiology of Infectious Diseases using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7120538/]
- 27. Methods for molecular transmission cluster detection [https://virological.org/t/methods-for-molecular-transmission-cluster-detection/934]
- 28. Empirical comparison of analytical approaches for ... [https://www.nature.com/articles/s41598-020-75560-1]
- 29. Inferring putative transmission clusters with Phydelity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6785678/]
- 30. Mathematical Contact Tracing Models for the COVID-19 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12026787/]
- 31. Novel insights on unraveling dynamics of transmission ... [https://www.sciencedirect.com/science/article/pii/S1567134824001126]
- 32. Empirical evidence on the efficiency of backward contact ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9375086/]
- 33. Bidirectional contact tracing could dramatically improve ... [https://www.nature.com/articles/s41467-020-20325-7]
- 34. Molecular network analysis for detecting HIV transmission ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1429464/full]
- 35. A comparison of phylogenetic and distance-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10599596/]
- 36. Common Methods for Phylogenetic Tree Construction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11117635/]
- 37. Phylogenetic Tree Construction Methods | Guide to ... [https://go.zageno.com/blog/guide-to-the-different-methods-of-phylogenetic-tree-construction]
- 38. Molecular cluster, transmission characteristics, origin and ... [https://www.sciencedirect.com/science/article/pii/S0001706X2400278X]
- 39. A survey of current software for network analysis in molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3500165/]
- 40. Software & Platforms [https://idekerlab.ucsd.edu/software/]
- 41. Build Phylogenetic Trees [https://www.geneious.com/tutorials/phylogenetic-trees]
- 42. A Brief History of Exposure Notification During the COVID-19 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9357651/]
- 43. 大模型赋能的云原生应用安全平台-汉为软件NovaGuard - AWS [https://aws.amazon.com/cn/blogs/china/large-language-model-enabled-cloud-native-application-security-platform-hanwei-software-novaguard/]
- 44. COVID-19接触者追踪应用程序的隐私研究 [https://www.anquanke.com/post/id/216683]
- 45. 调试、分析和部署状态数据收集| Apigee [https://cloud.google.com/apigee/docs/hybrid/v1.9/other-data-collection?hl=zh-cn]
- 46. 新冠肺炎疫情下接触者追踪的隐私风险及保护 [https://m.fx361.com/news/2021/1026/12581551.html]
- 47. Digital Exposure Notification Tools: A Global Landscape ... [https://www.medrxiv.org/content/10.1101/2022.06.02.22275925v1.full-text]
- 48. Exposure notification system activity as a leading indicator for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0287368]
- 49. 超级全面的数据库开启API解决方案,收藏!一步搞定集成与 ... [https://www.fanruan.com/blog/article/1793124/]
- 50. Defining HIV-1 transmission clusters based on sequence data [https://pmc.ncbi.nlm.nih.gov/articles/PMC5482559/]
- 51. Nationwide Implementation of HIV Molecular Cluster ... [https://wwwnc.cdc.gov/eid/article/31/13/24-1143_article]
- 52. Threshold sensitivity analysis for HIV-1 transmission cluster ... [https://www.sciencedirect.com/science/article/abs/pii/S0042682225001710]
- 53. Prediction of HIV Transmission Cluster Growth with Statewide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6692892/]
- 54. T-shaped alignments integrating HIV-1 near full-length ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013676]
- 55. Identifying High-Risk Events for COVID-19 Transmission [https://pubmed.ncbi.nlm.nih.gov/36851670/]
- 56. Use of surveillance data to elucidate household of... clustering [https://pmc.ncbi.nlm.nih.gov/articles/PMC9536872/]
- 57. Monitoring and Understanding Household of... :: SSRN Clustering [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4095731]
- 58. Transmission of SARS-CoV-2 in the workplace [https://pmc.ncbi.nlm.nih.gov/articles/PMC10193509/]
- 59. (PDF) Household of transmission - COVID according to index 19 ... case [https://www.academia.edu/143890204/Household_transmission_of_COVID_19_according_to_index_case_children_parents_and_healthcare_workers]
- 60. Transmission of SARS-CoV-2: A Review of Viral, Host, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7505025/]
- 61. Effectiveness of digital contact tracing interventions for ... [https://www.sciencedirect.com/science/article/pii/S0033350625000927]
- 62. Intervention effect of targeted workplace closures may be ... [https://www.nature.com/articles/s41598-024-66741-3]
- 63. Clustering of countries according to the COVID-19 incidence ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-022-13086-z]
- 64. Mobile App-based contact Tracing During COVID-19— ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7811390/]
- 65. Autobiographical memory in contact tracing: evidence from ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2023.1244568/full]
- 66. Impact of delays on effectiveness of contact tracing strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7365652/]
- 67. Contact tracing efficiency, transmission heterogeneity, and ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1009122]
- 68. Optimizing the order of actions in a model of contact tracing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10013731/]
- 69. Contact tracing strategies for infectious diseases: A systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12063836/]
- 70. A novel approach to estimating Rt through infection networks [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1586786/full]
- 71. Characterising non-household contact patterns relevant to ... [https://www.sciencedirect.com/science/article/pii/S2589750025000706]
- 72. On the contact tracing for COVID-19: A simulation study [https://pmc.ncbi.nlm.nih.gov/articles/PMC10019035/]
- 73. Contact tracing is an imperfect tool for controlling COVID ... [https://www.nature.com/articles/s41467-021-25531-5]
- 74. Digital proximity tracing on empirical contact networks for ... [https://www.nature.com/articles/s41467-021-21809-w]
- 75. Mining relationships between transmission from clusters ... contact [https://pubmed.ncbi.nlm.nih.gov/34498059/]
- 76. Analysis of contact showed contribution of asymptomatic... tracing data [https://www.nature.com/articles/s41598-023-35622-6?error=cookies_not_supported&code=0a830aa3-8963-4309-9437-2001c02001ff]
- 77. Developing practical strategies to reduce addiction-related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11097512/]
- 78. Increasing opportunities for community input in harm reduction ... [https://harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-025-01323-8]
- 79. The EpiQuant Framework for Computing Epidemiological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5405252/]
- 80. Concordance between epidemiological evaluation of ... [https://www.sciencedirect.com/science/article/pii/S1198743X20302238]
- 81. Comparison of molecular surveillance methods to assess ... [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2023.1067966/full]
- 82. Concordance and discordance of sequence survey ... [https://peerj.com/articles/761/]
- 83. Cluster Validation Statistics: Must Know Methods - Datanovia [https://www.datanovia.com/en/lessons/cluster-validation-statistics-must-know-methods/]
- 84. A brief introduction to Cluster Validation | by Jonte Dancker [https://medium.com/@jodancker/a-brief-introduction-to-cluster-validation-ca4215295b06]
- 85. A mathematical model to assess the effectiveness of test-trace ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0299880]
- 86. Combining Mass Testing and Contact for Tracing Pandemic... Effective [https://scisimple.com/en/articles/2025-10-10-combining-mass-testing-and-contact-tracing-for-effective-pandemic-response--ak6jp2o]
- 87. A Framework for Using Cost-effectiveness Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12227514/]
- 88. Cost-Effectiveness Analysis of Branded Drugs With Market ... [https://www.sciencedirect.com/science/article/pii/S1098301521015783]
- 89. Mathematical Contact Tracing Models for the COVID-19 ... [https://www.mdpi.com/2227-9032/13/8/935]
- 90. Contact tracing as a measure to combat COVID-19 and ... [https://www.sciencedirect.com/science/article/pii/S0196655321007951]
- 91. A Cluster Analysis of the Acceptance of a Contact Tracing App ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9140954/]
- 92. Lessons for future outbreaks from successful contact ... [https://pubmed.ncbi.nlm.nih.gov/40470521/]
- 93. Prospective Space-Time Scan Statistical Analysis Method [https://publichealth.jmir.org/2022/8/e35840/]
- 94. Updated Surveillance Metrics and History of the COVID-19 ... [https://publichealth.jmir.org/2025/1/e53214]
- 95. The reproduction number of COVID-19 and its correlation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7359536/]
- 96. Comparison of the Basic Reproduction Numbers for COVID ... [https://www.mdpi.com/2673-8937/3/1/1]
- 97. Differences between the true reproduction number and ... [https://www.sciencedirect.com/science/article/pii/S1755436524000033]
- 98. Effective contact tracing for COVID-19: A systematic review [https://www.sciencedirect.com/science/article/pii/S2590113323000068]
- 99. Comparison of Different Approaches in Estimating Initial ... [https://brieflands.com/journals/jamm/articles/113224]
- 100. Network epidemiological analysis of COVID-19 ... [https://www.nature.com/articles/s41598-025-14267-7]